
作者/講者: 林廷遠 醫師
校稿: Ian YC Chen, MD
上次校閱: 2018/04/20

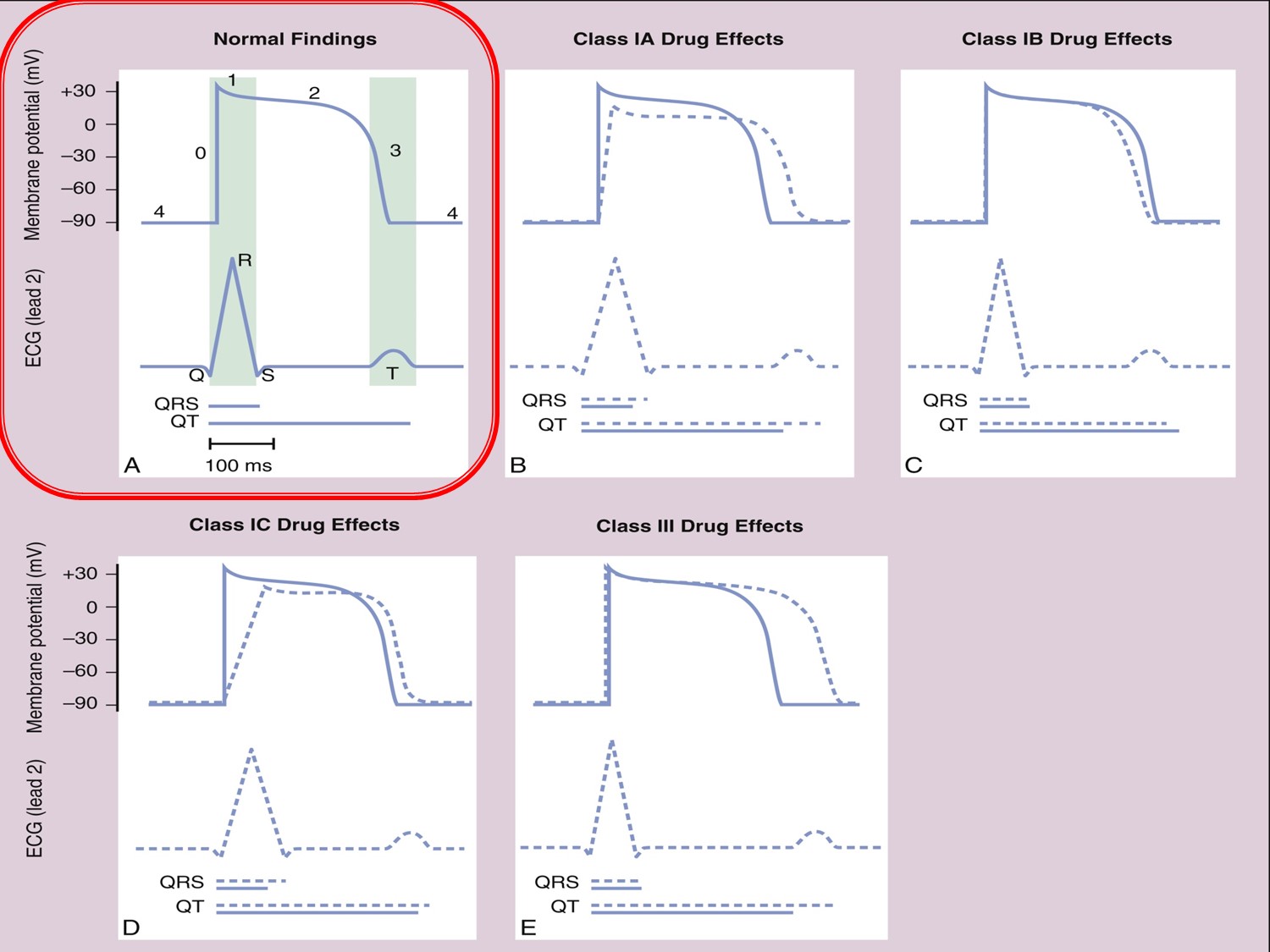
Phase 0:去極化
Phase 1:早期再極化
Phase 2:平原期再極化
Phase 3:快速再極化
Phase 4:緩慢去極化,接下一個action potential
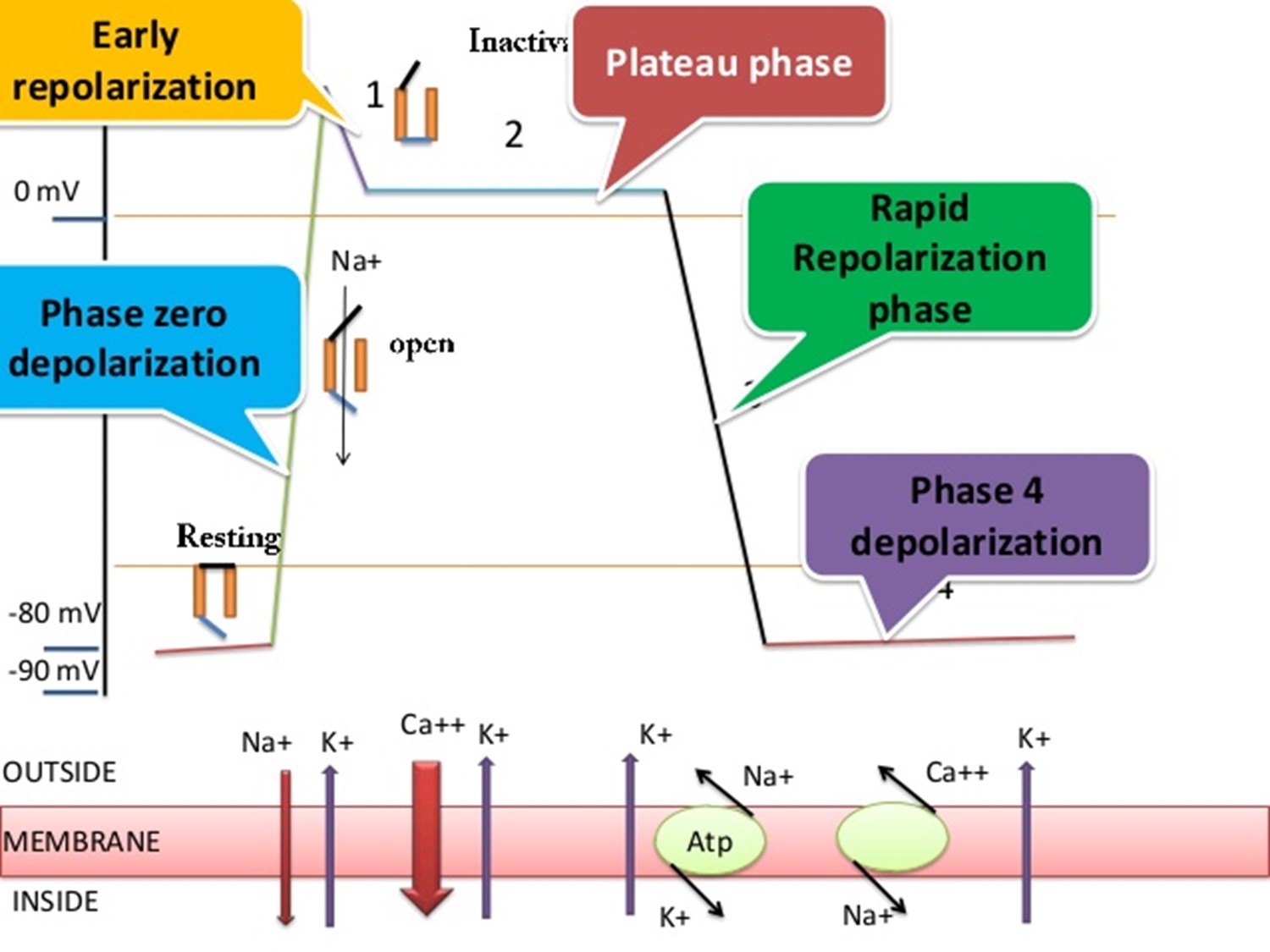
Phase 0:Na channel 打開,Na往細胞內流動
Phase 1:Na channel關閉
Phase 2:Ca進入細胞
Phase 3:K出去細胞
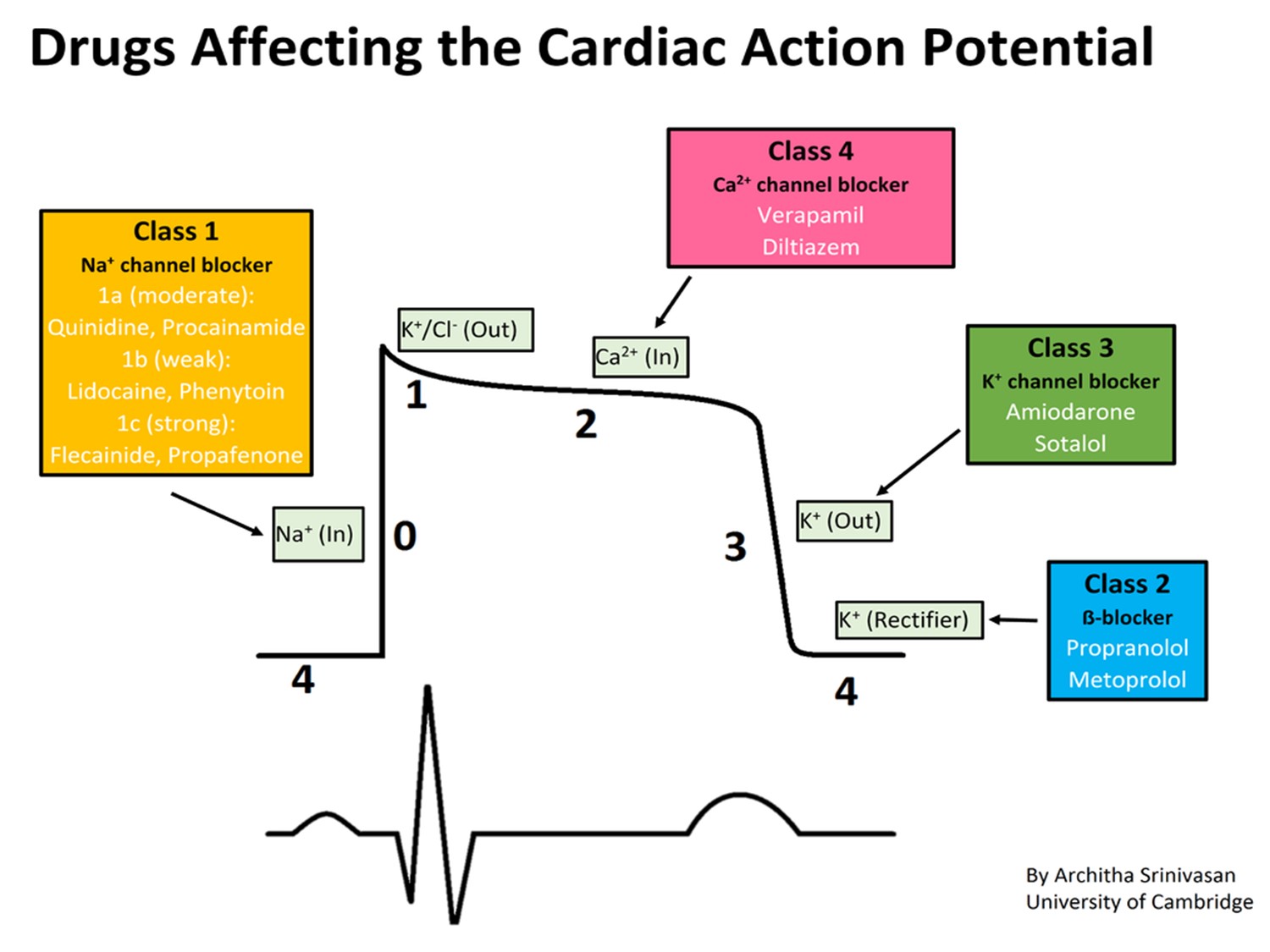
藥物作用時間
Class 1:0期
Class 2:4期
Class 3:3期
Class 4:2期
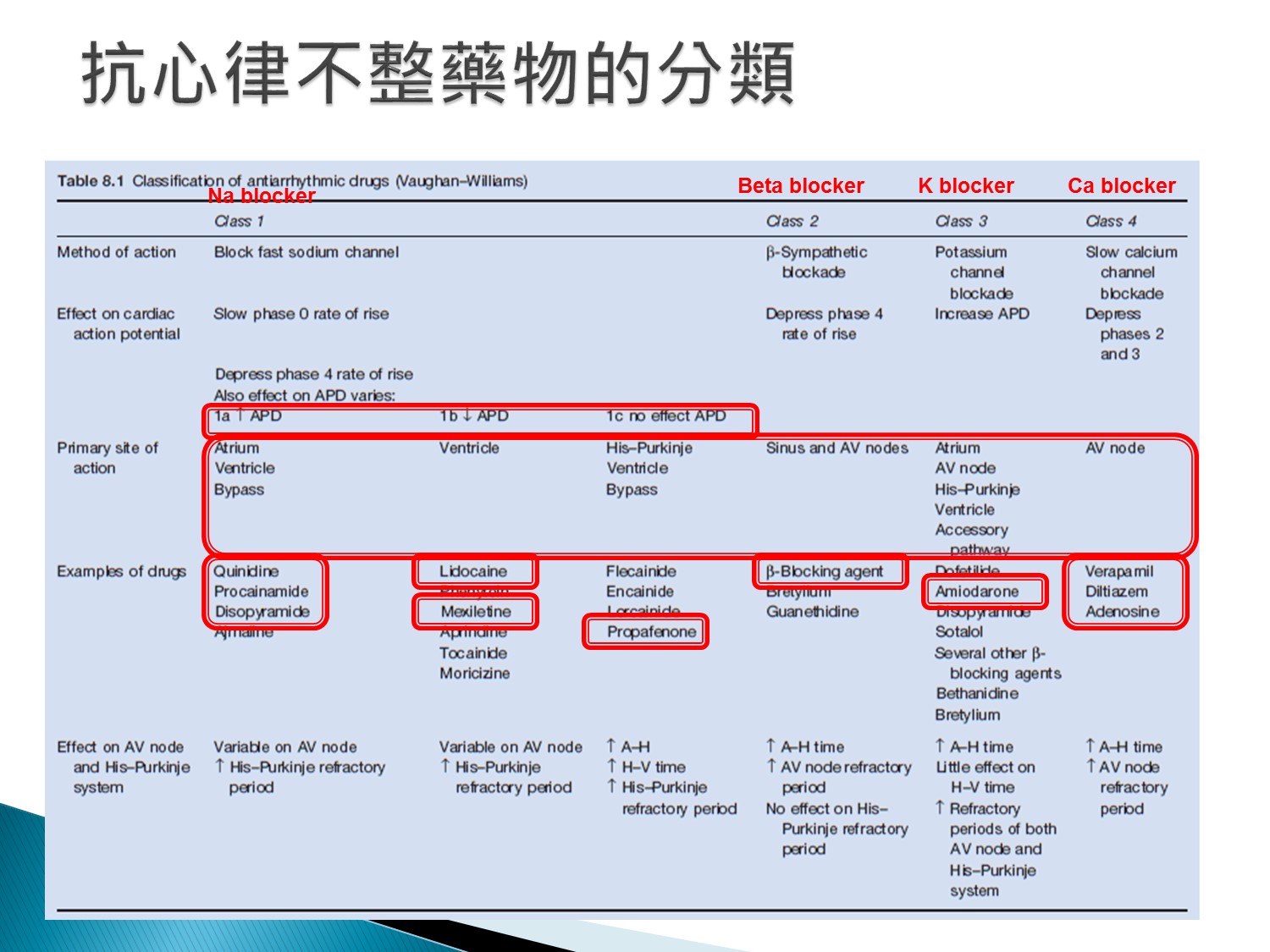
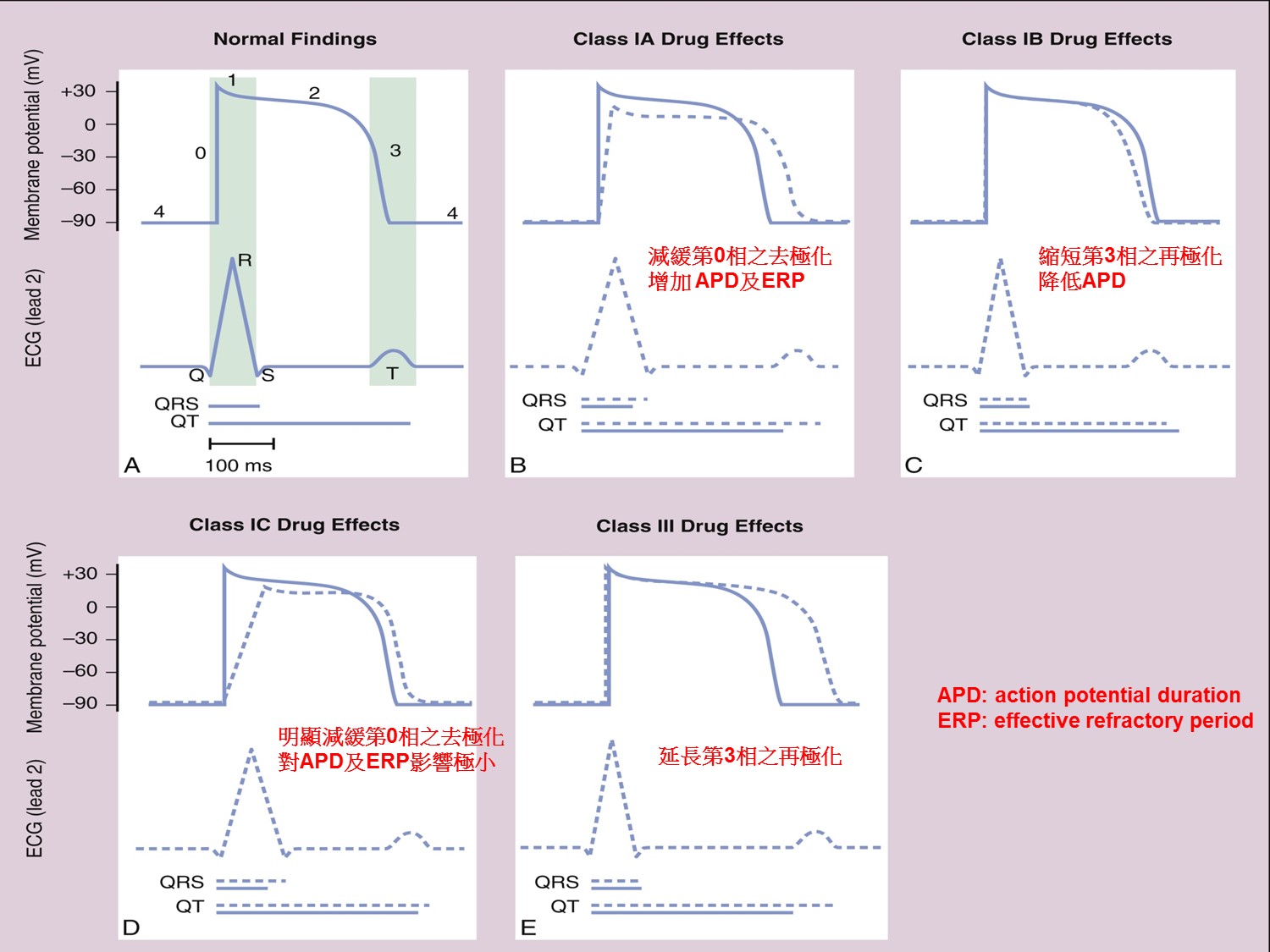
Ia:QRS延長、QT延長
Ib:QRS不變,QT縮短(可用在QT prolong者)
Ic:QRS延長,QT稍為延長
III:QRS不變,QT延長
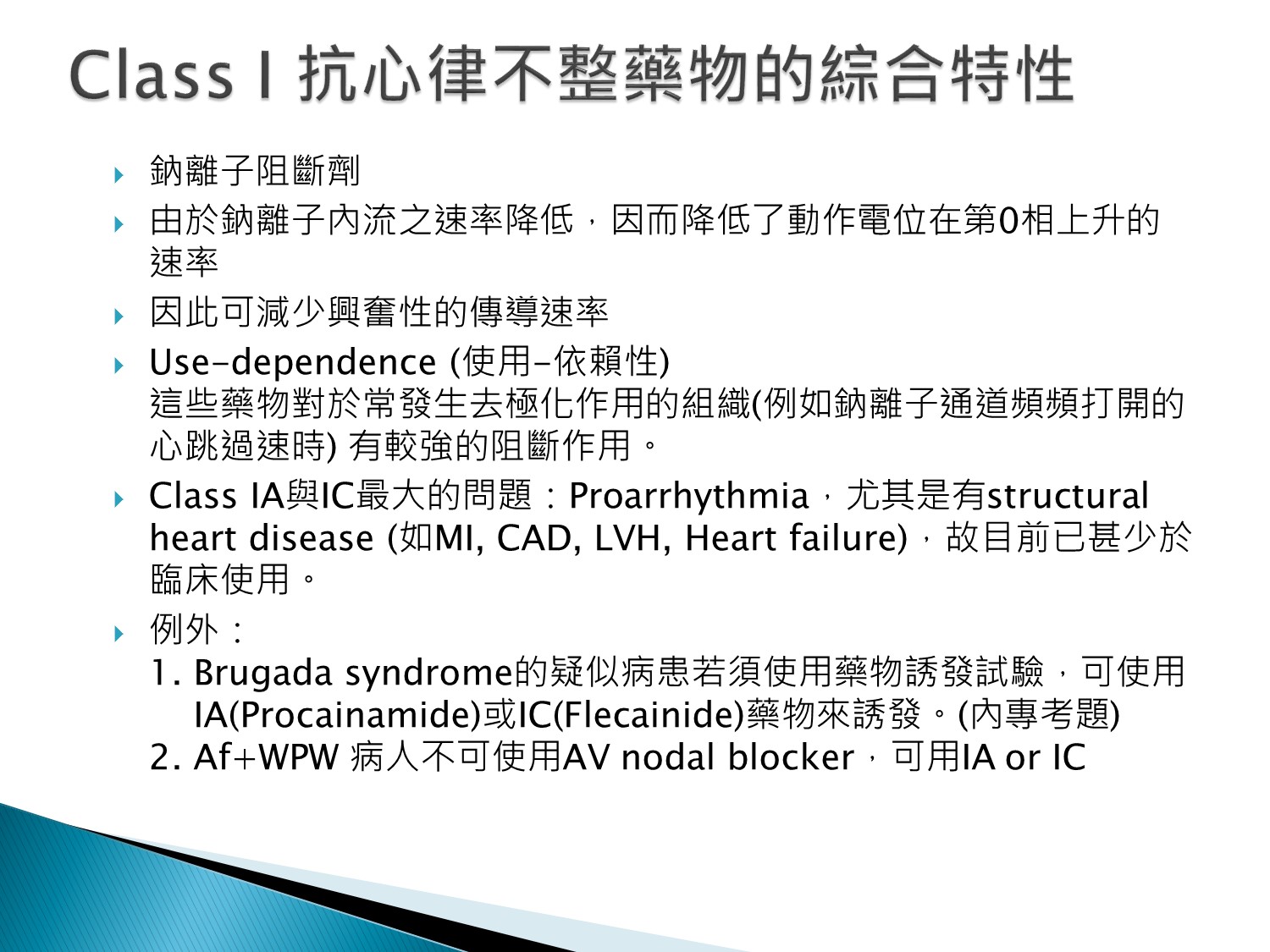
1.Use dependent:常去極化的組織作用較強,即跳動越厲害則作用越強
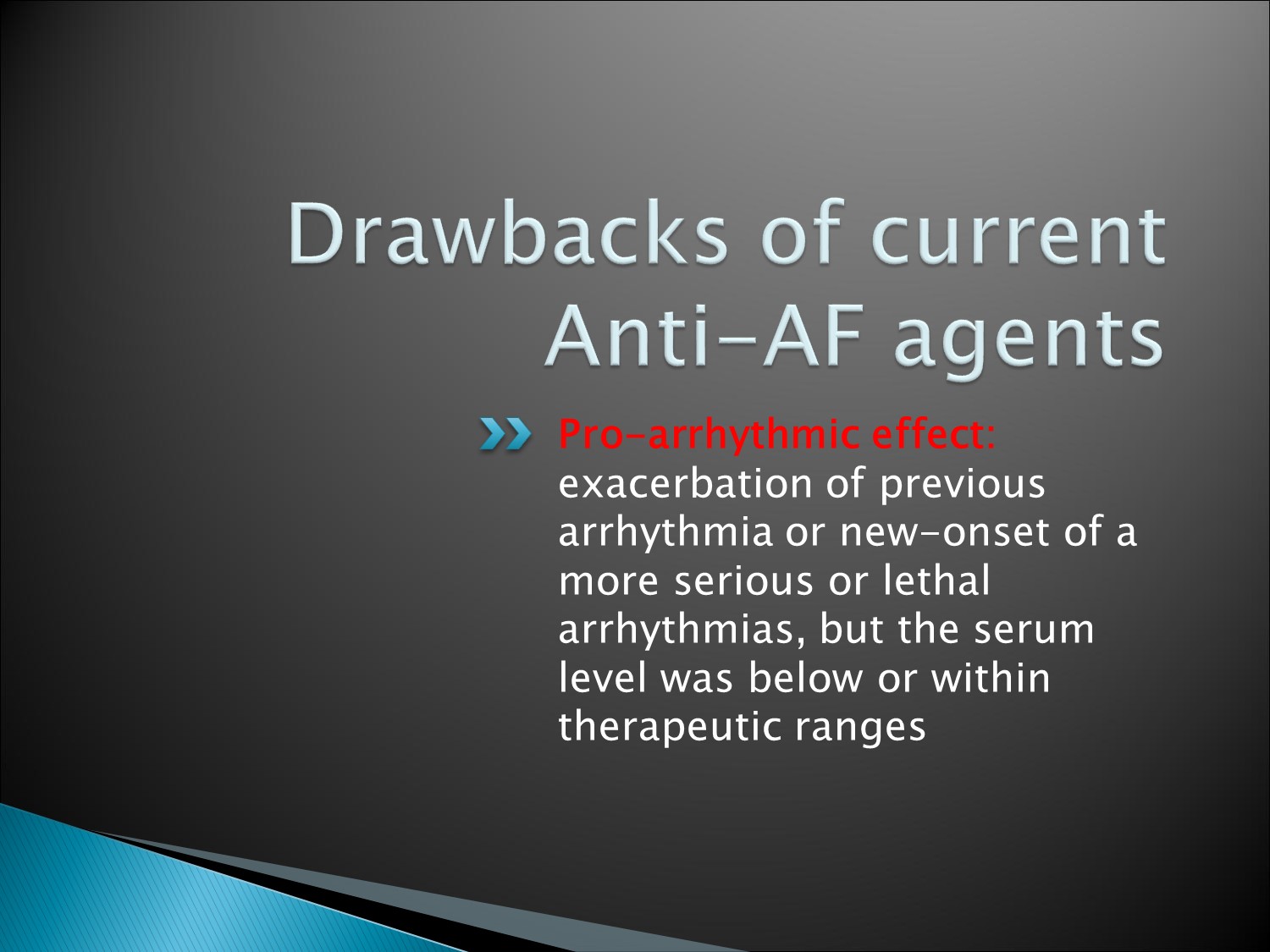
2.Proarrythmia:因為QTc會延長而造成proarrythmia,故禁用於structural heart disease
3.Af+WPW:用IA+IC對Accesory pathway也有block效果,Guideline的IA, IC是使用IV form,但台灣沒有IV form,只能電擊
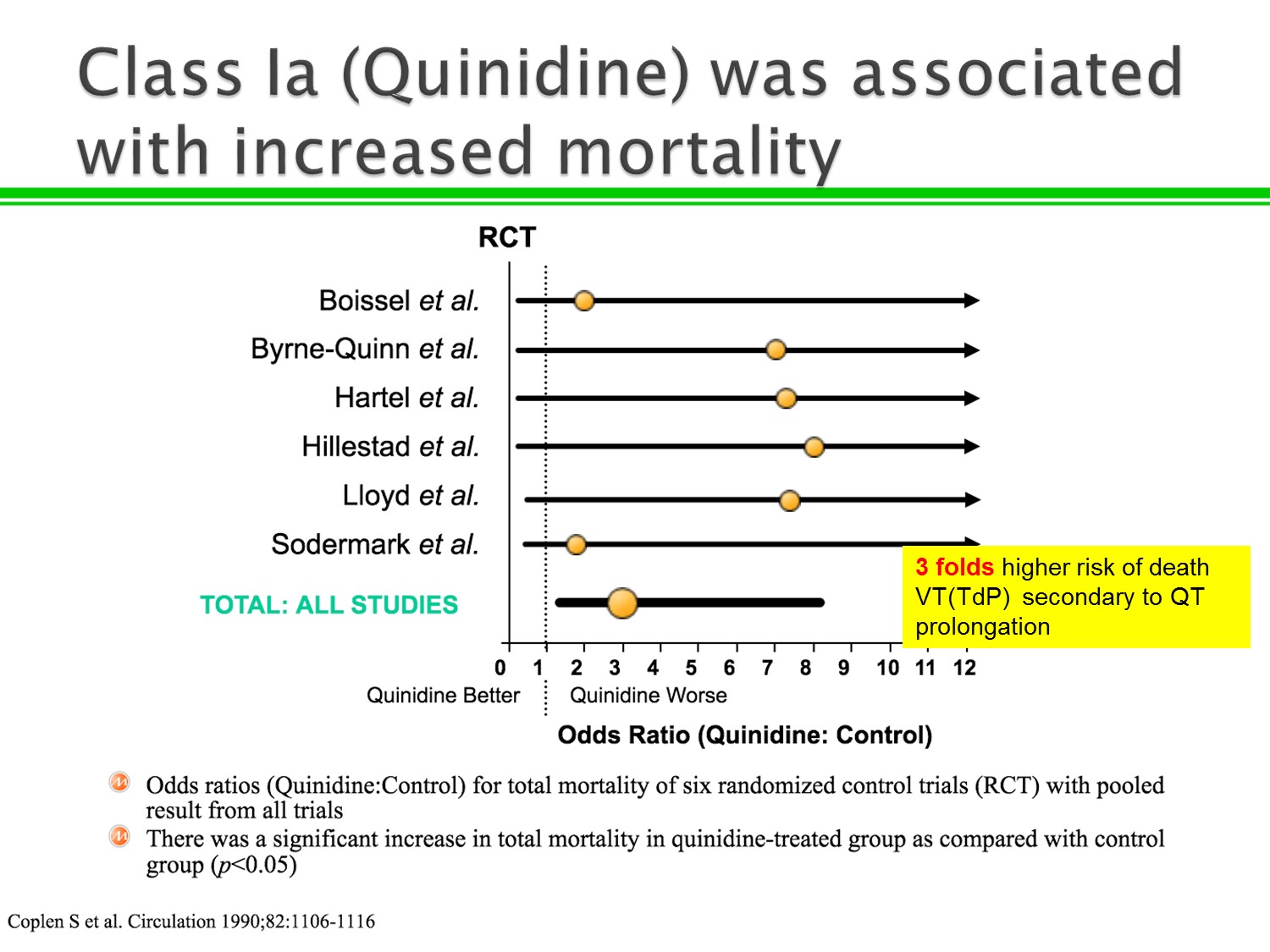
1.以前Quinidine會用在VT、VF,但研究指出mortality上升
2.原因在於QT prolong造成VT、VF及Torsade
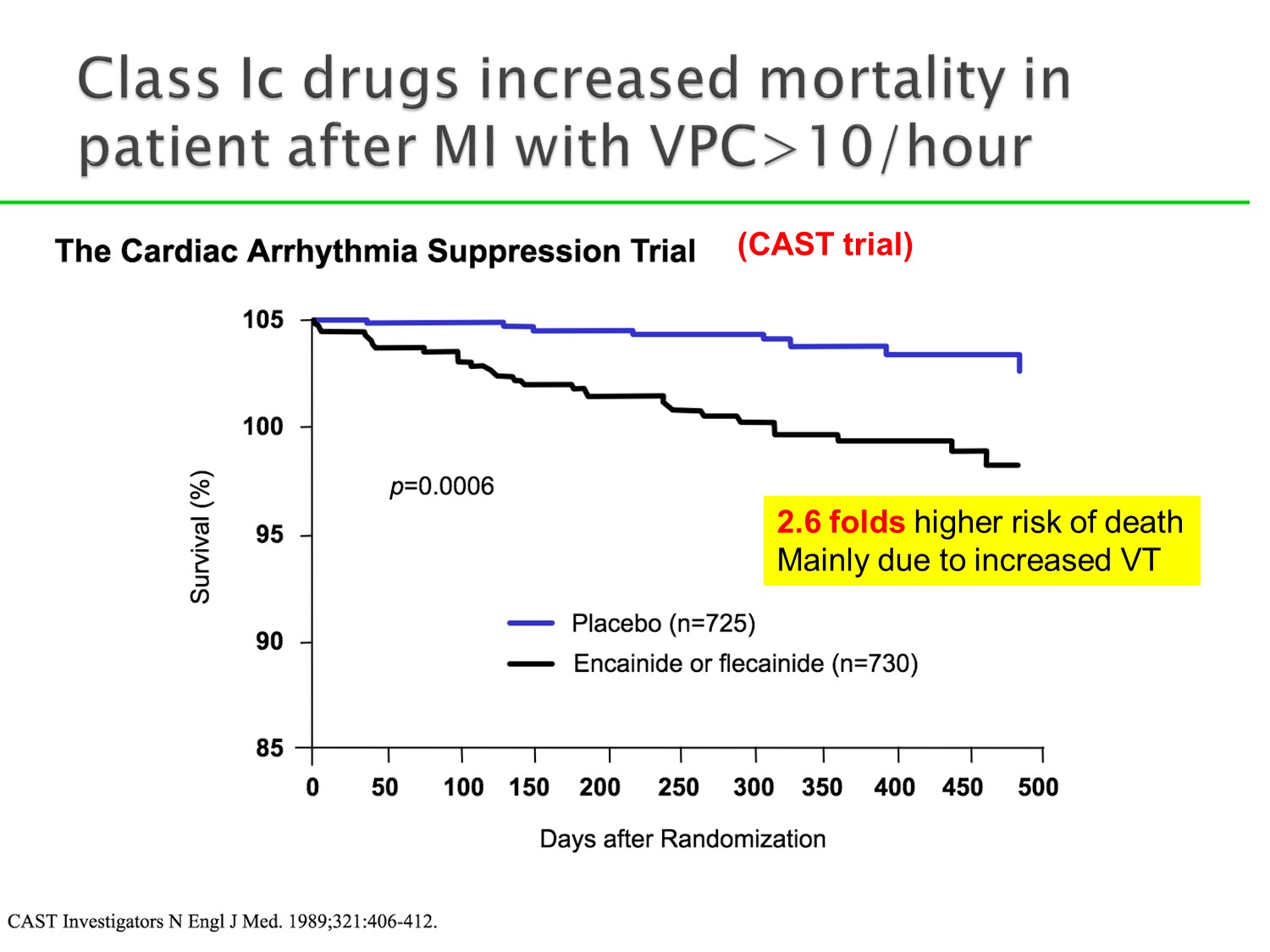
MI後VPC>10/hour者,使用Ic藥物,雖然壓制VPC,但總體死亡率上升。
原因在於增加VT機會
因此Ia、Ic目前已少用
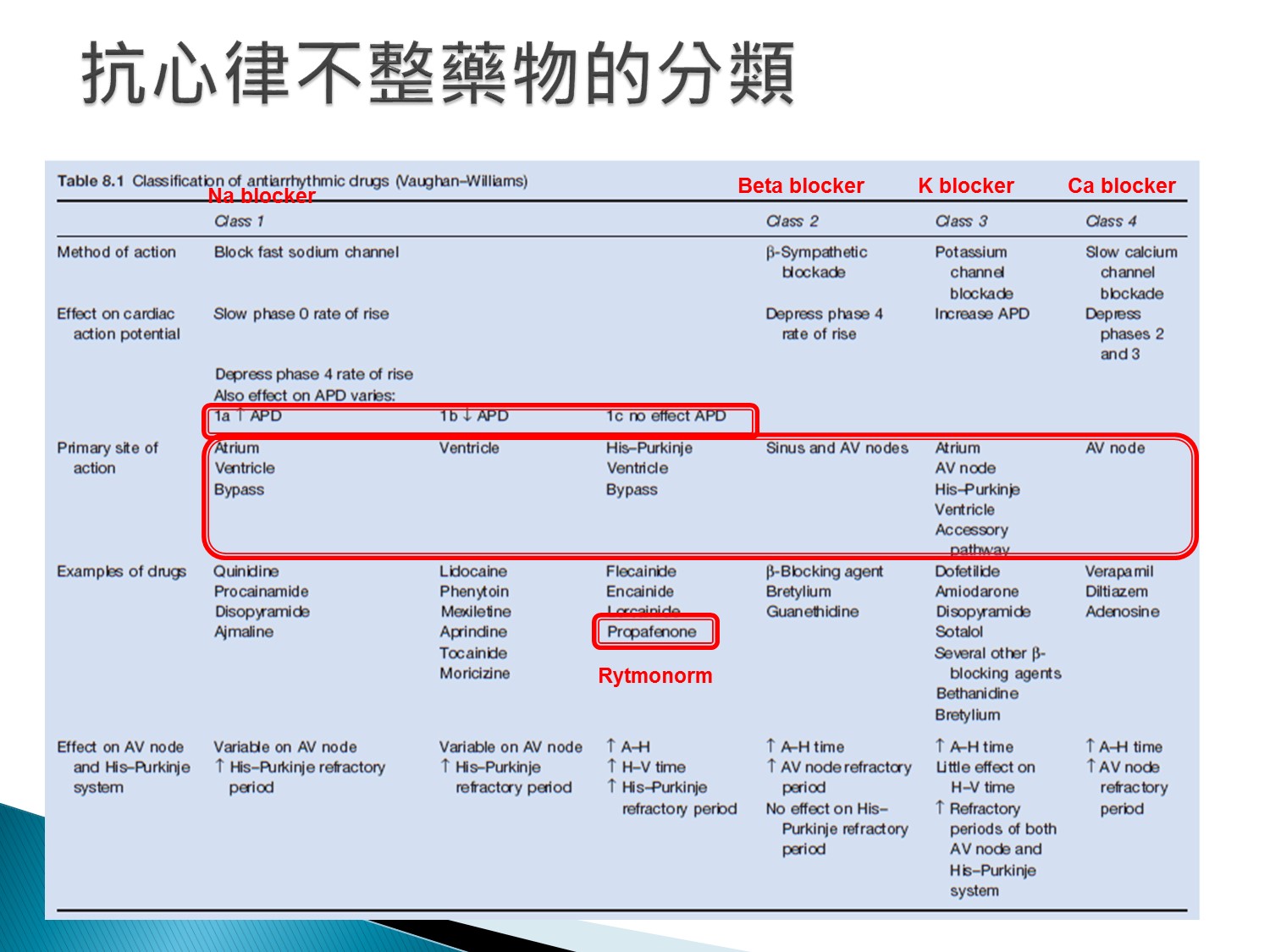
Ia、Ic對心室上及心室心律不整都有效
Ib只對心室心律不整有效,但QT不會延長
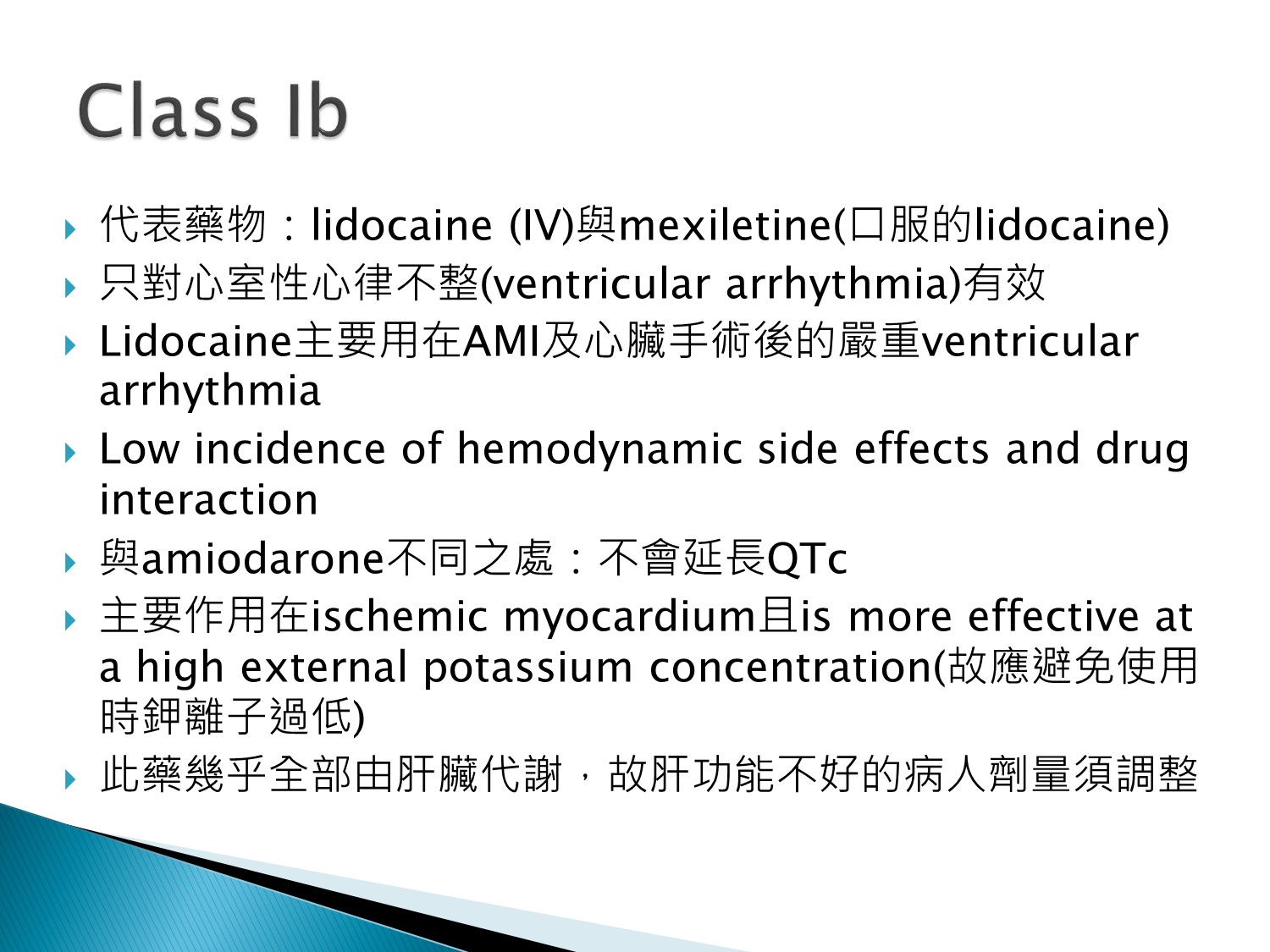
1.少有藥物交互作用
2.鉀高時使用才有效
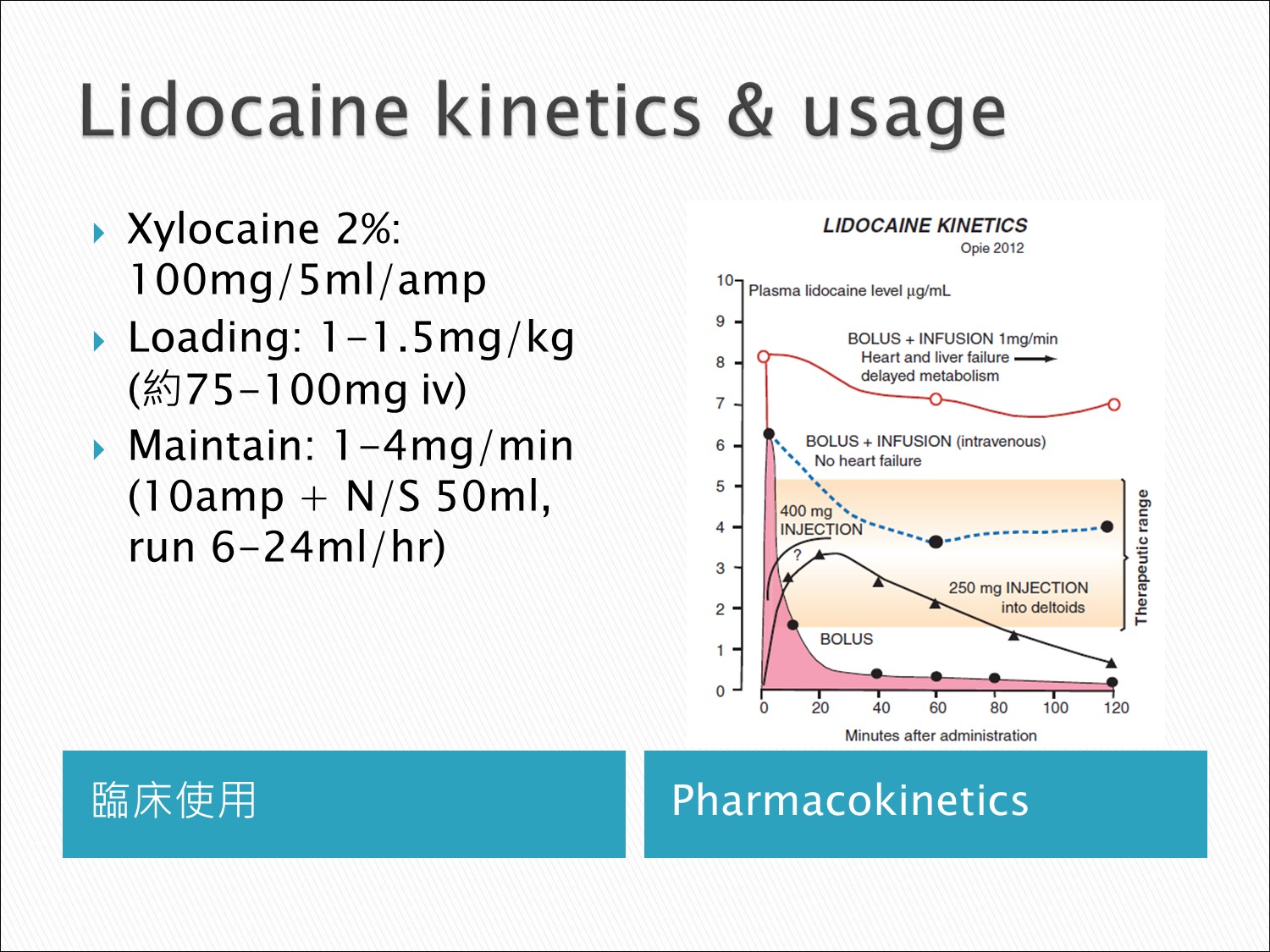
- VT、VF常用
- 一定要bolus + infusion,因為bolus完,濃度馬上掉到therapeutic range以下
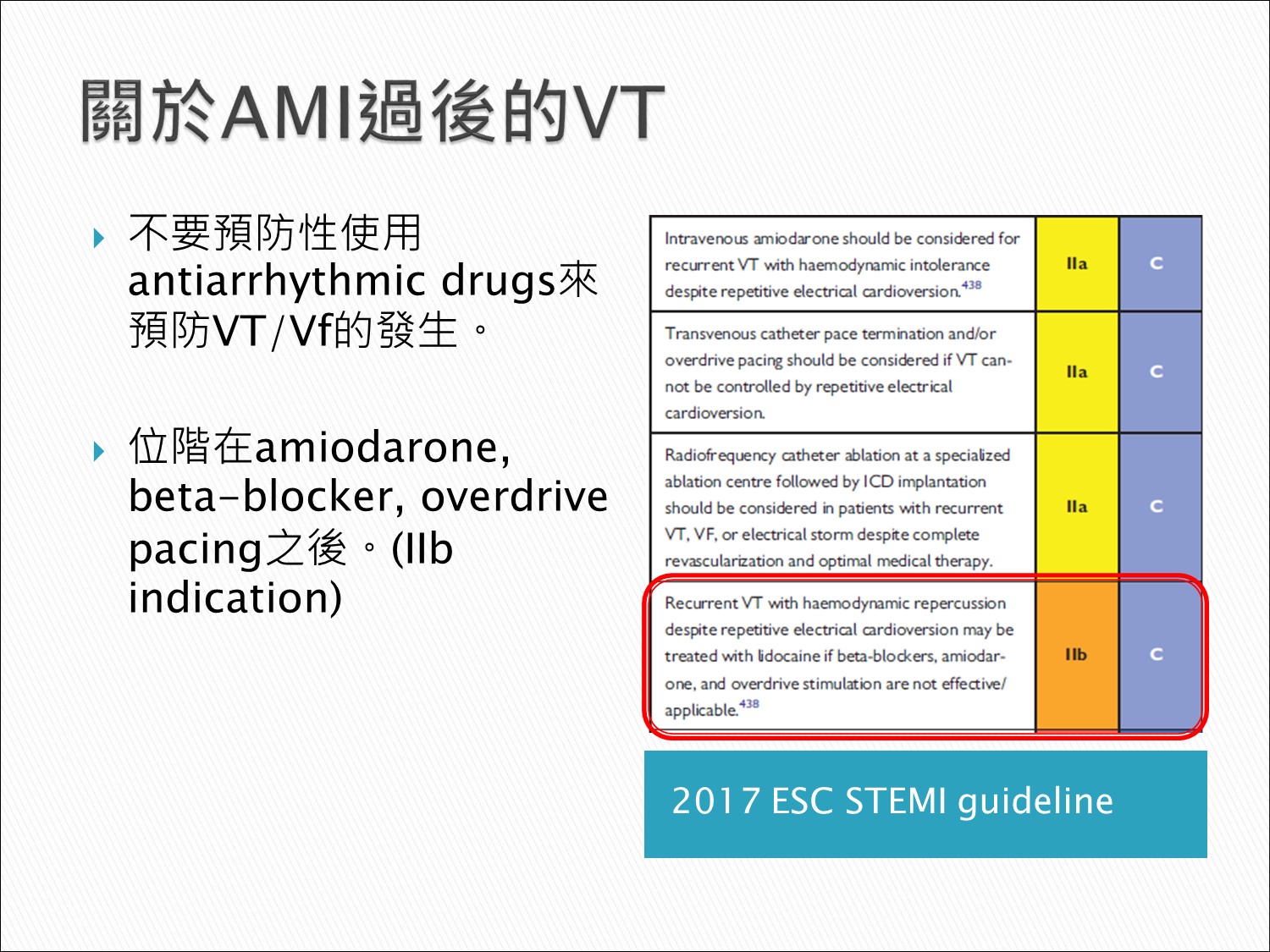
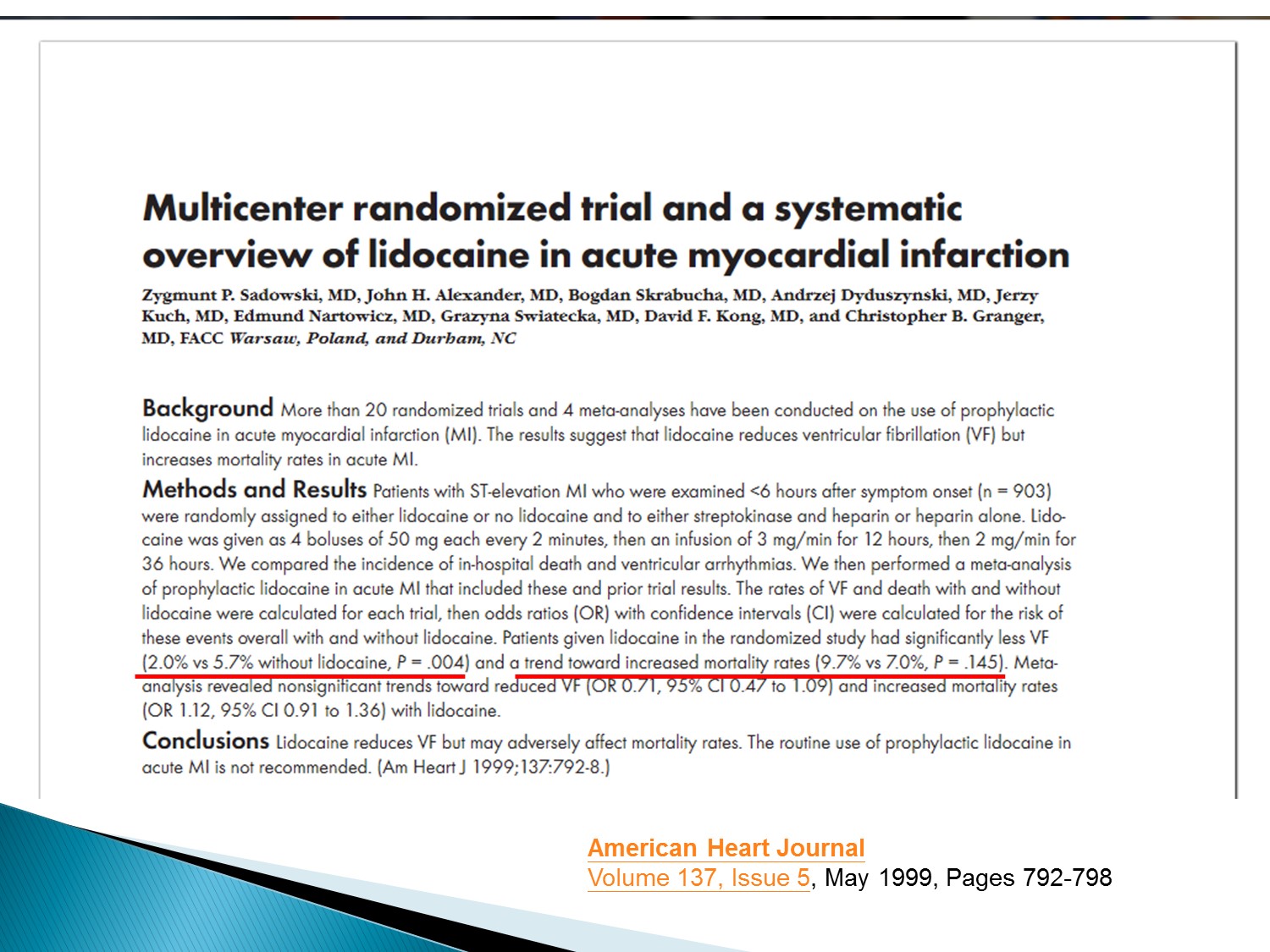
lidocaine位階較後面的原因在於雖然有效降低VF,但是增加mortality rate
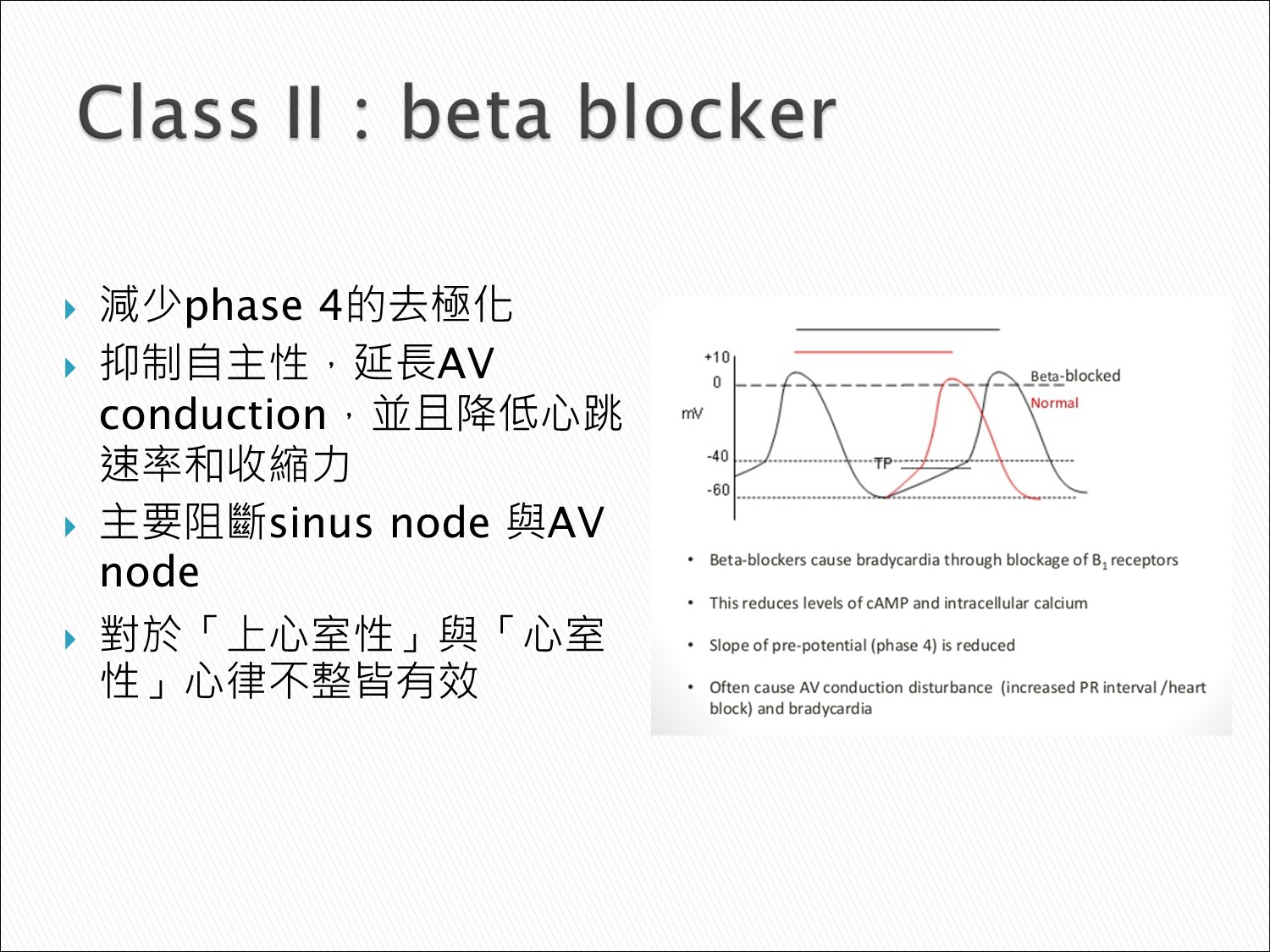
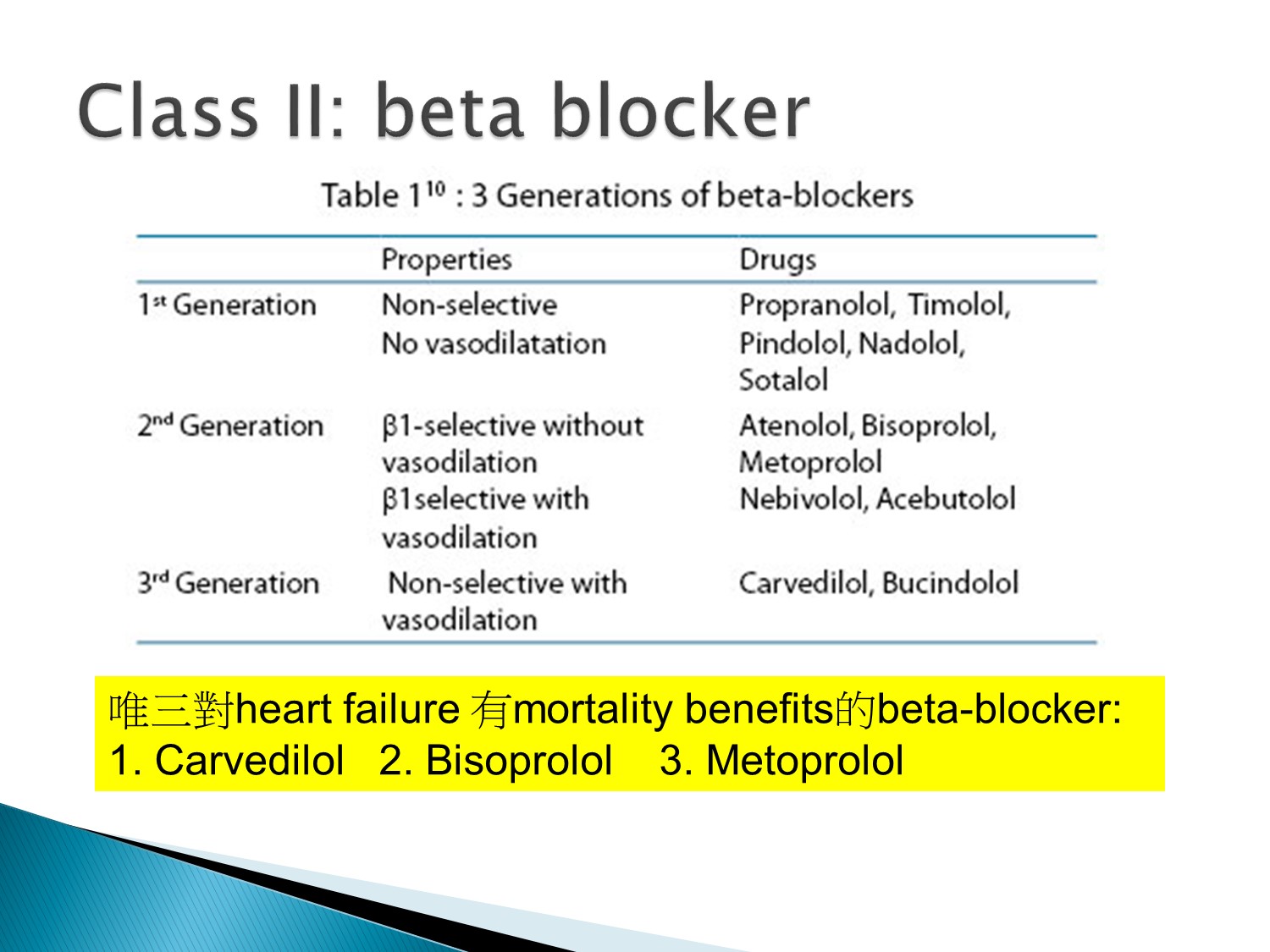
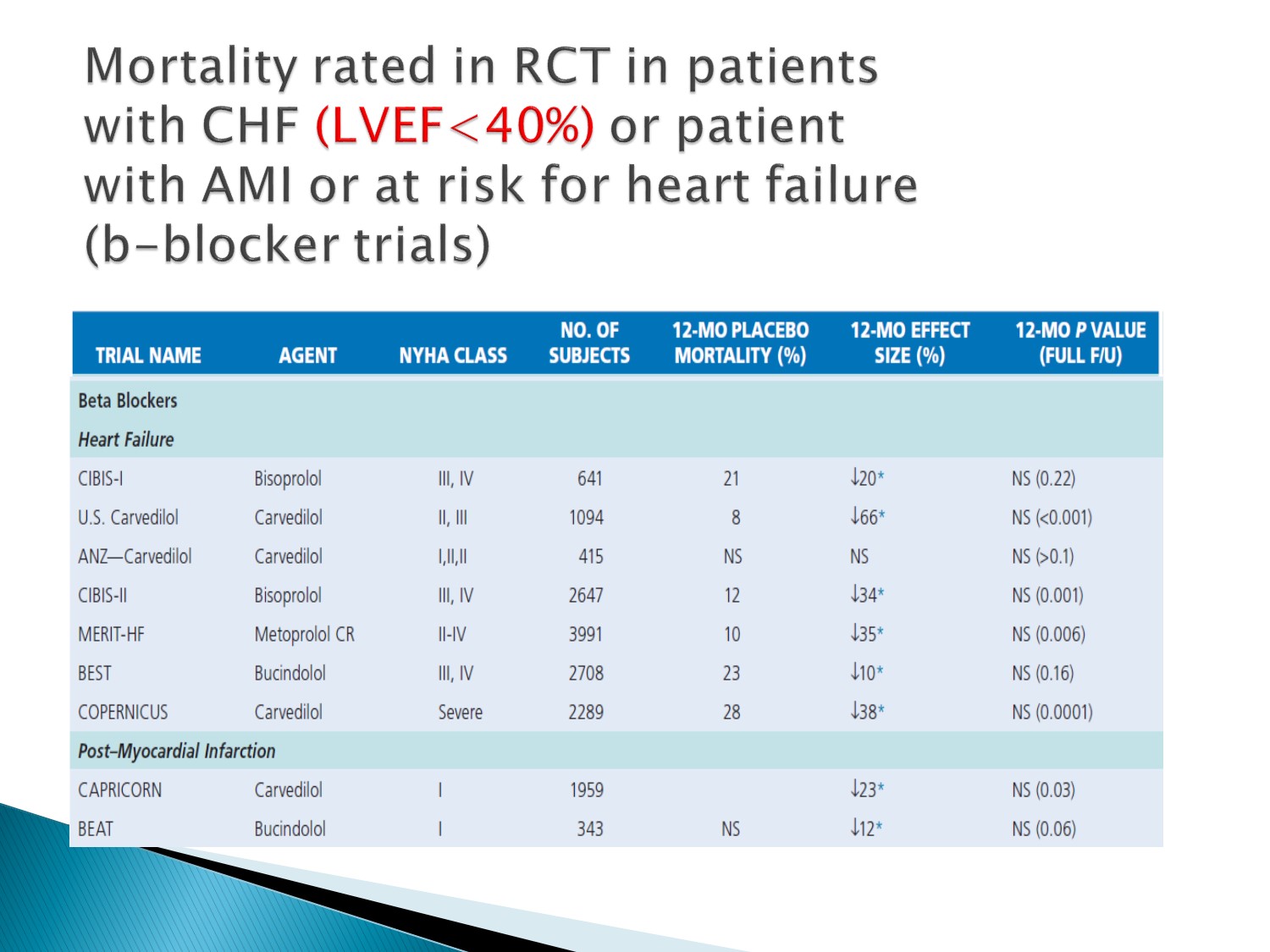
Bisoprolol, carvedilol, metoprolol在LVEF<40%者有減少mortality rate效果
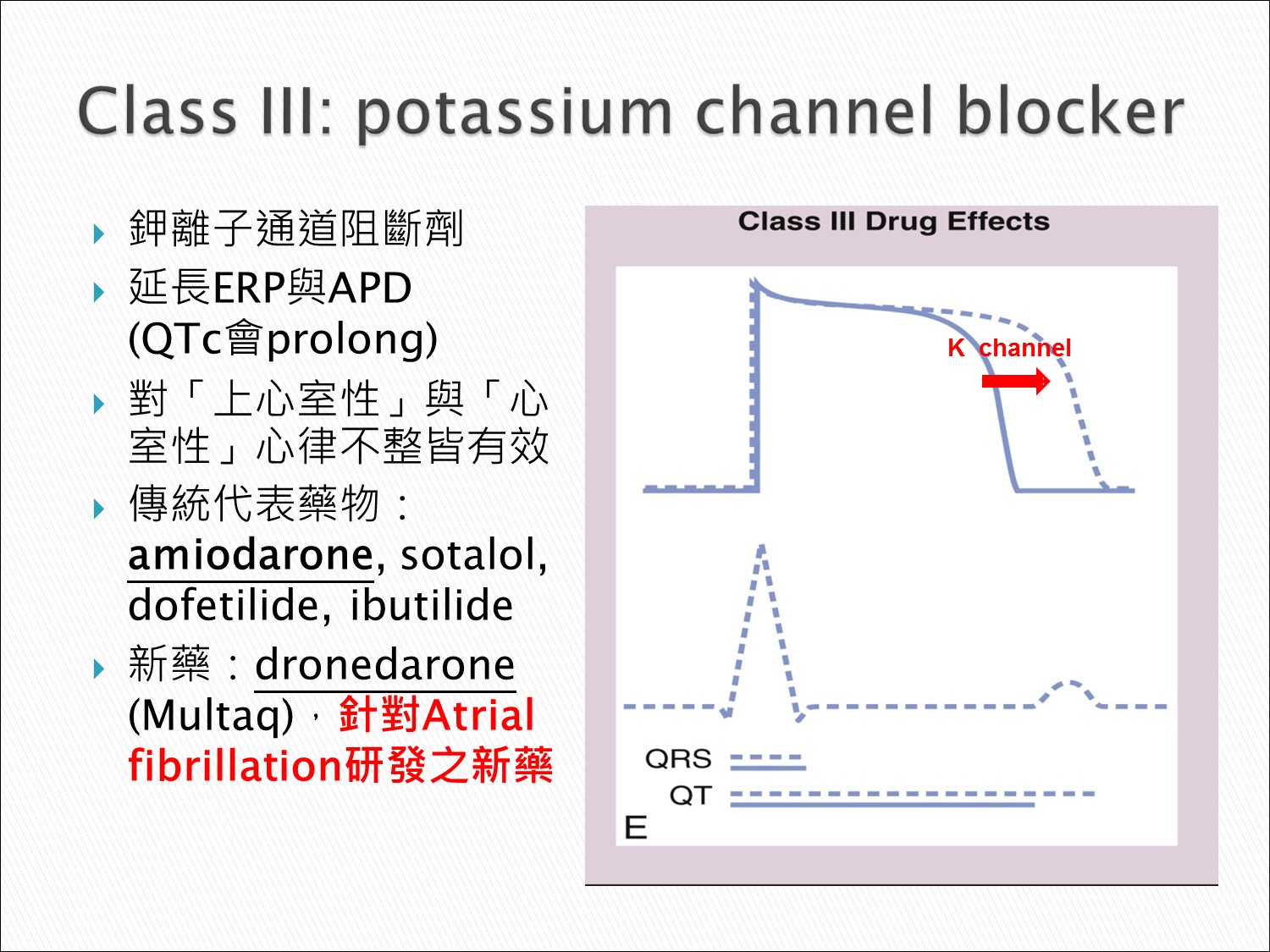
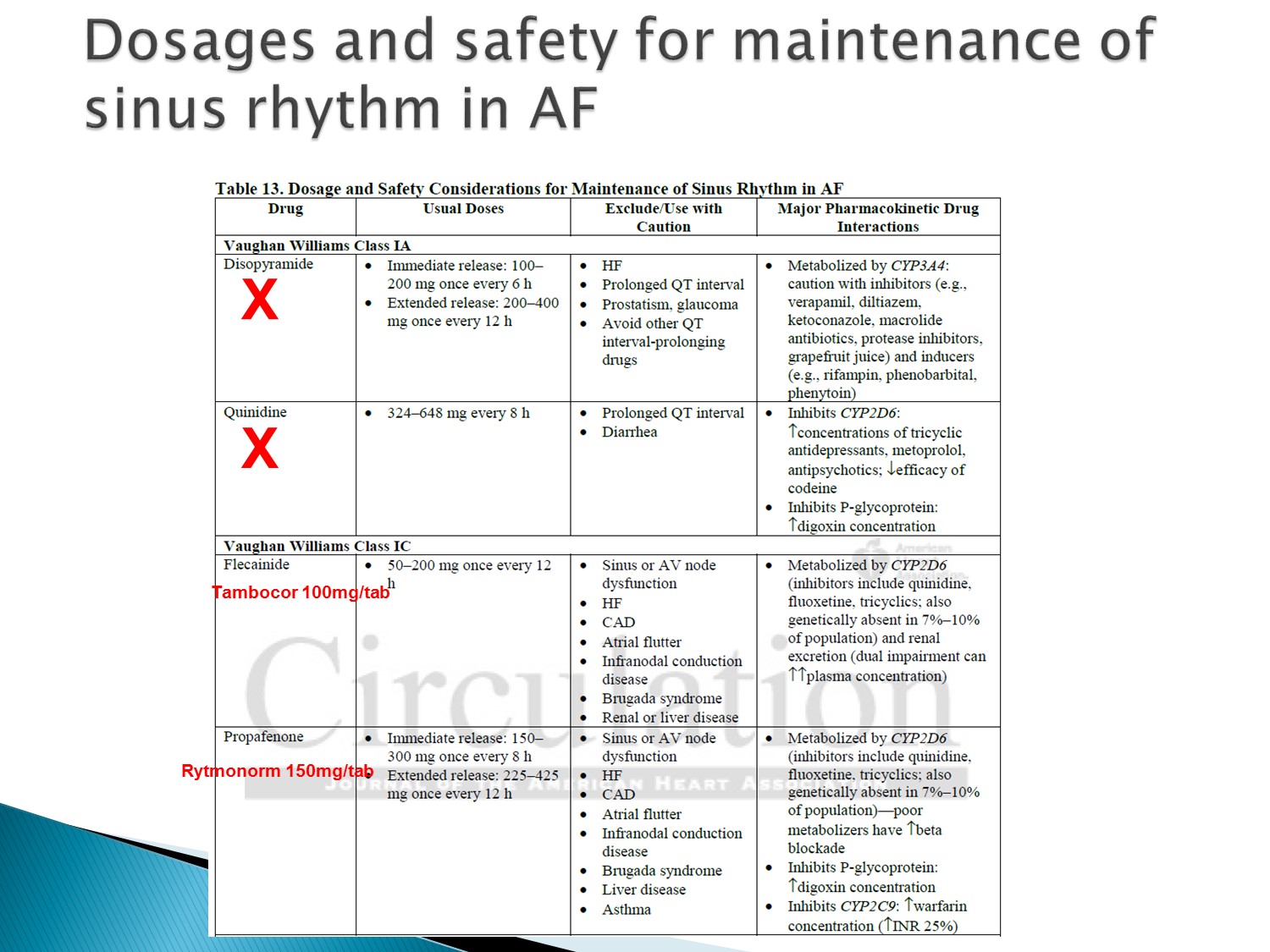
國外常用dofetilide、ibutilide,但國內只有amiodarone及sotalol
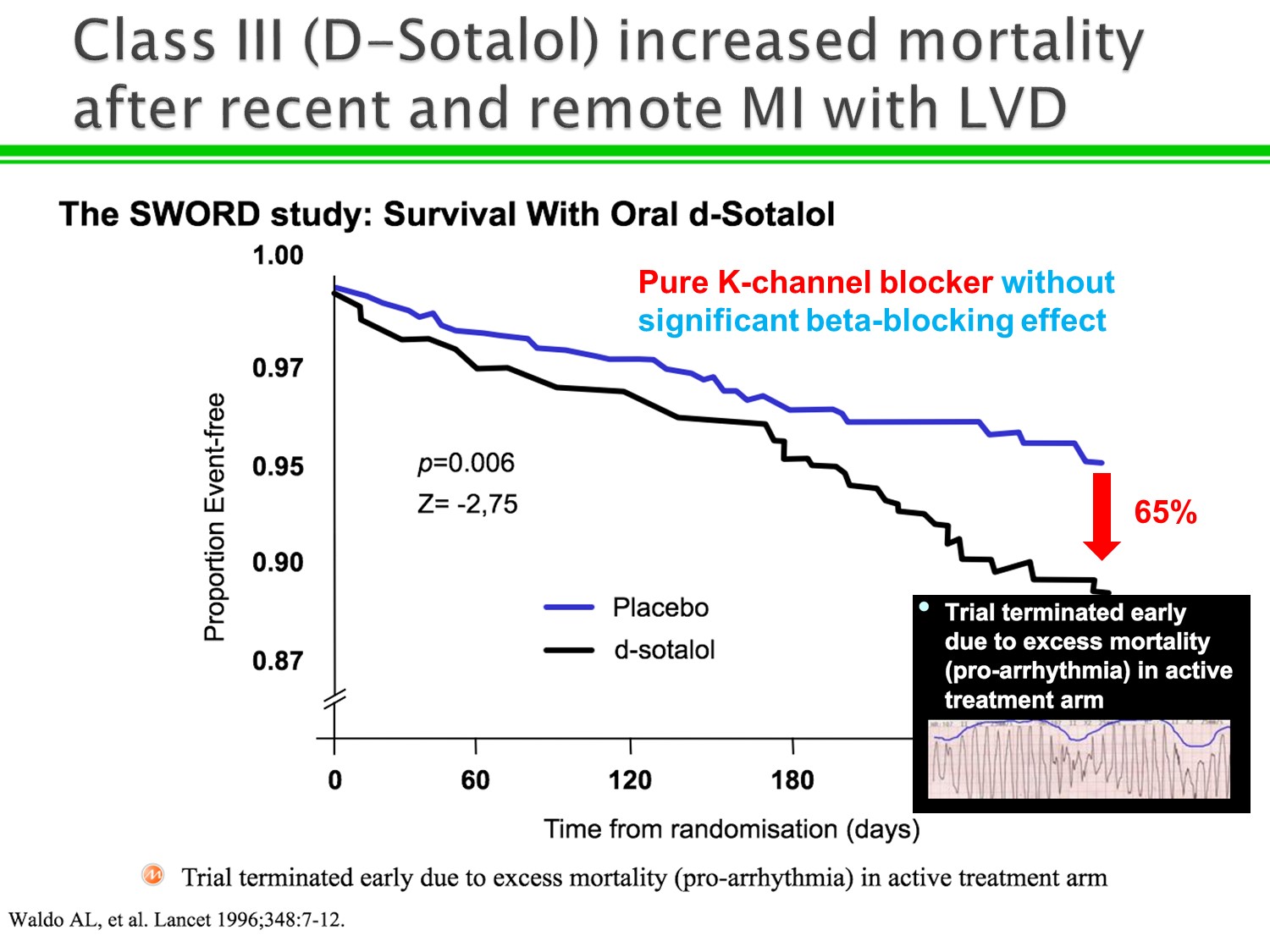
1.Sotalol 式微的原因:容易 proarrythmia 造成 torsade
2.Sotalol 不同於 amiodarone 之處:sotalol 是 pure K channel blocker,而 amiodarone 具有class I, II, III, IV特點
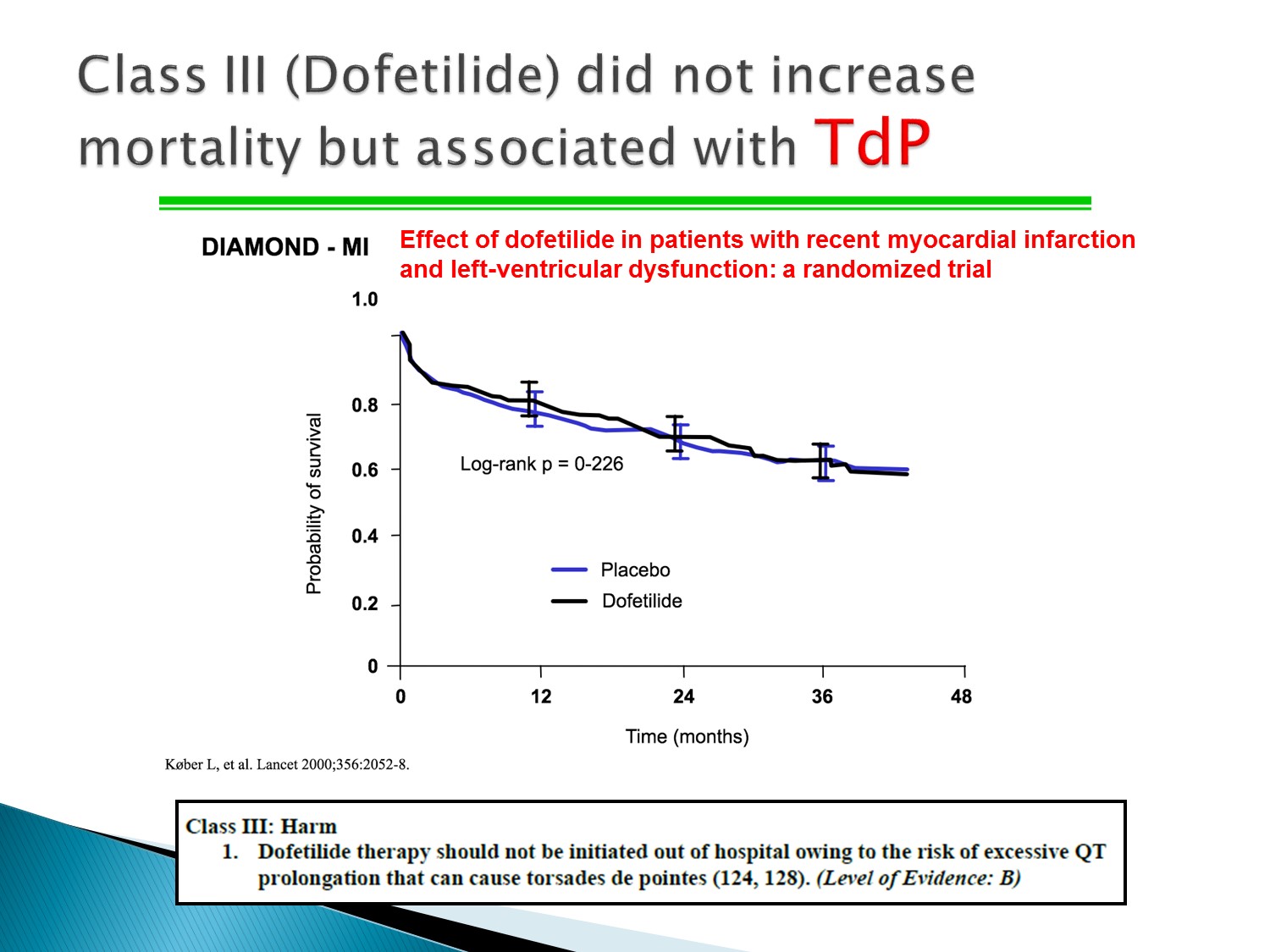
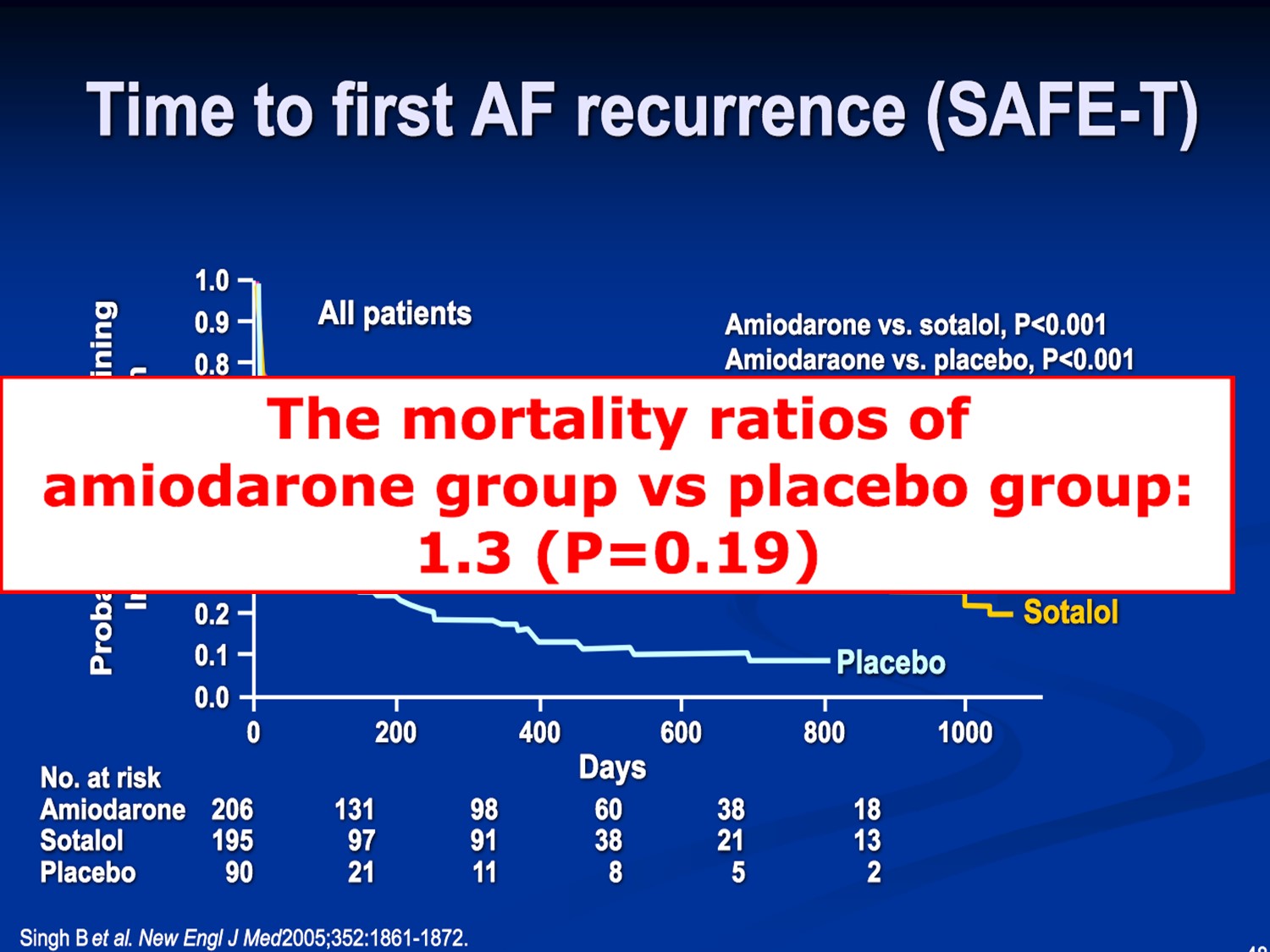
Dofetilide:Mortality 與 placebo差不多,但也有 torsade 的風險,故不可用在 OPD 病患
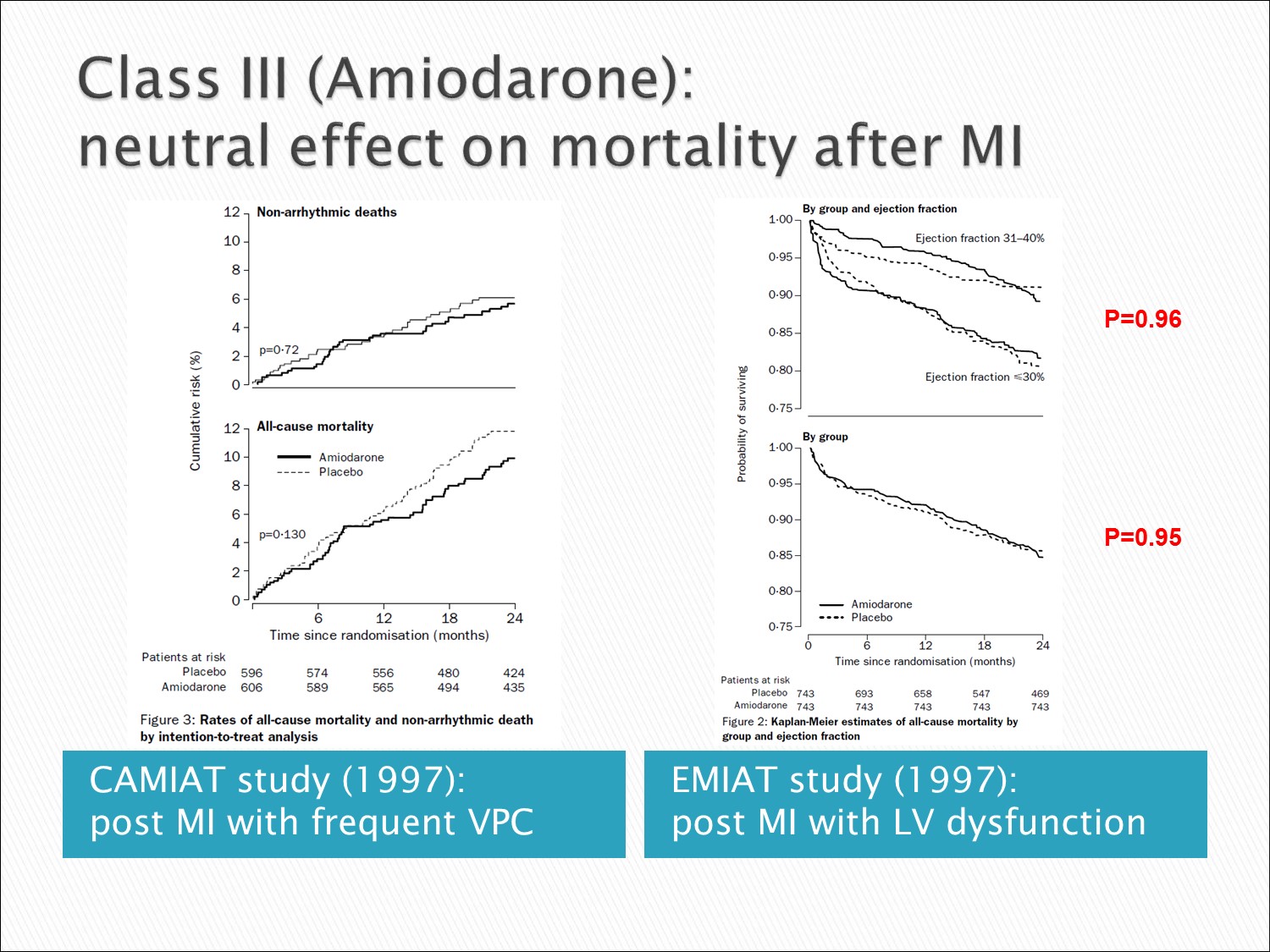
Amiodarone:Mortality 與 placebo 差不多,甚至好一些,故為 AMI 後 VT 的首選
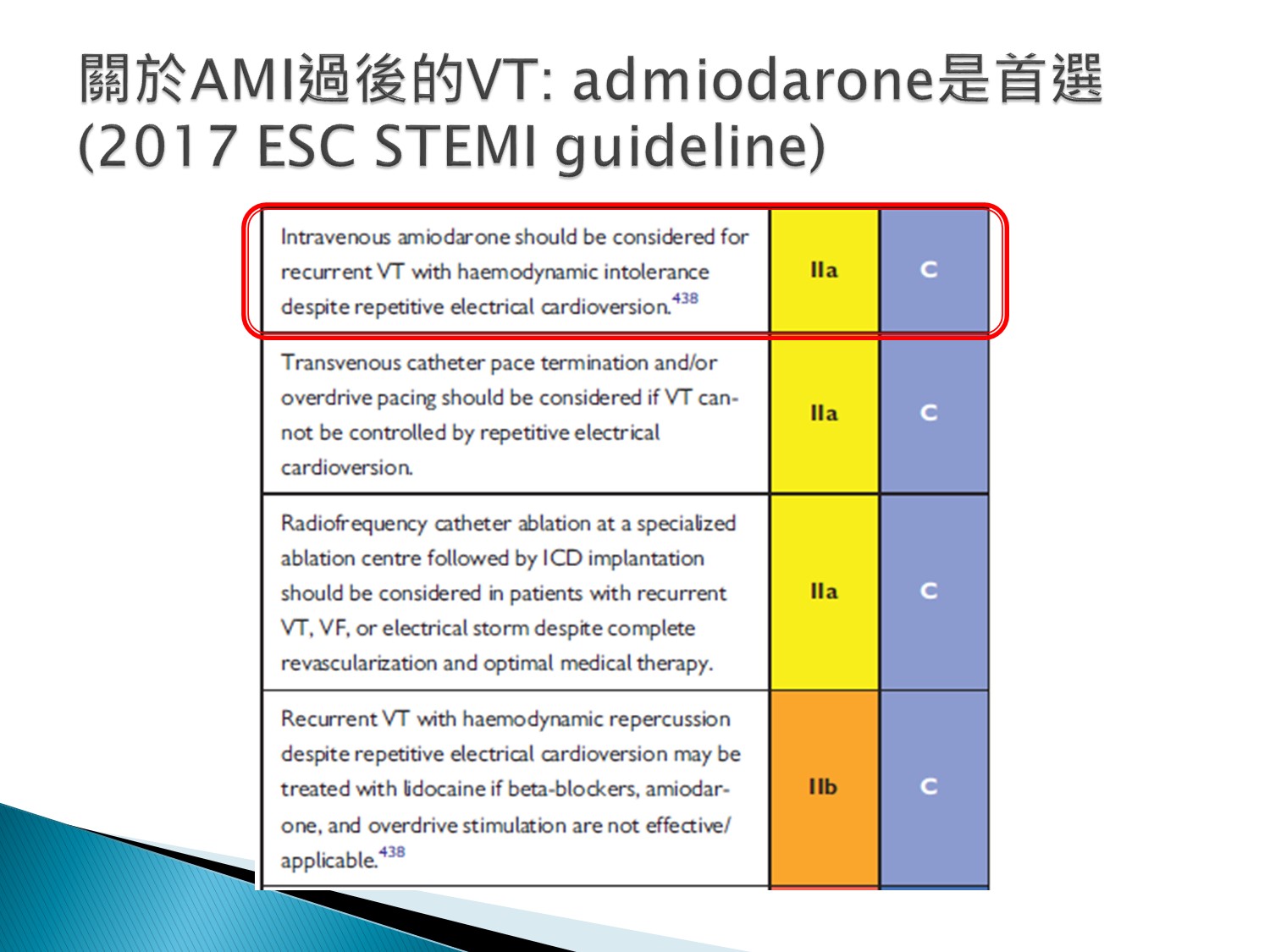
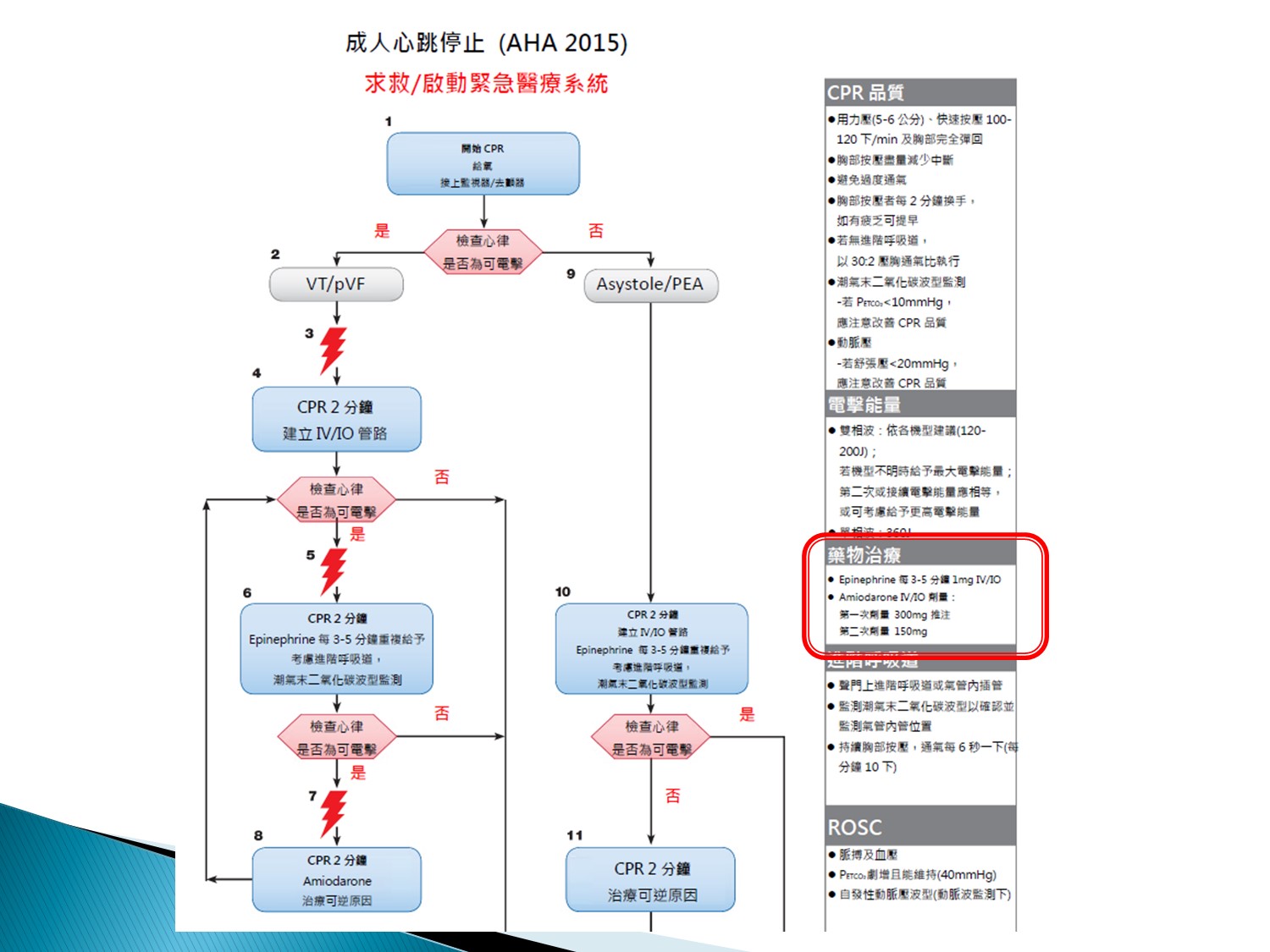
ACLS:amiodarone是用”IV push”的
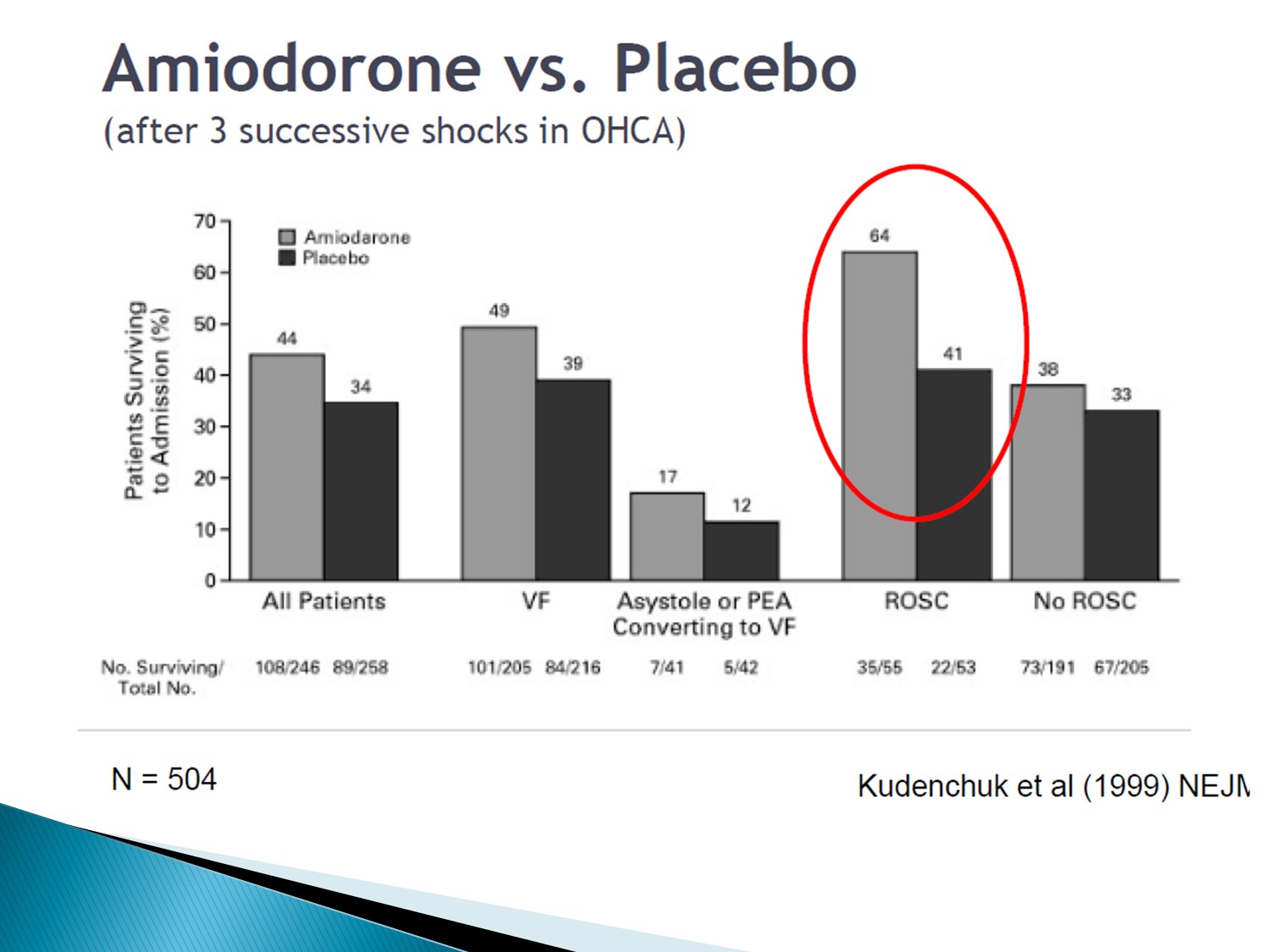
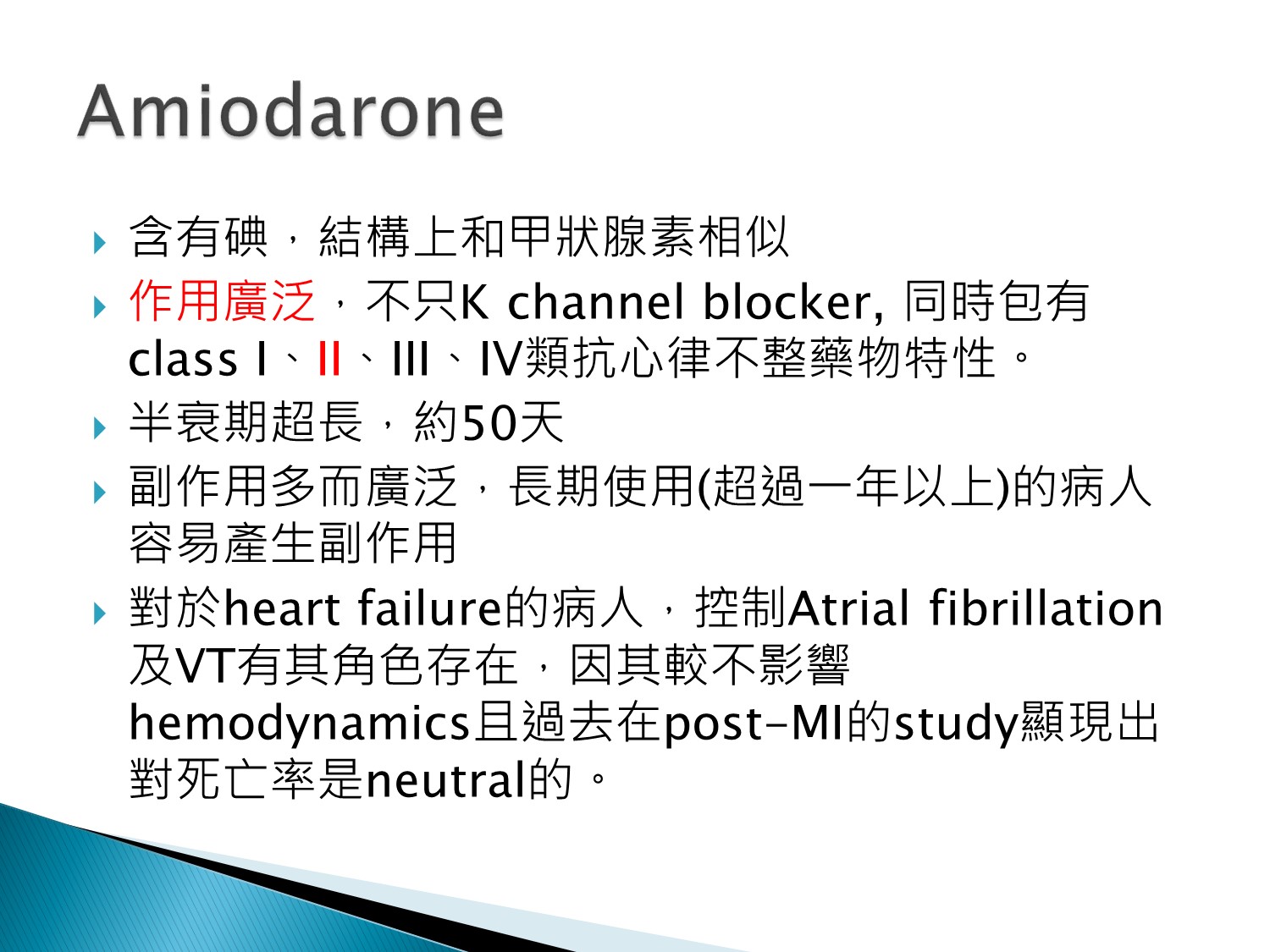
比其他Class III藥物好是因為有Class II effect
Class II effect 可減少VPC
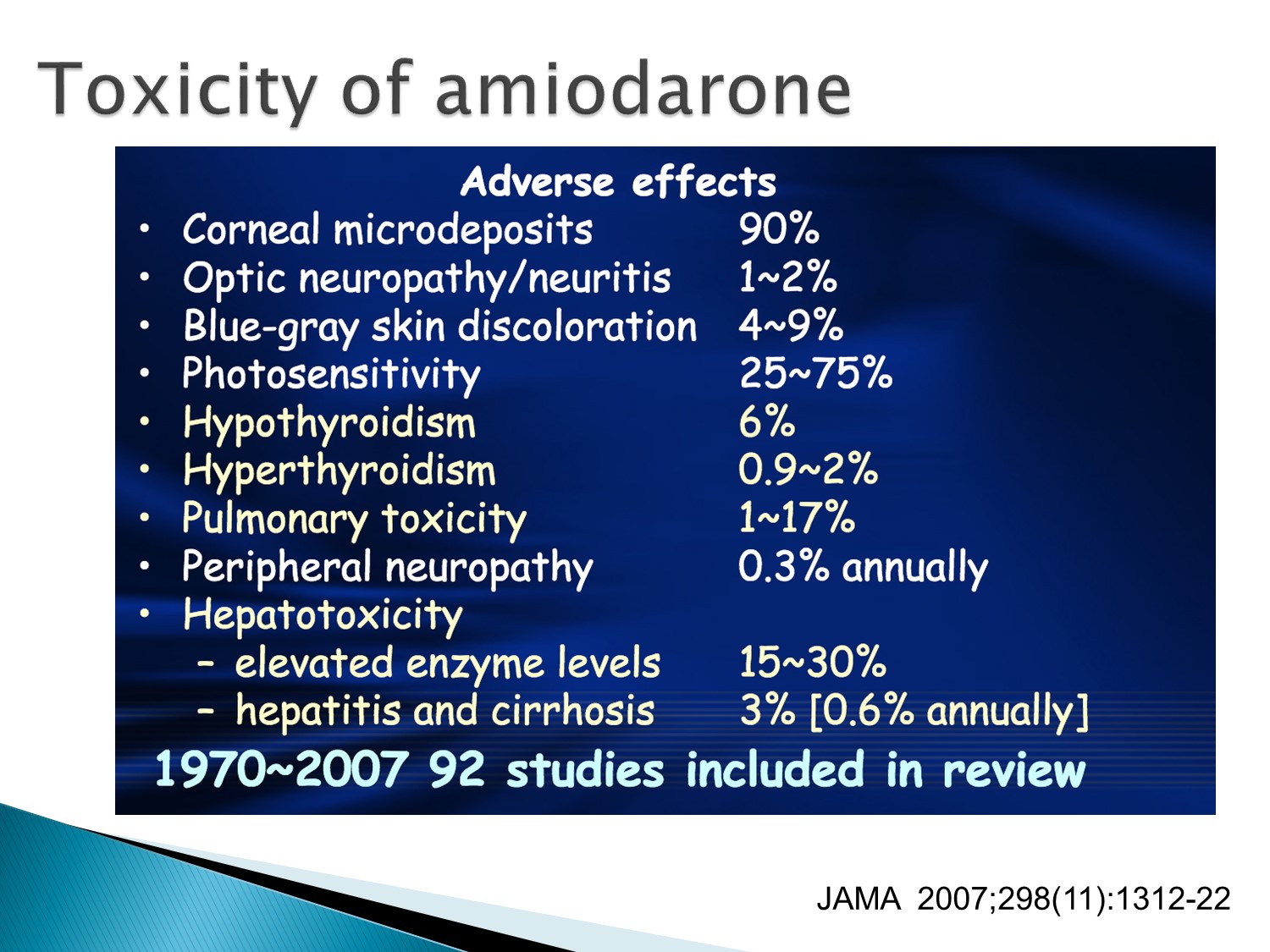
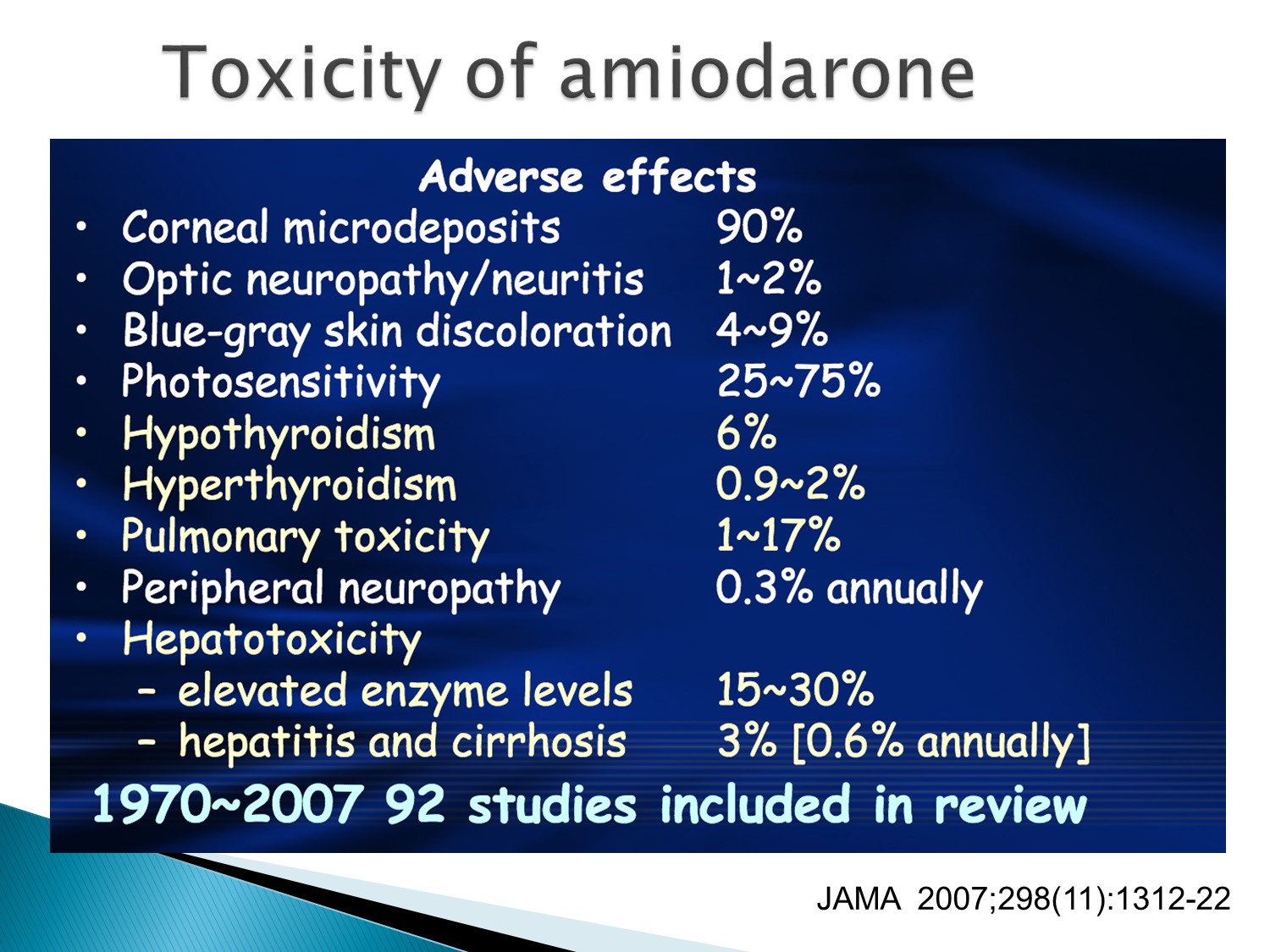
Corneal microdeposit:用越久,dose越高,陳積越多
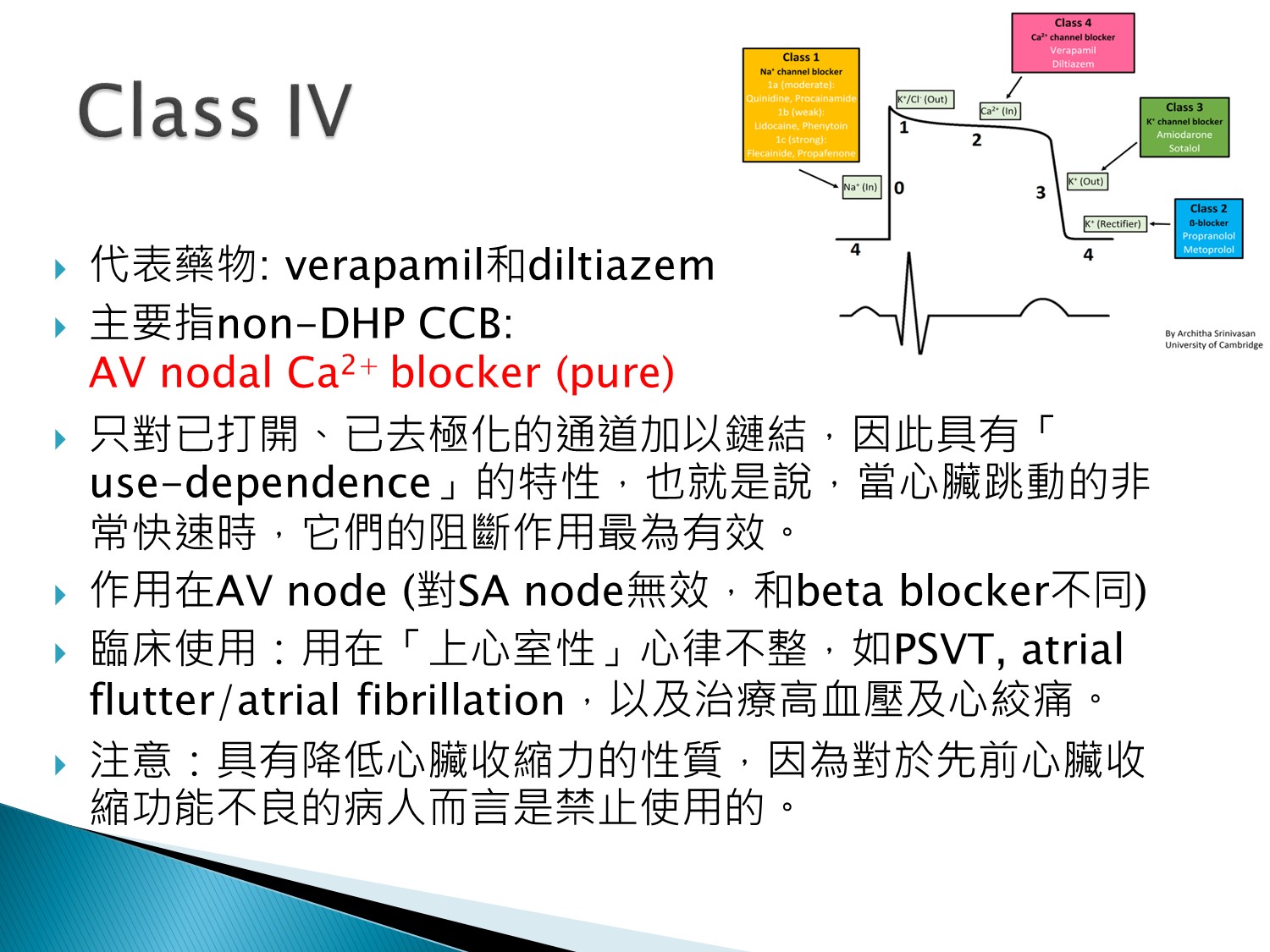
是pure AV nodal blocker,用在上心室性心律不整
禁用在LV dysfunction者
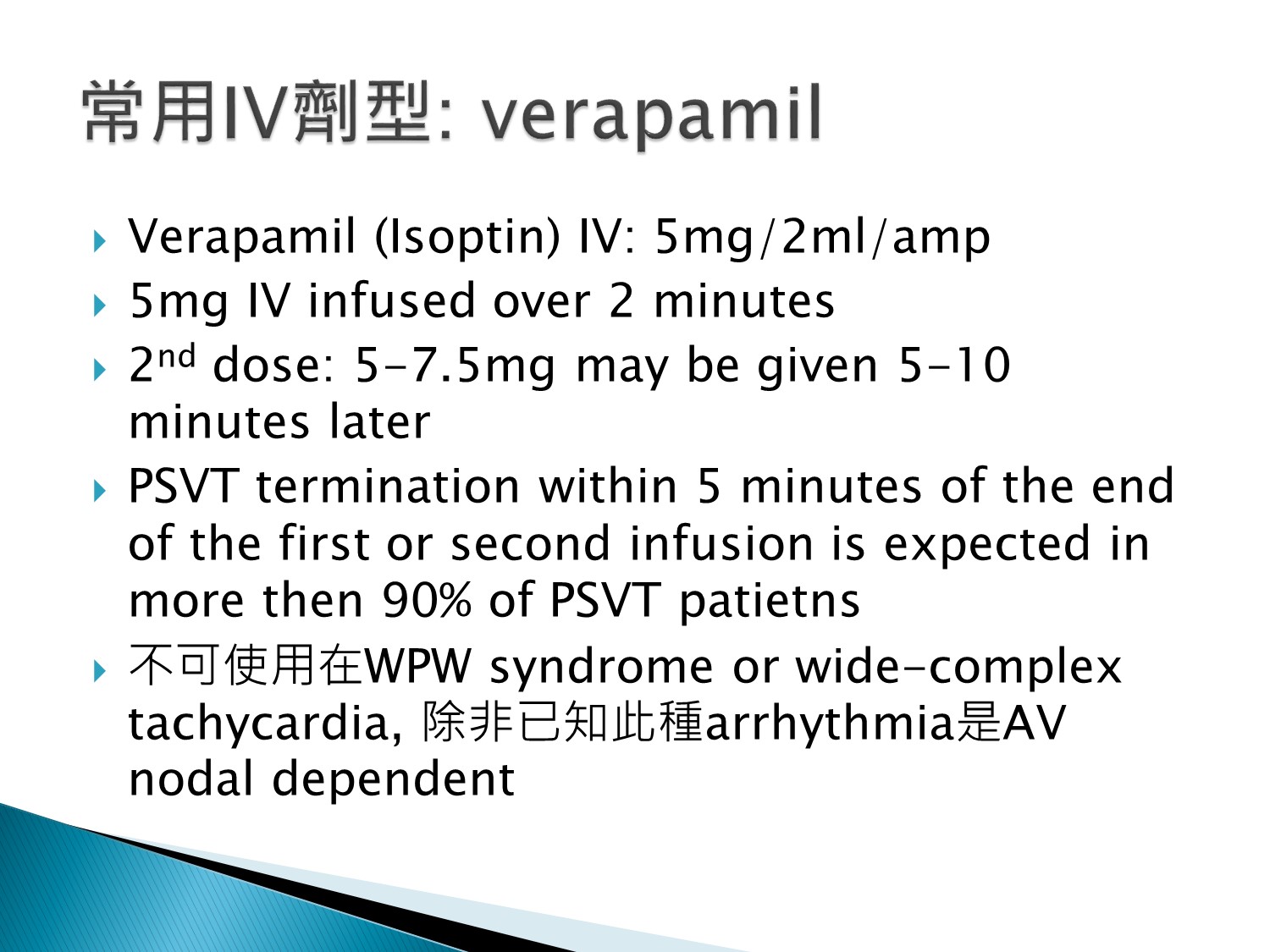
WPW會induced VT、VF
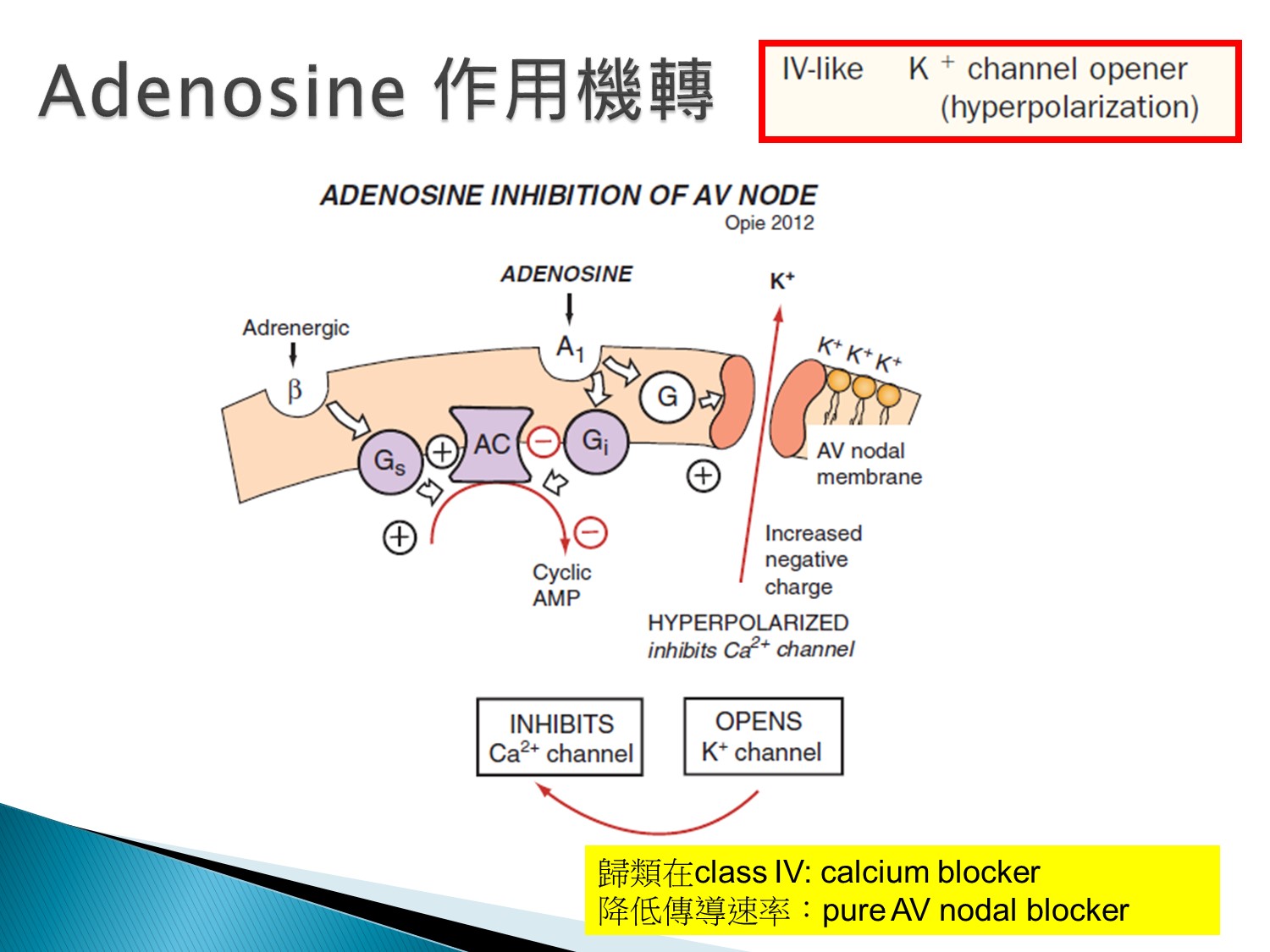
Adenosin其實是K channel opener,接著造成Ca channel block,算是class 4 like藥物
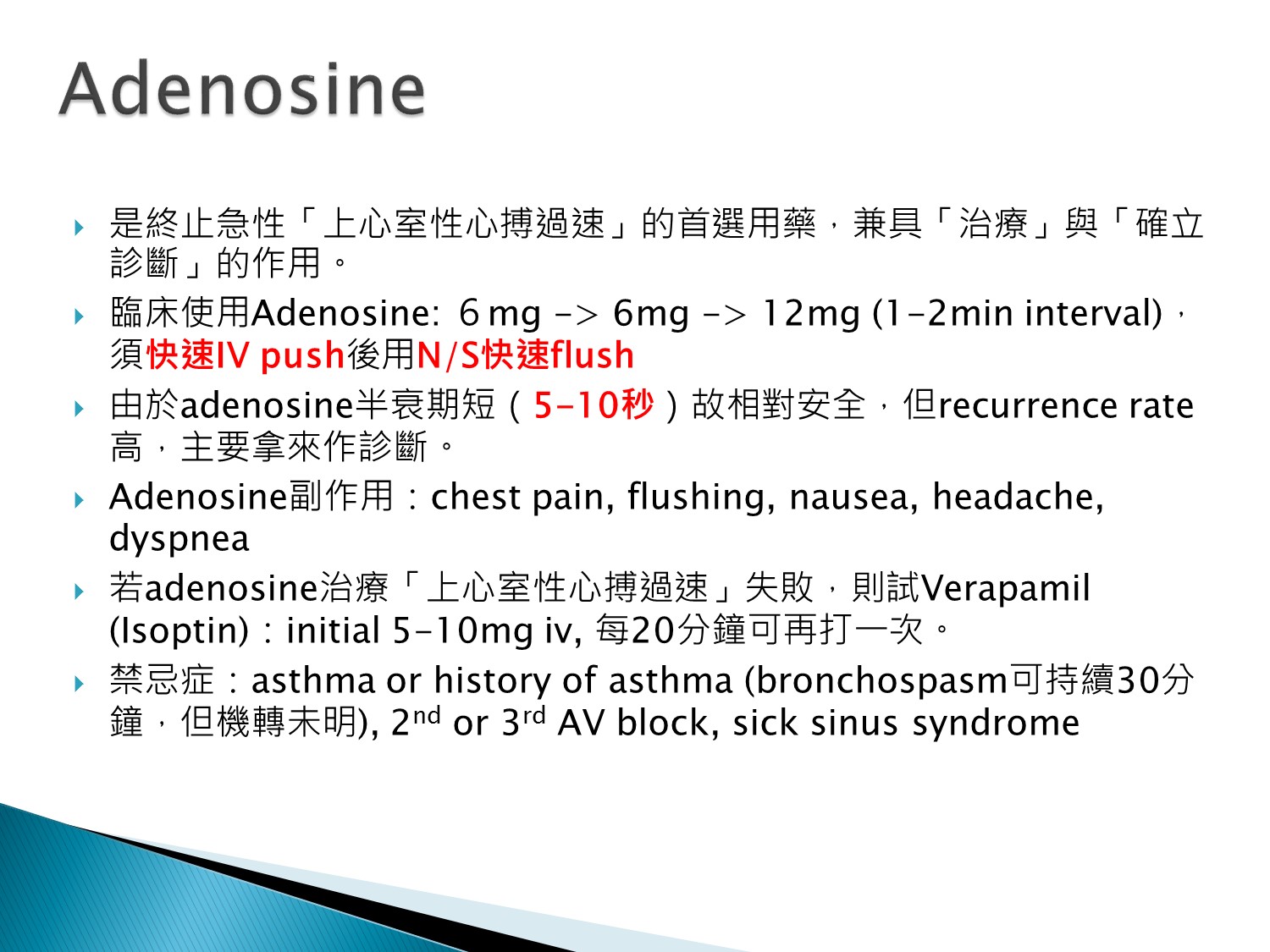
用在確立診斷
若打下去失敗,可以使用verapamil
用之前要先問有無氣喘(禁用)
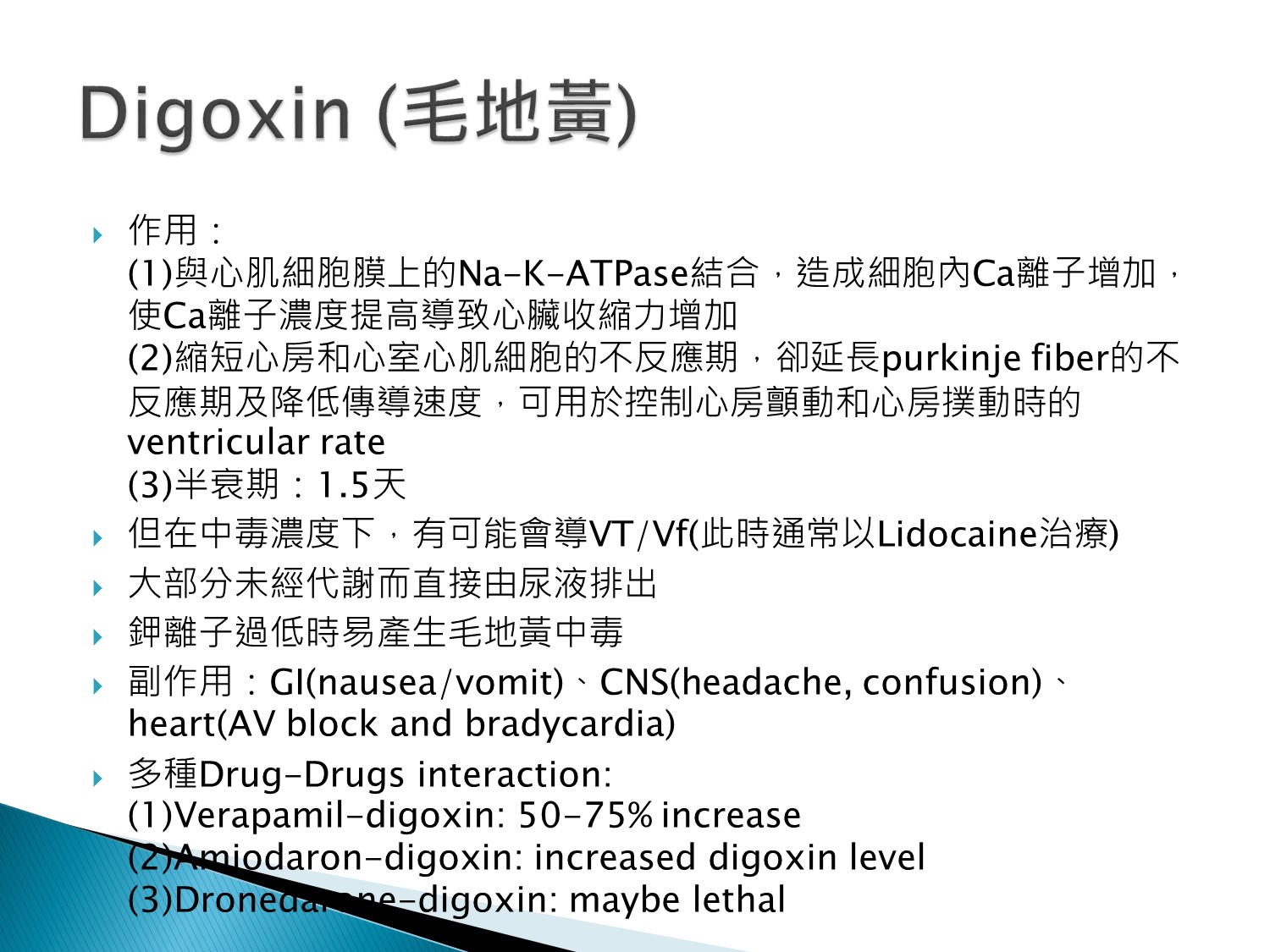
1.腎不好者小心代謝慢
2.HF者常併用利尿劑,要小心鉀過低而中毒
3.有多個藥物交互作用要小心
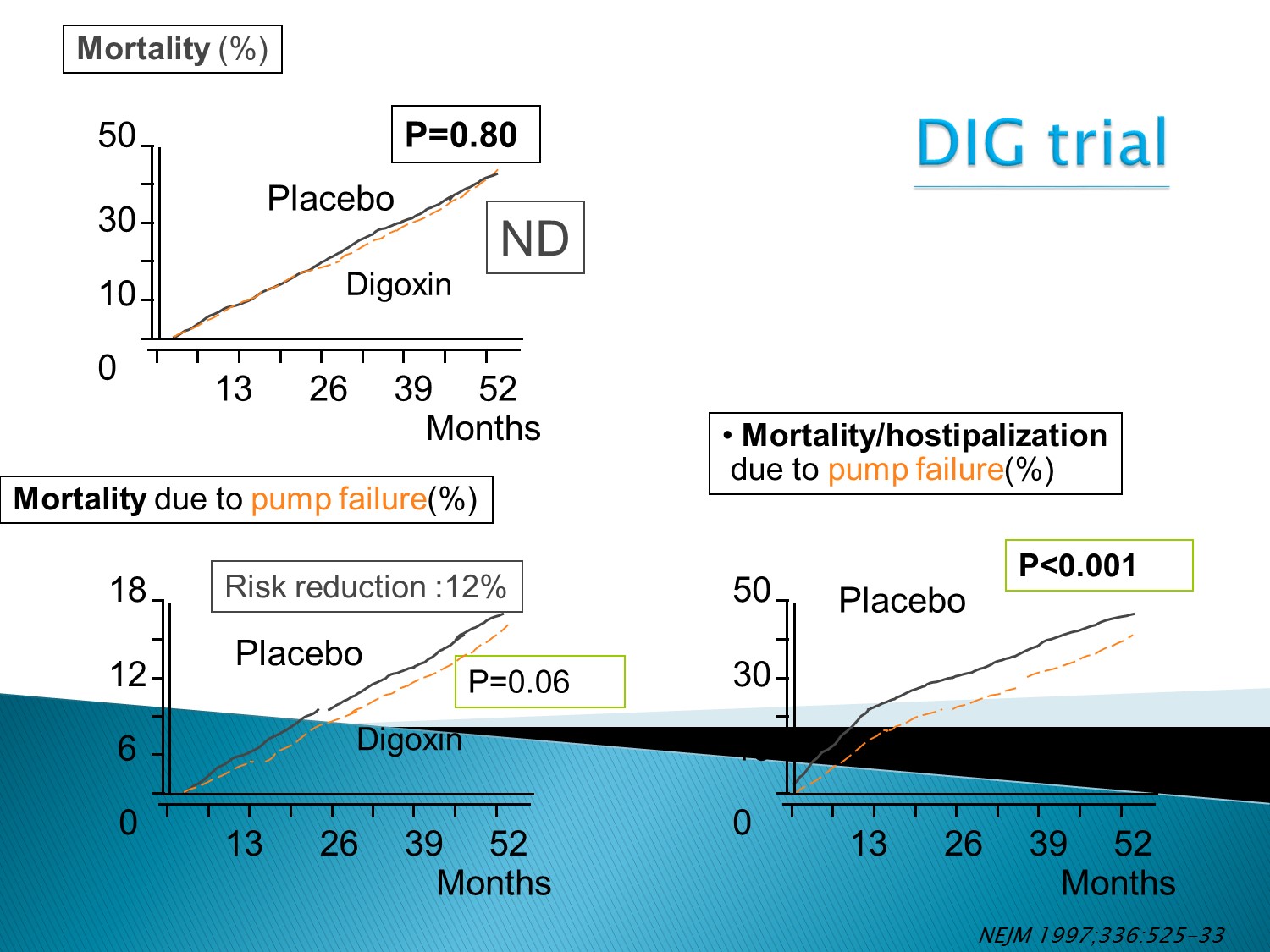
Digoxin對減少住院率有幫助
但對死亡率沒幫助
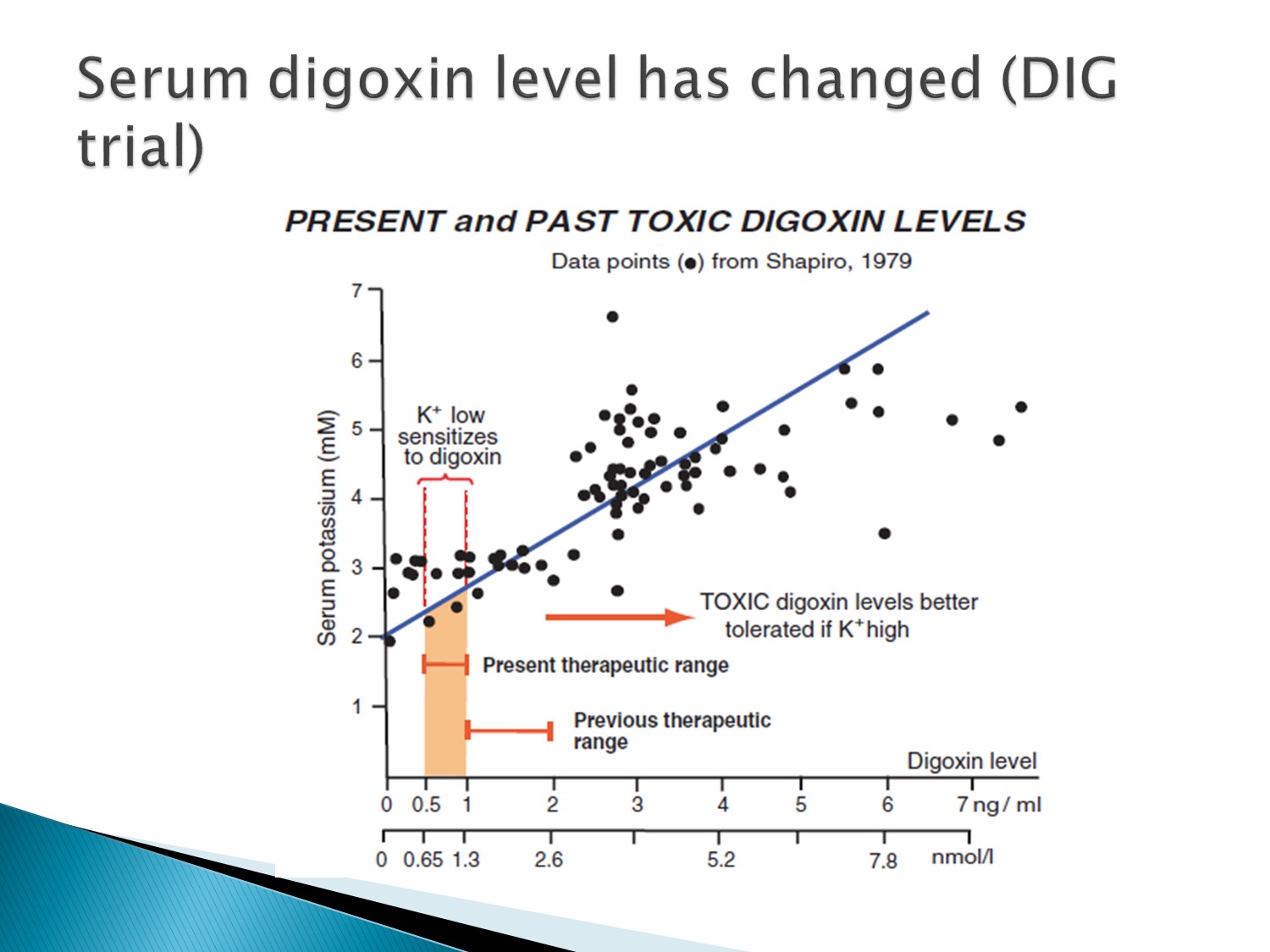
Therapeutic range是 0.5~1才正確
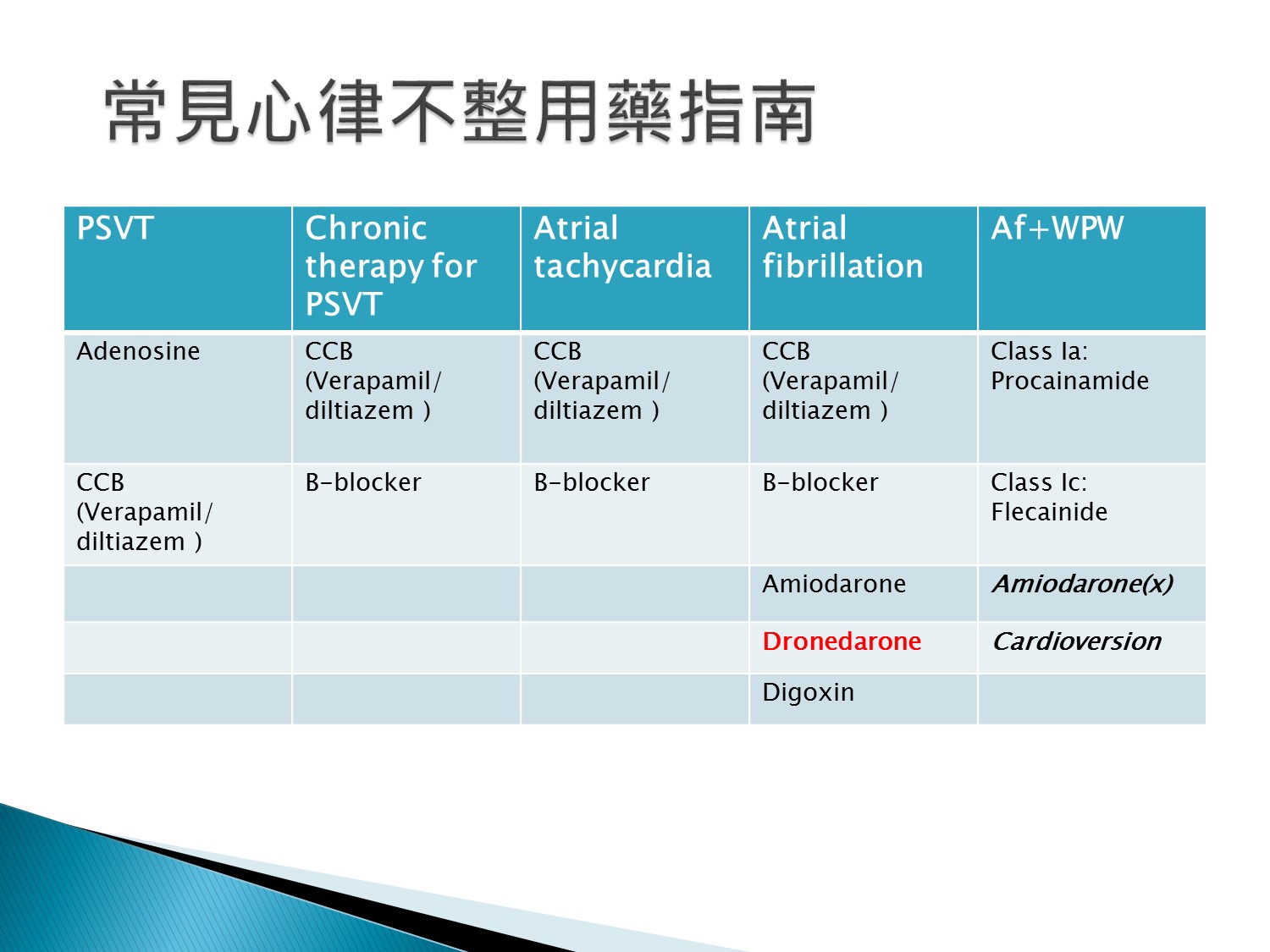
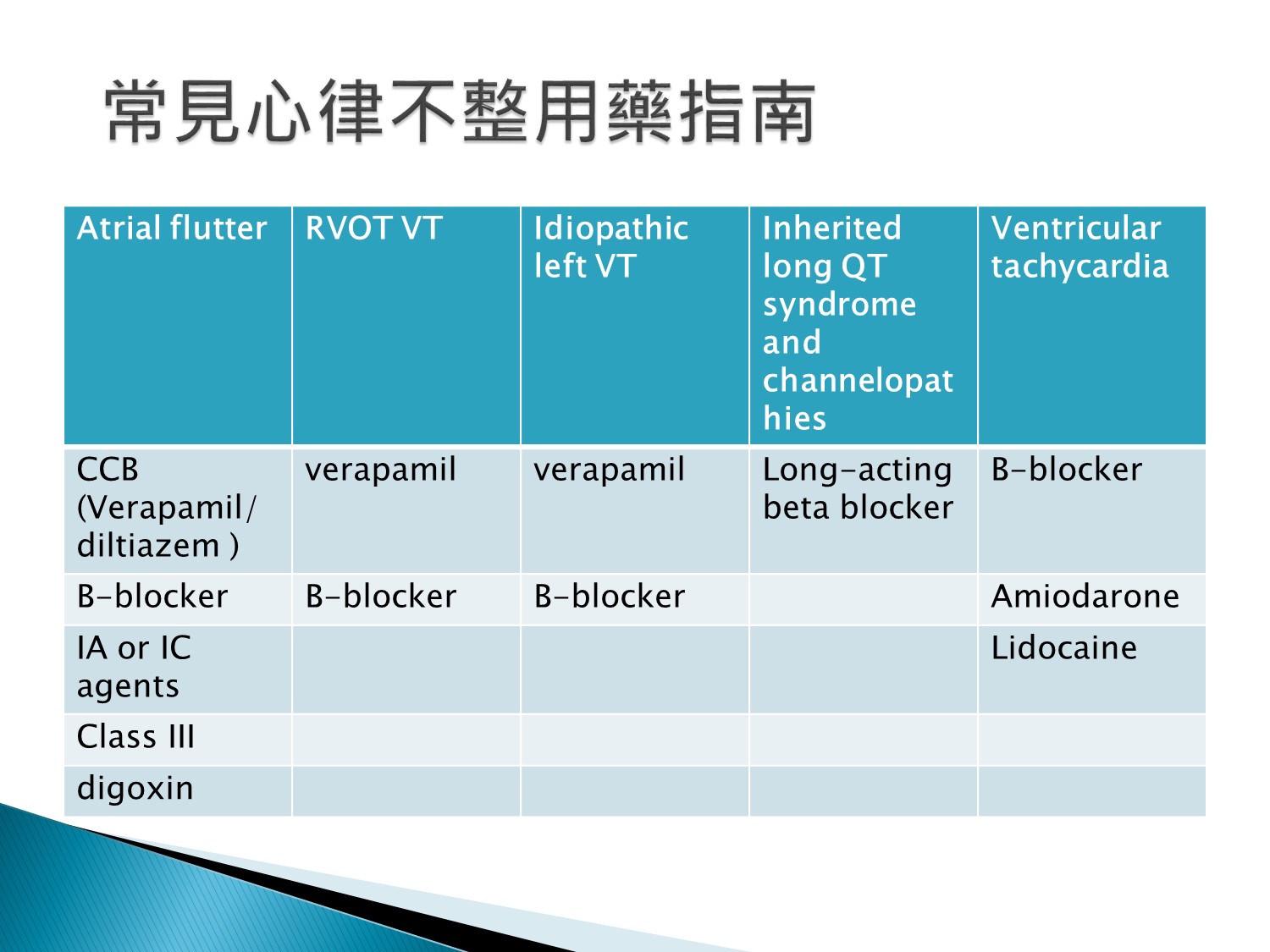
PSVT:先用adenosine,有些就被終止了
Af+WPW不能用AV blocker,只能用Ia、Ic
辨異:
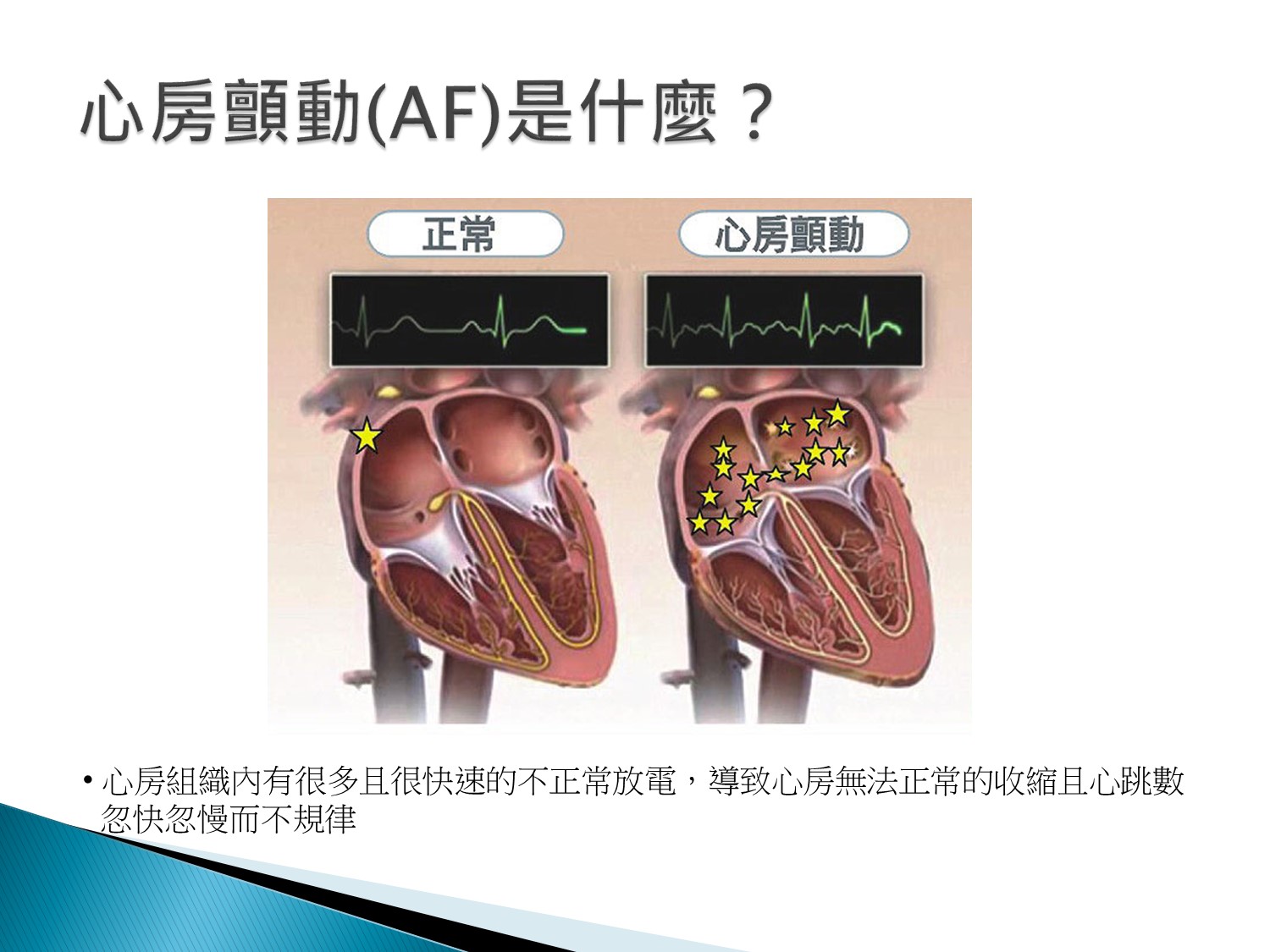
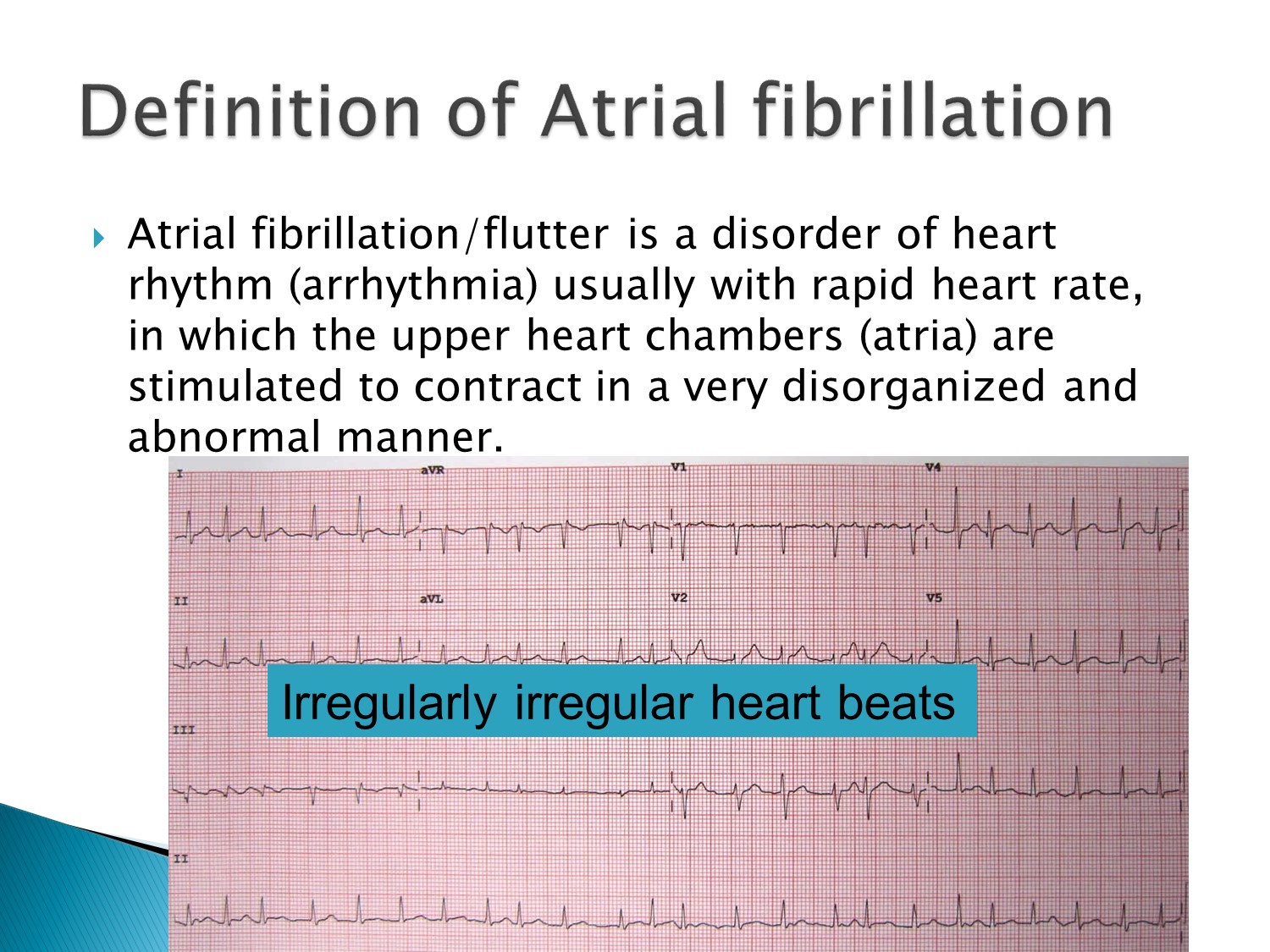
Irregularly irregular:例:Atrial fibrillation
Regularly irregular:例:幾個sinus+APC
以下為林廷遠醫師ppt檔案原本就有的內容:
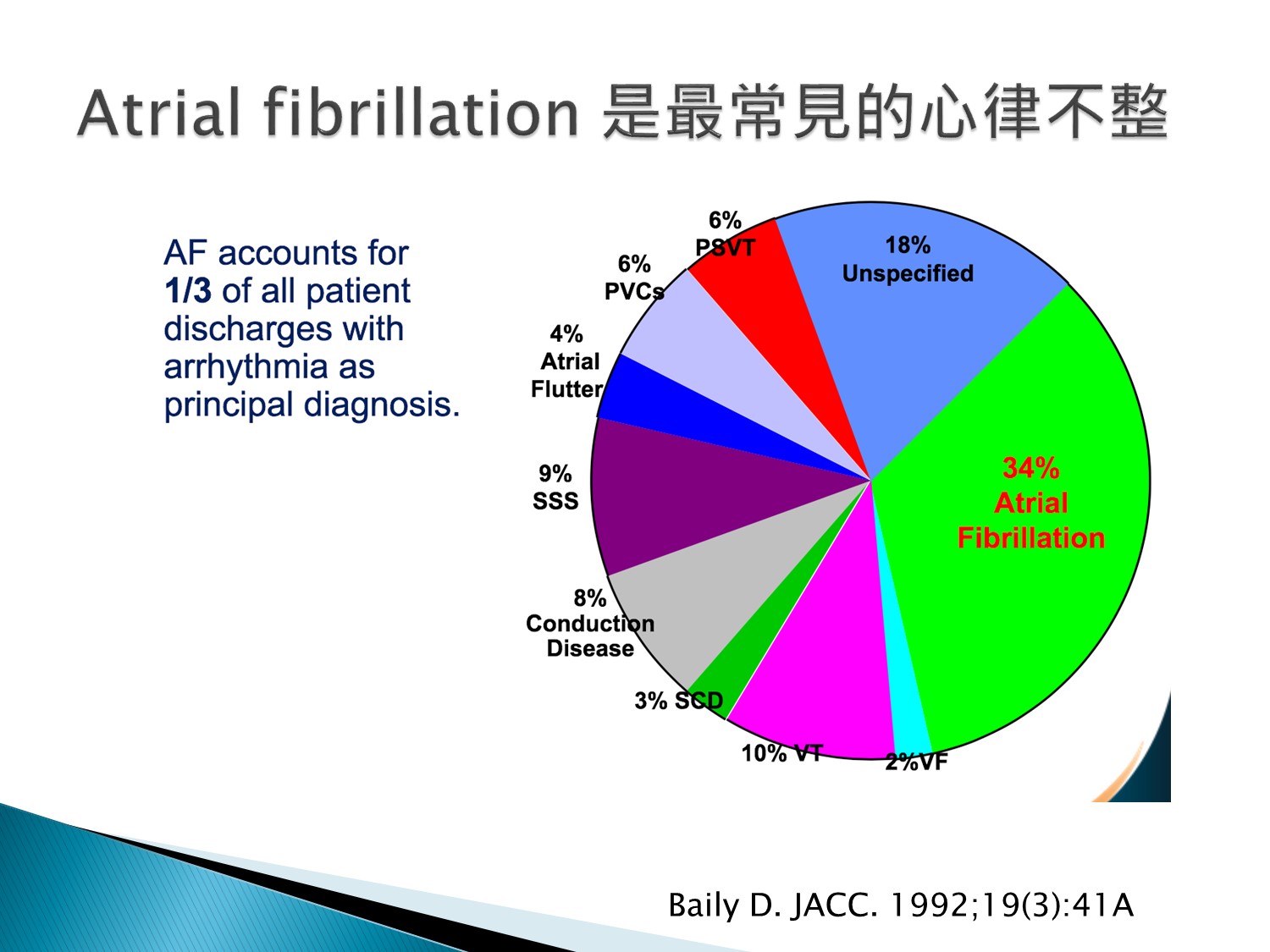
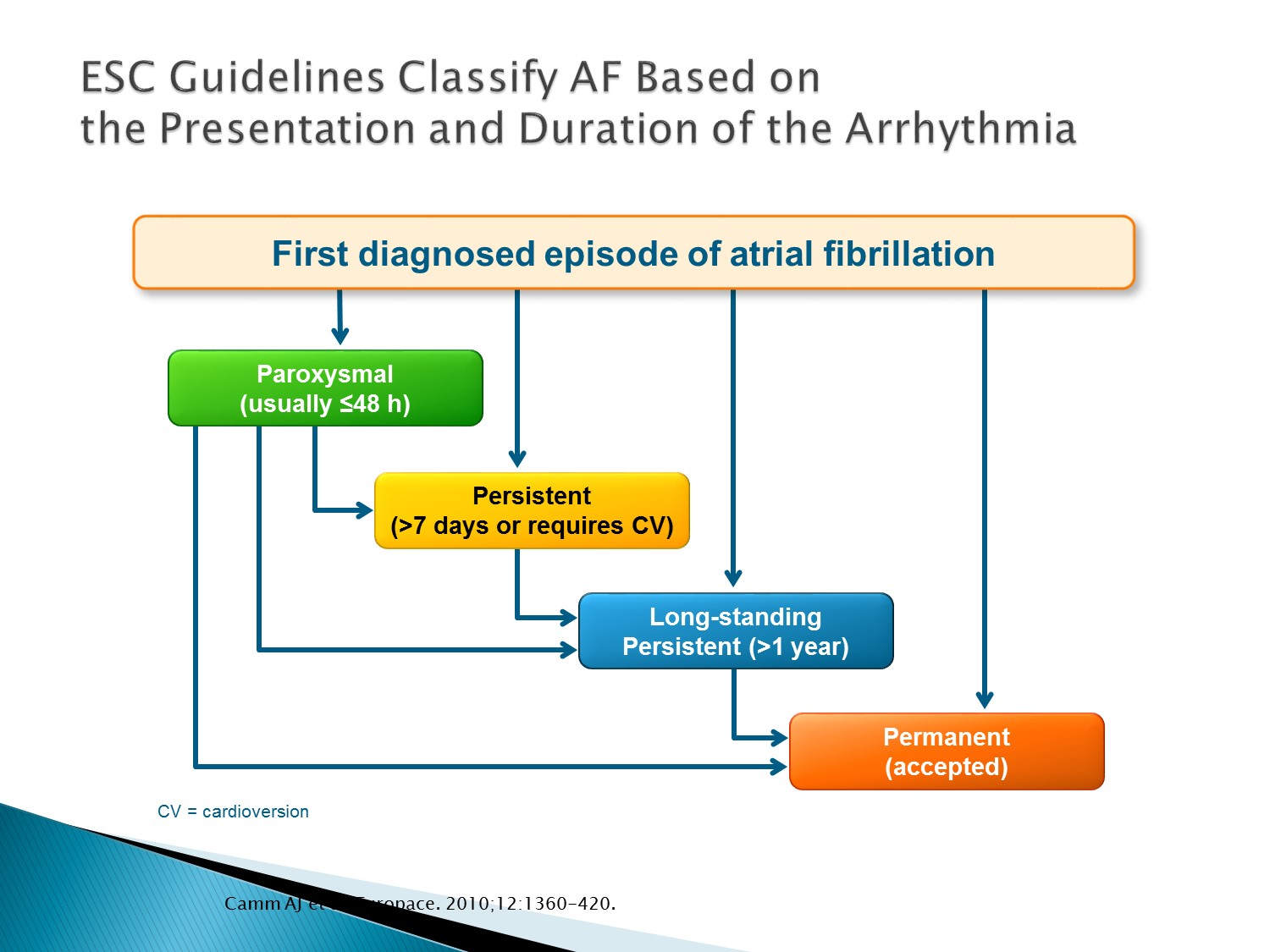
- Every patient who presents with AF for the first time is considered a patient with first diagnosed AF, irrespective of the duration of the arrhythmia or the presence and severity of AF-related symptoms.
- Paroxysmal AF is self-terminating, usually within 48 h. Although AF paroxysms may continue for up to 7 days, the 48 h time point is clinically important—after this the likelihood of spontaneous conversion is low and anticoagulation must be considered (see Section 4.1).
- Persistent AF is present when an AF episode either lasts longer than 7 days or requires termination by cardioversion, either with drugs or by direct current cardioversion (DCC).
- Long-standing persistent AF has lasted for ≥1 year when it is decided to adopt a rhythm control strategy.
- Permanent AF is said to exist when the presence of the arrhythmia is accepted by the patient and physician. Hence, rhythm control interventions are, by definition, not pursued in patients with permanent AF. Should a rhythm control strategy be adopted, the arrhythmia is redesignated as ‘long-standing persistent AF
- Silent AF (asymptomatic) may manifest as an AF-related complication (ischaemic stroke or tachycardiomyopathy) or may be diagnosed by an opportunistic ECG. Silent AF may present as any of the temporal forms of AF.
Reference
Adapted from Camm J, et al. Europace. 2010;12:1360-420
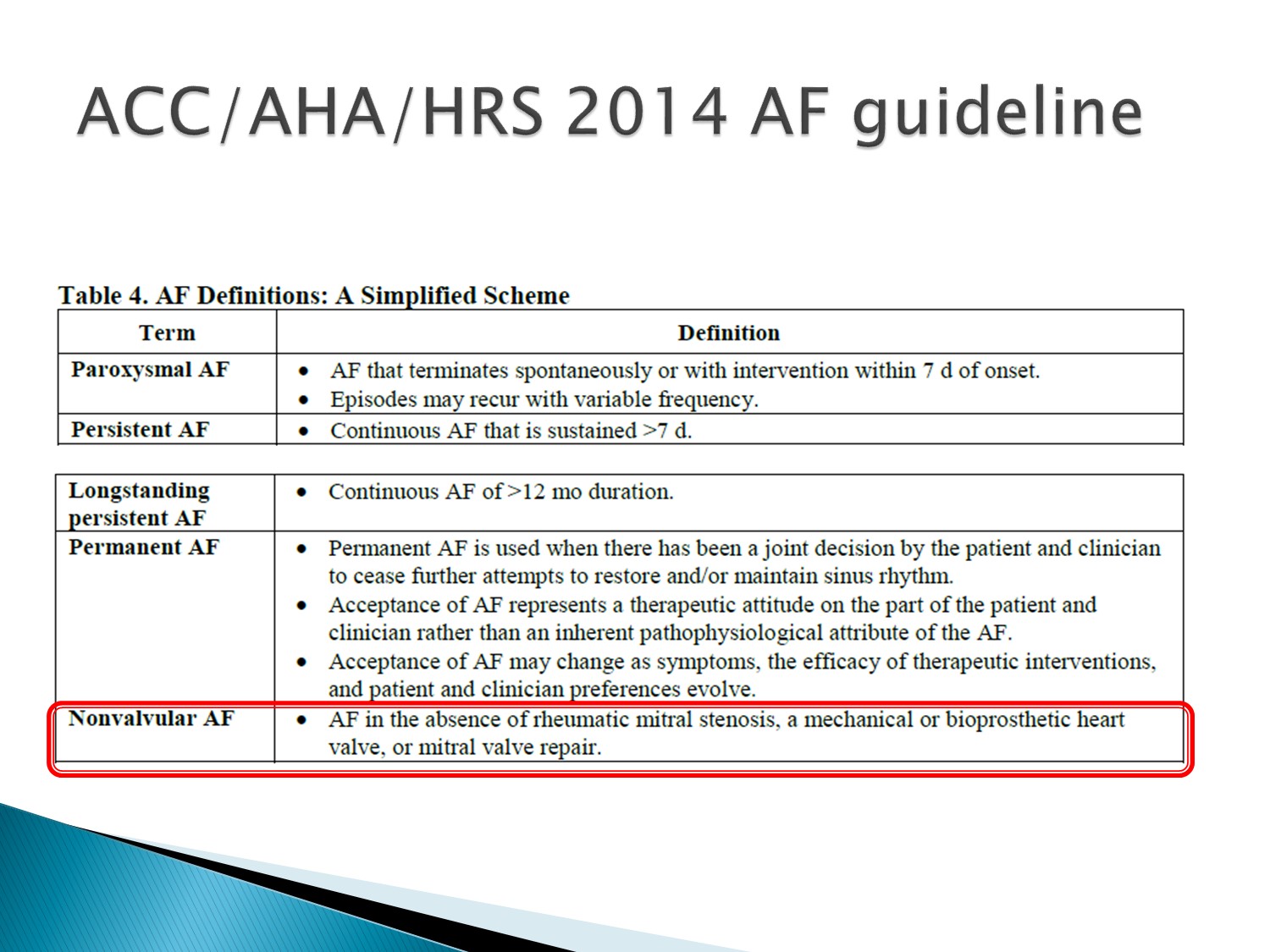
Non-valvular A fib:才能用 NOAC(沒 rheumatic MS、沒換過 valve)
以下為林廷遠醫師ppt檔案原本就有的內容:
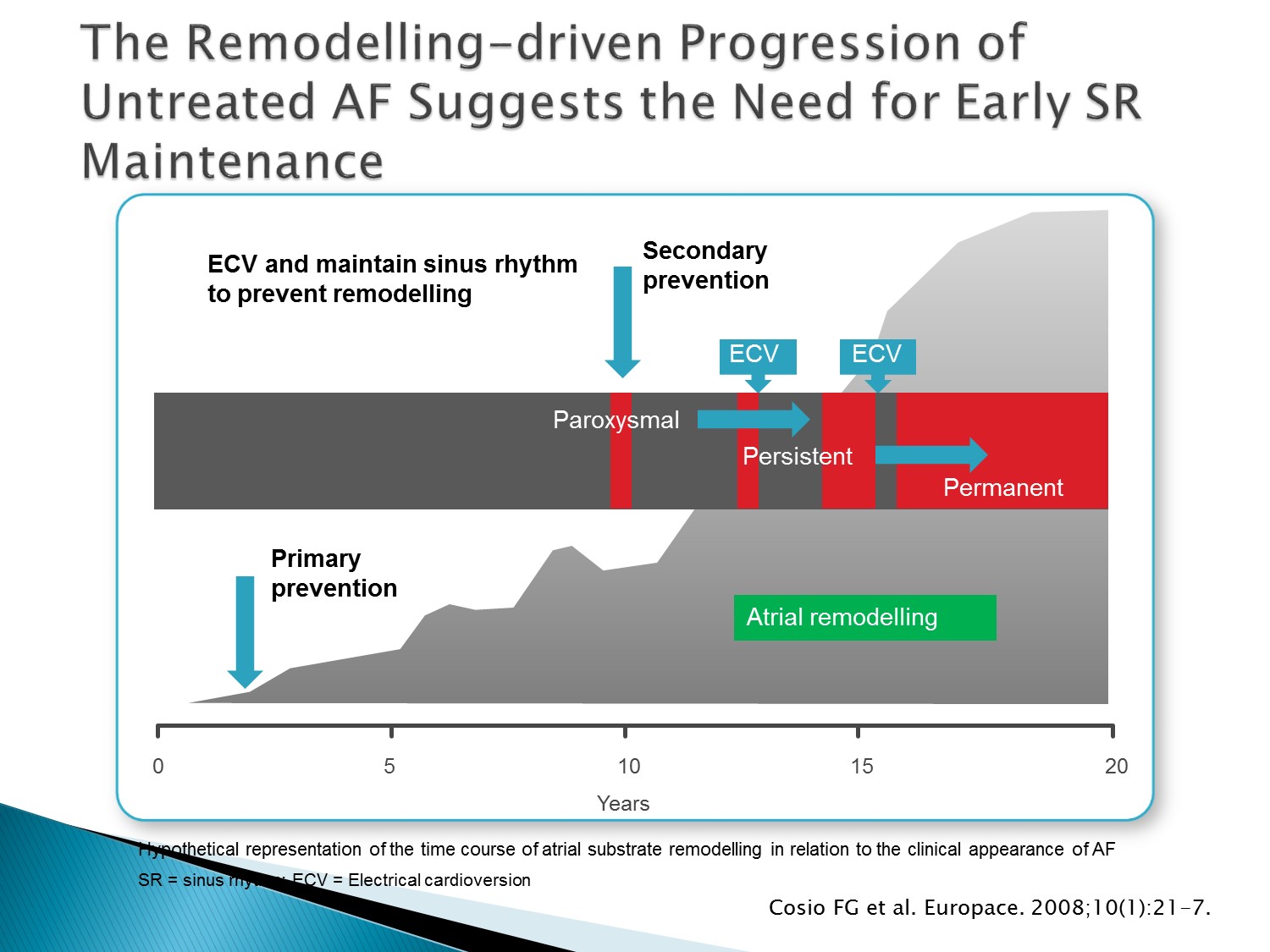
- Cosio et al. have proposed a hypothetical representation of the time course of atrial substrate remodelling in relation to the clinical appearance of AF and possible interventions to slow or arrest the remodelling process
- A dual strategy of early treatment of AF that includes rhythm control as well as aggressive detection and management of associated conditions may help to prevent electrical and structural remodelling and provide a window of opportunity to arrest the progression or even revert the arrhythmogenic changes in the atria
Reference
Adapted from Cosio FG, et al. Europace. 2008;10(1):21-7
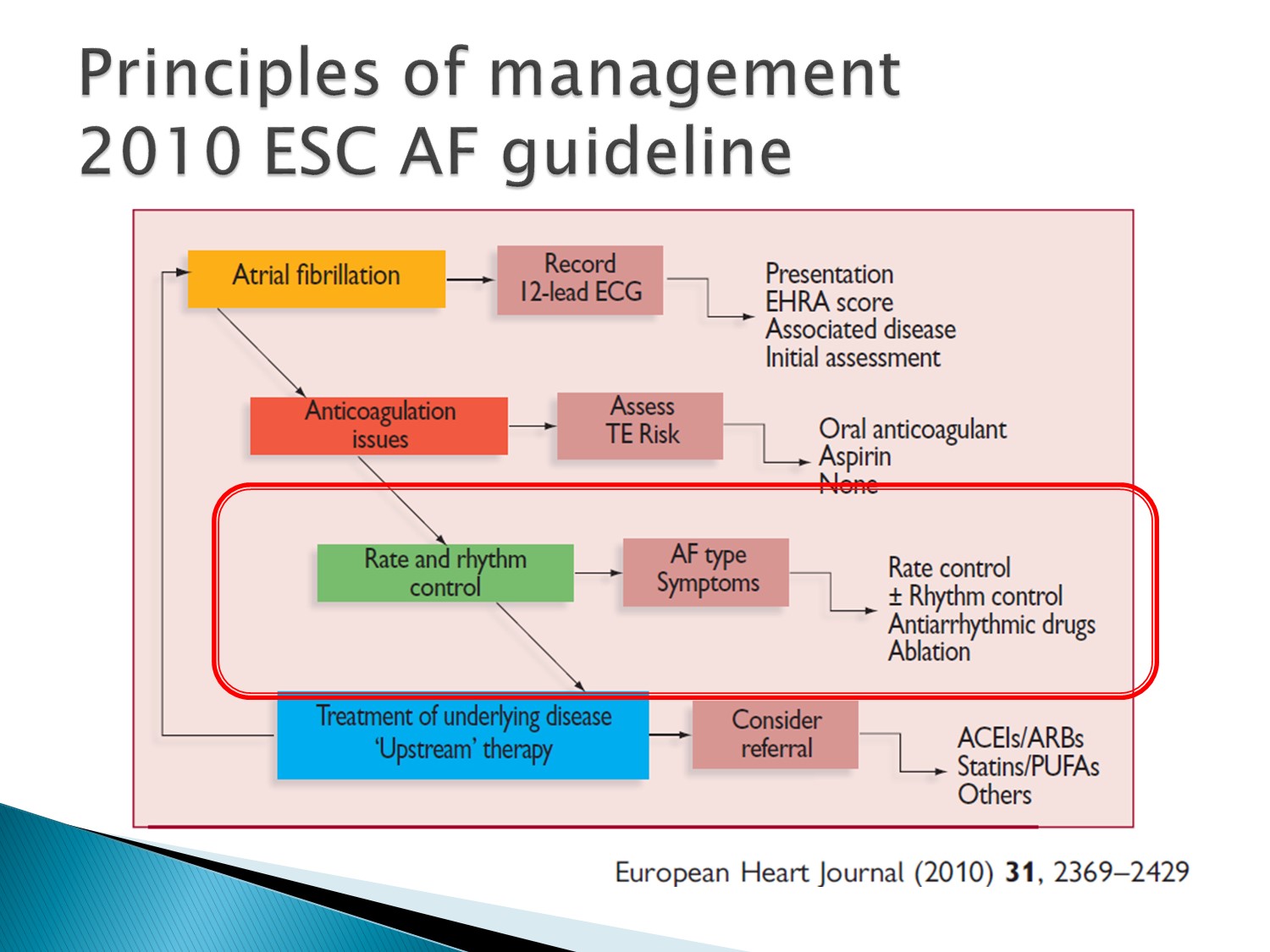
以下為林廷遠醫師ppt檔案原本就有的內容:
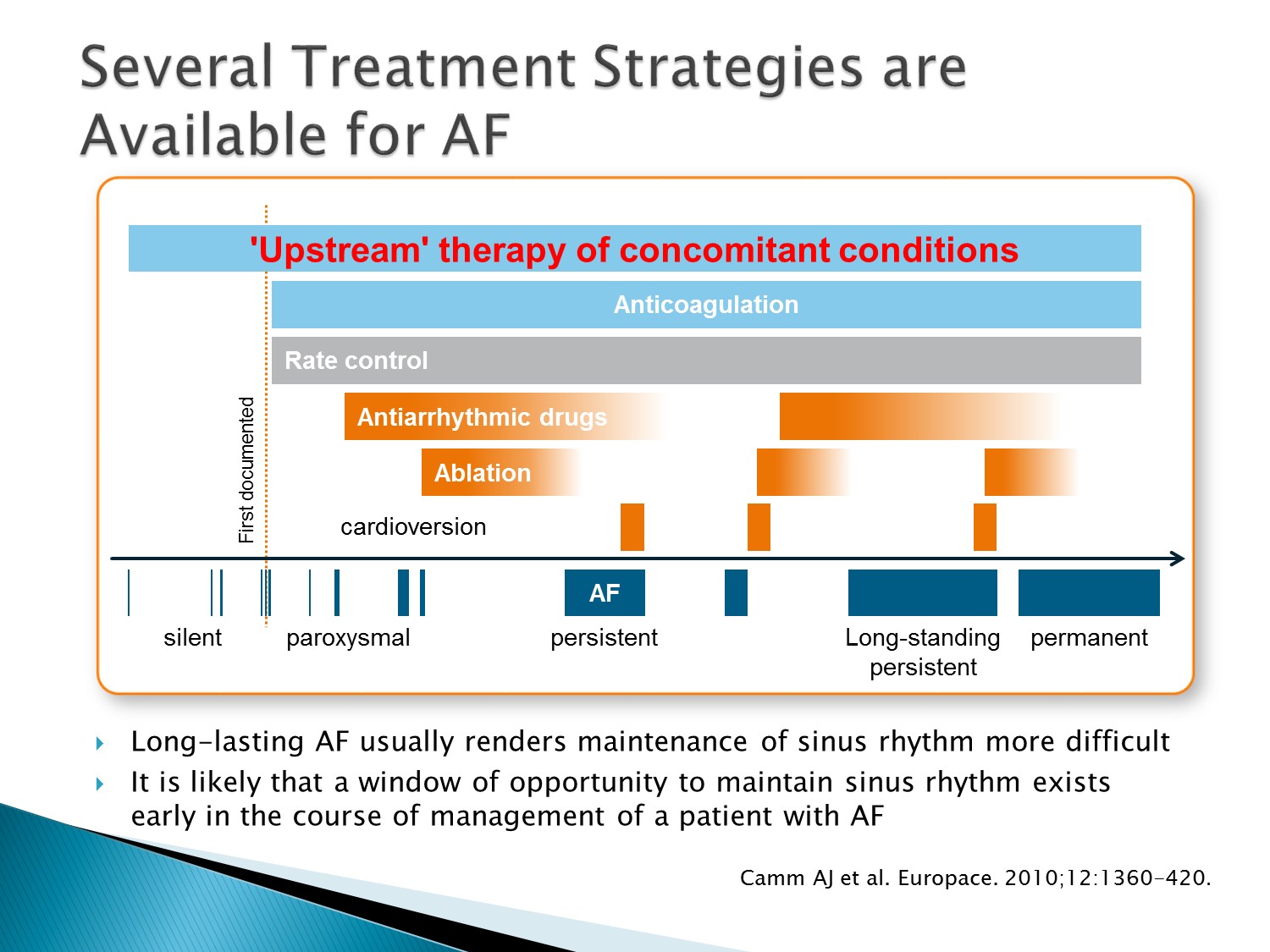
- This schematic is taken from the 2010 ESC AF guidelines and illustrates the treatment options available for the progressive stages of AF
- The upper bars above the blue arrow indicate therapeutic measures that could be pursued
- Light blue boxes indicate therapies that have proven effects on ‘hard outcomes’ in AF, such as stroke or acute heart failure
- Orange boxes indicate therapies that are currently used for symptom relief, but may in the future contribute to reduction of AF-related complications
- Rate control (grey box) is valuable for symptom relief and may improve cardiovascular outcomes
Reference
Adapted from Camm J, et al. Europace. 2010;12:1360-420
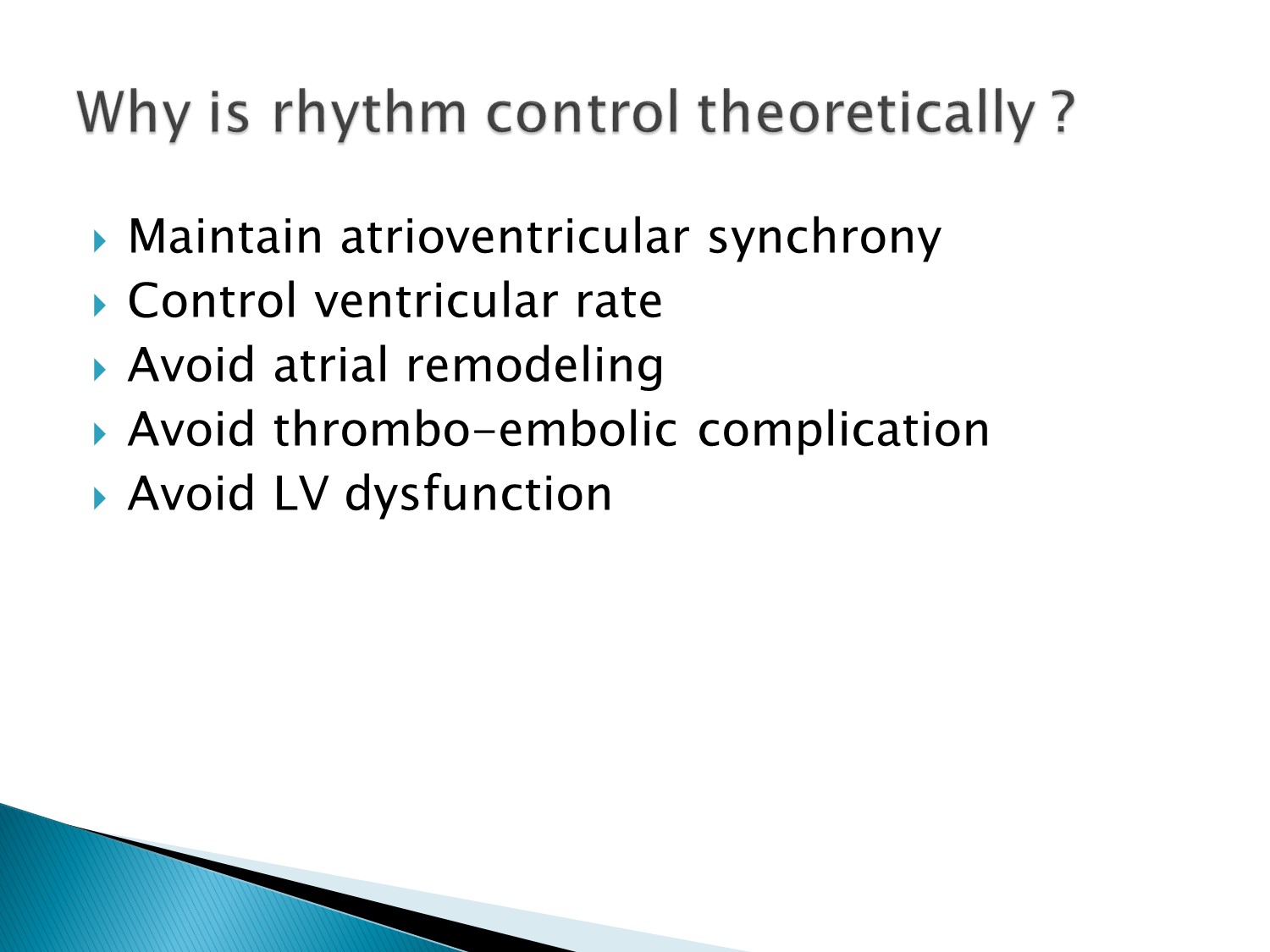
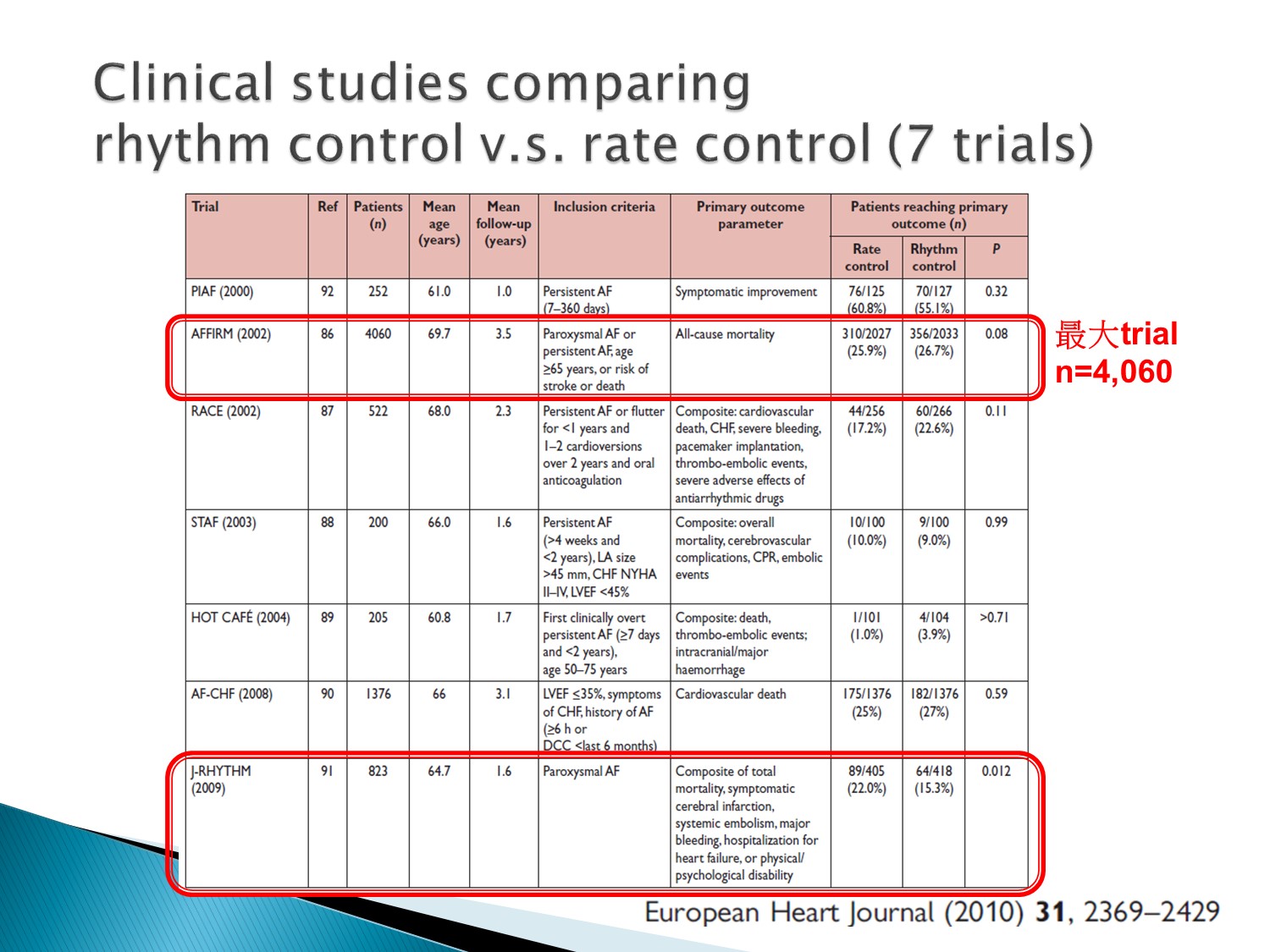
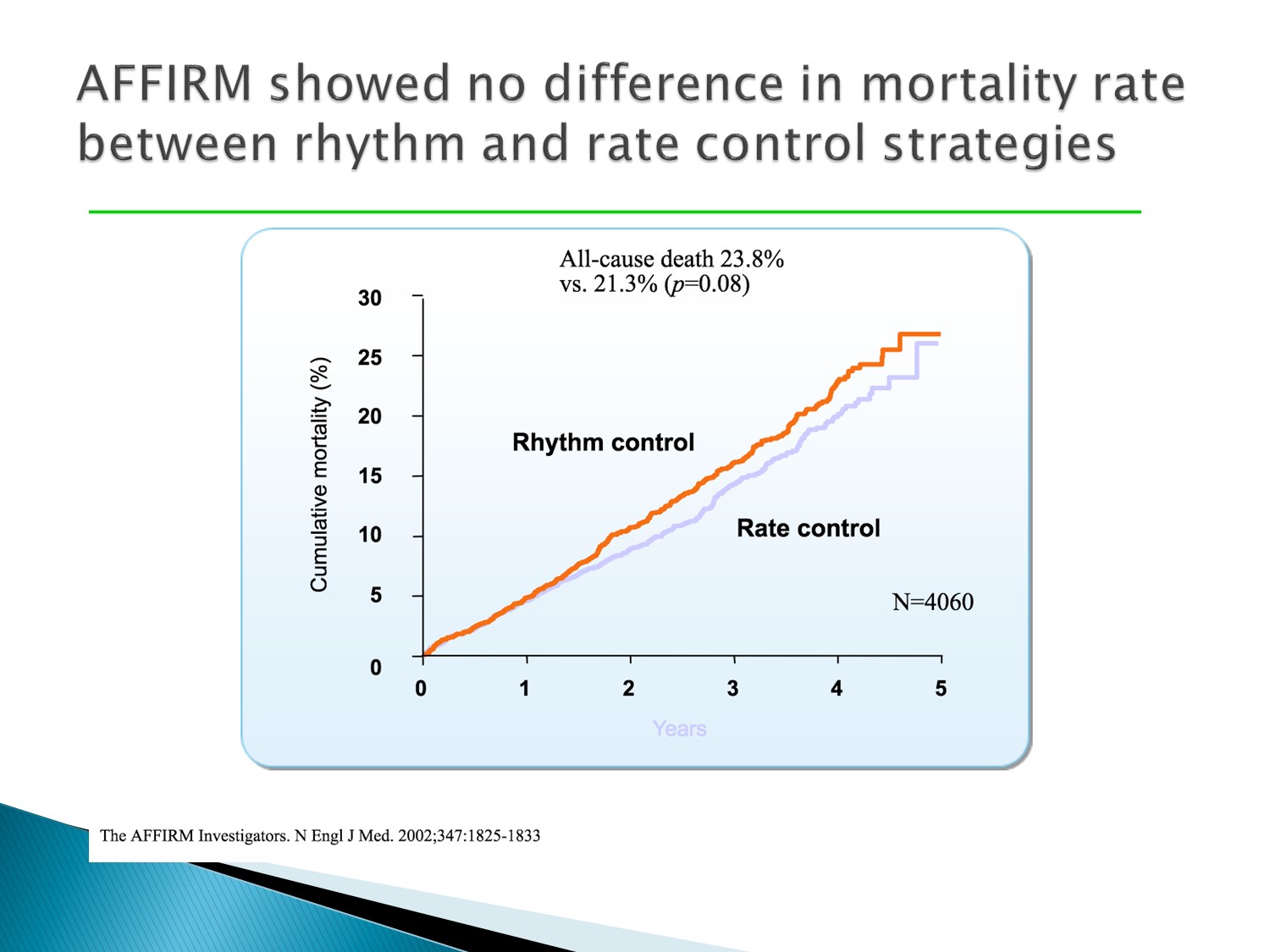
AFFIRM studies:
Rhythm control 及 rate contro l對 all cause mortality 沒有差異
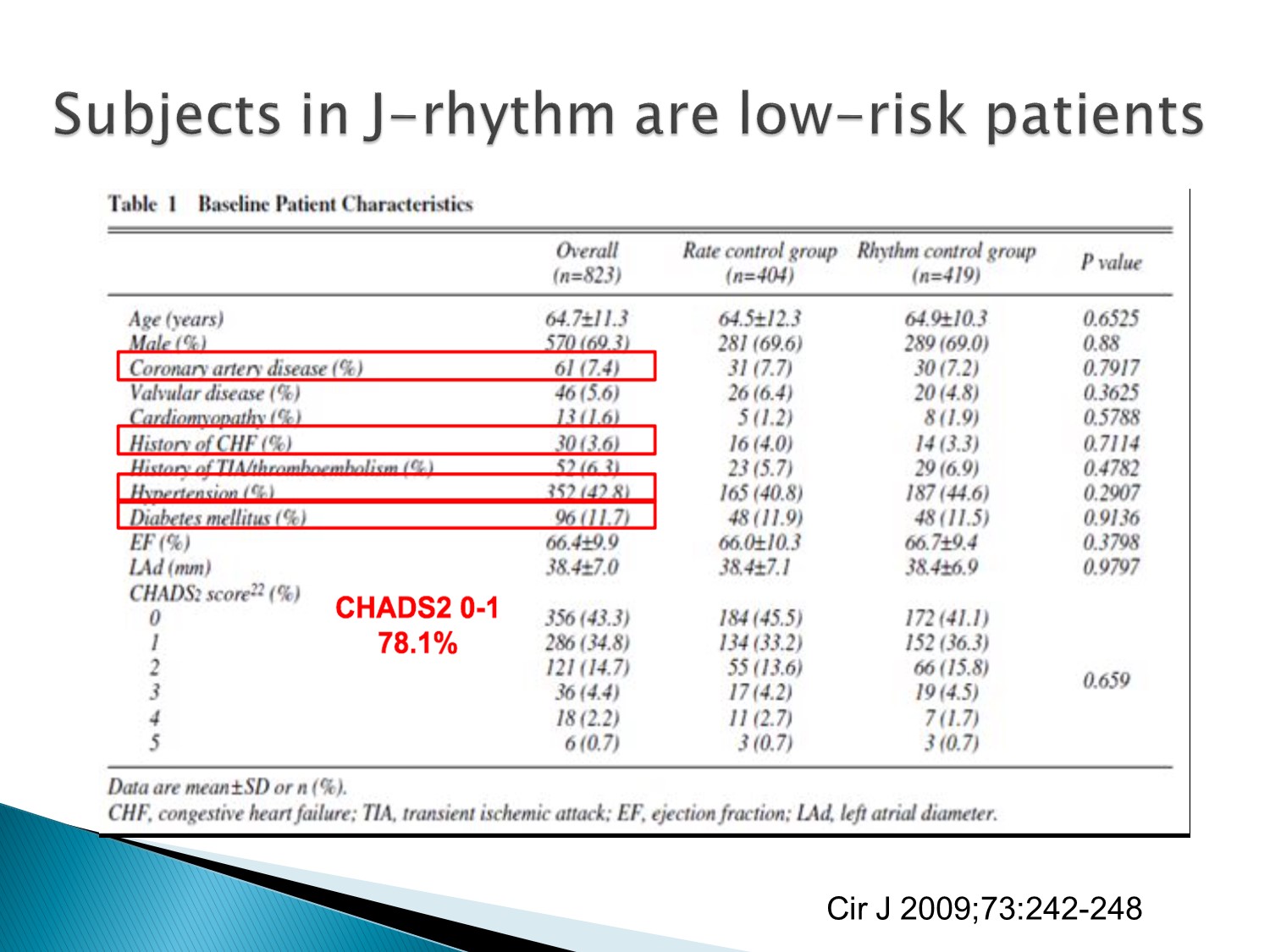
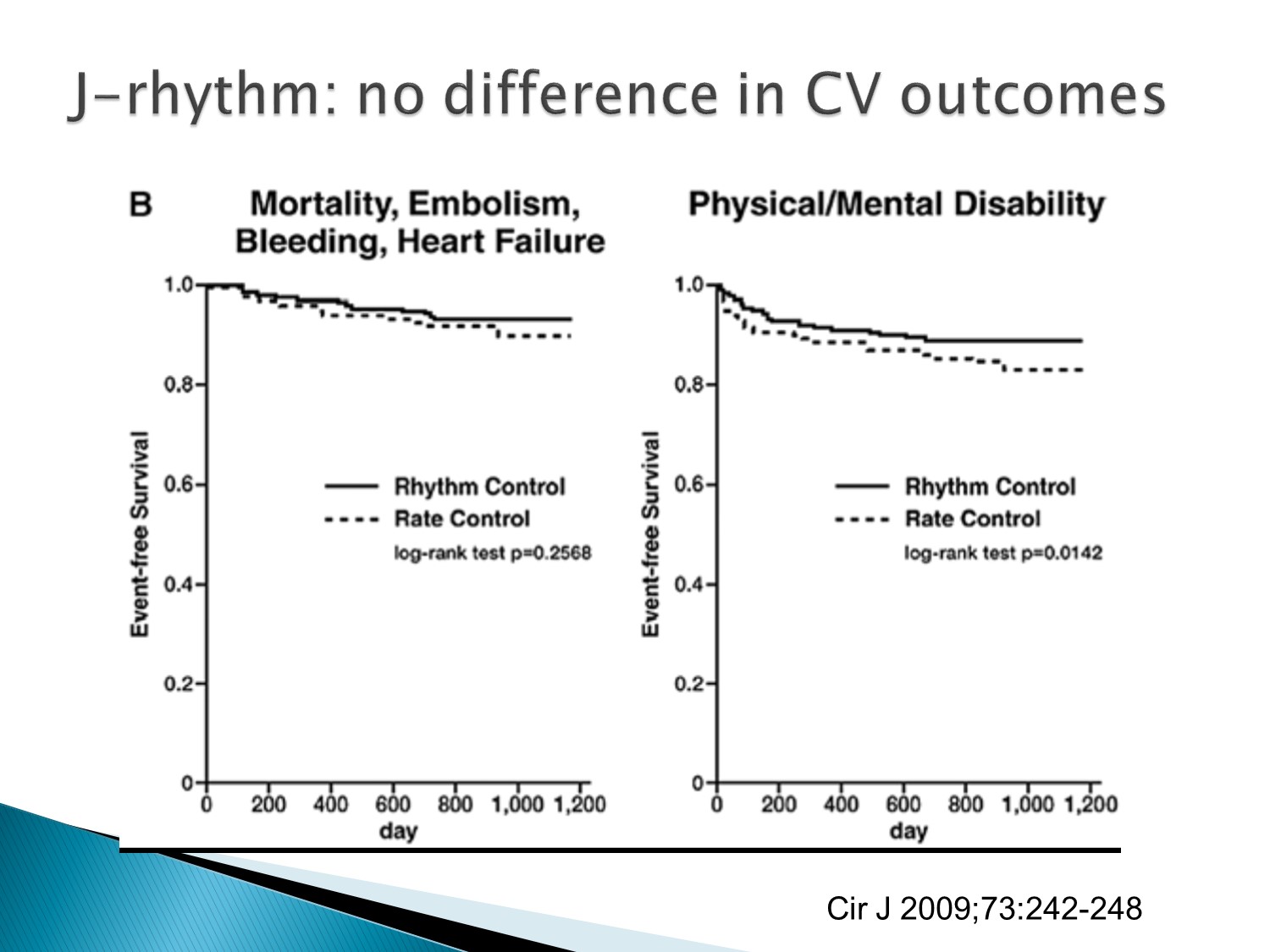
J rhythn studies:rhythm control 在 mortality 的表現較優。
但此 studies 的病患選擇普遍 CHADS2 score 較低分
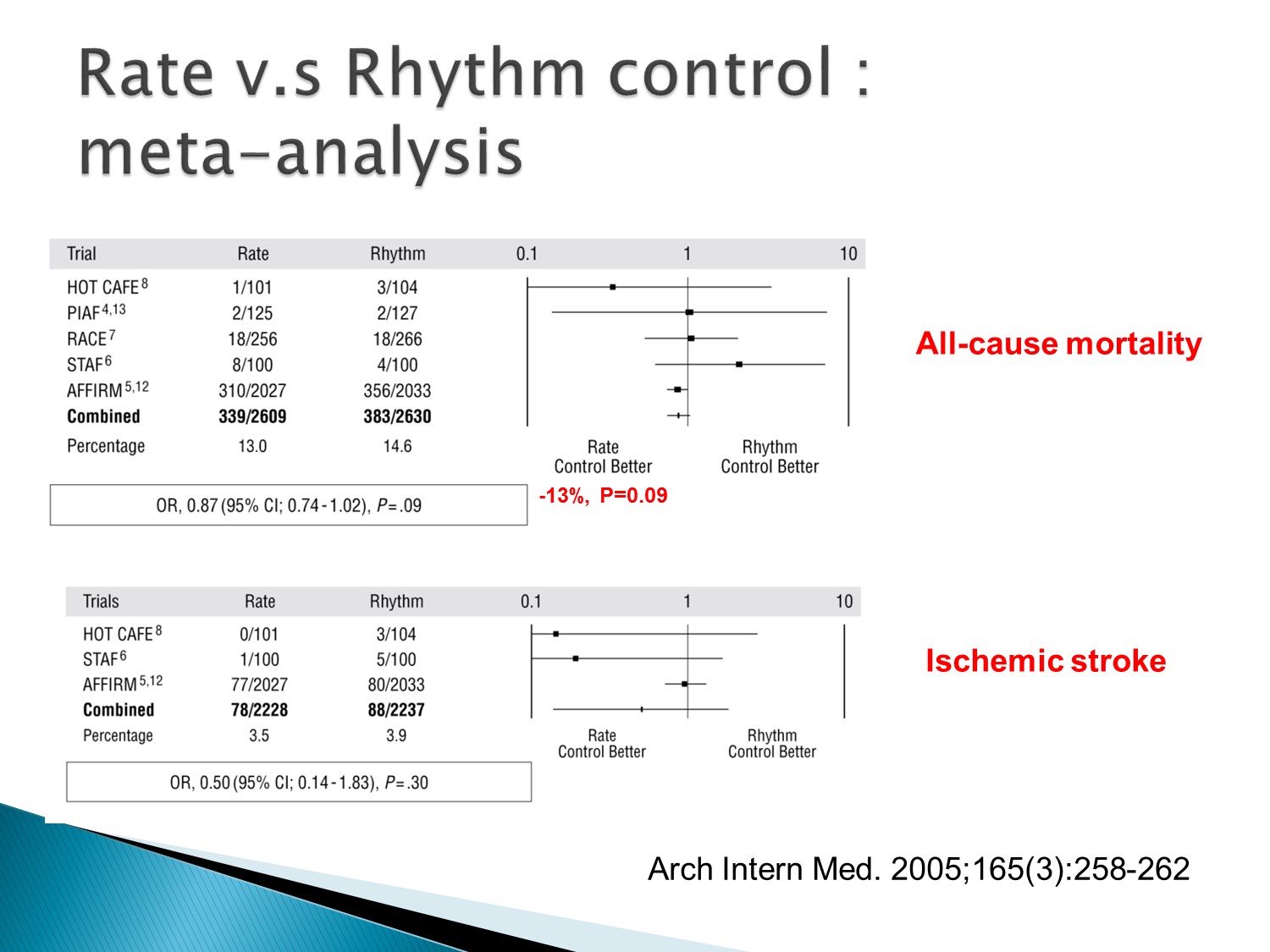
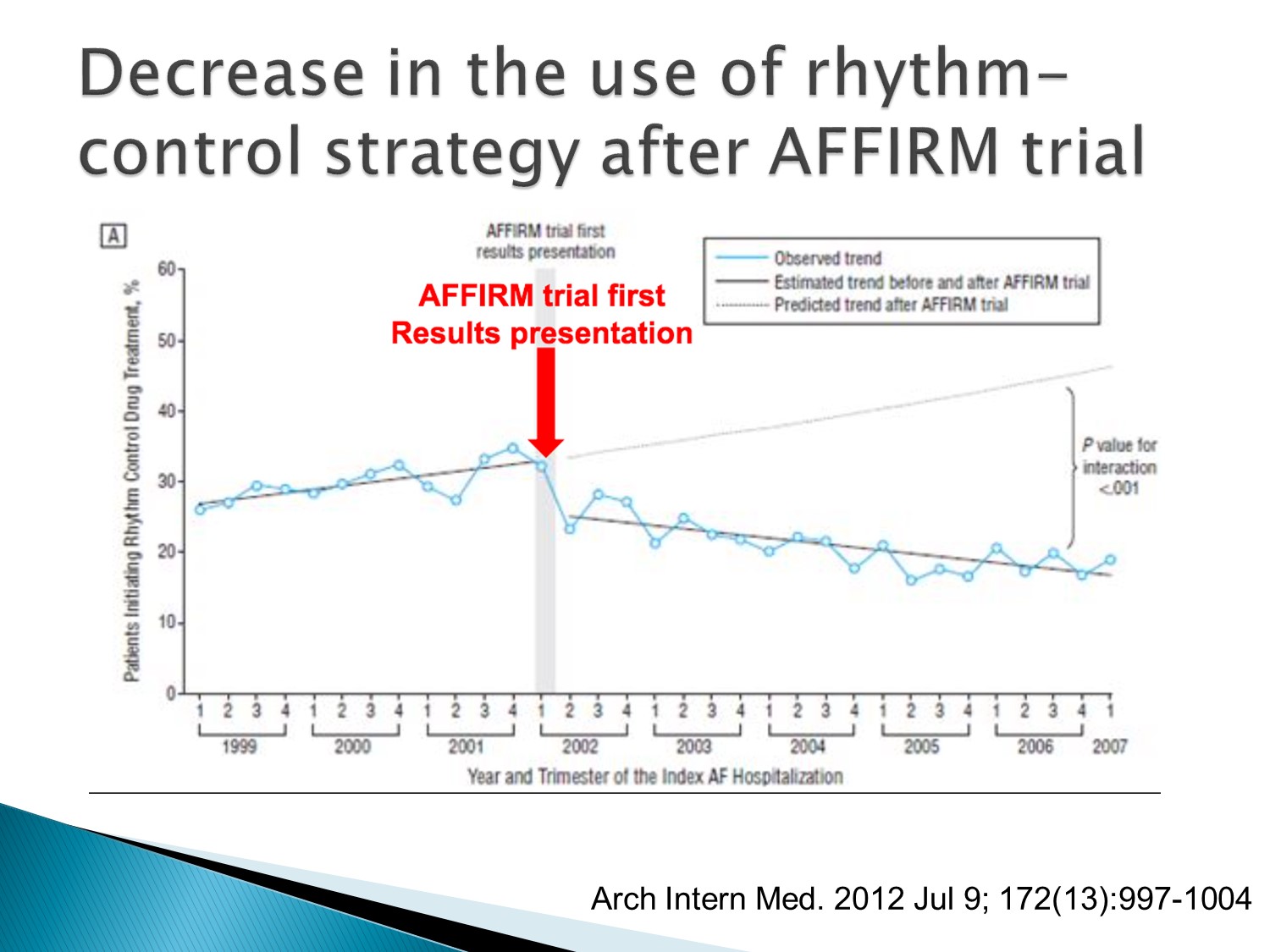
所以在 AFFIRM studies 後以 rate control 為主流
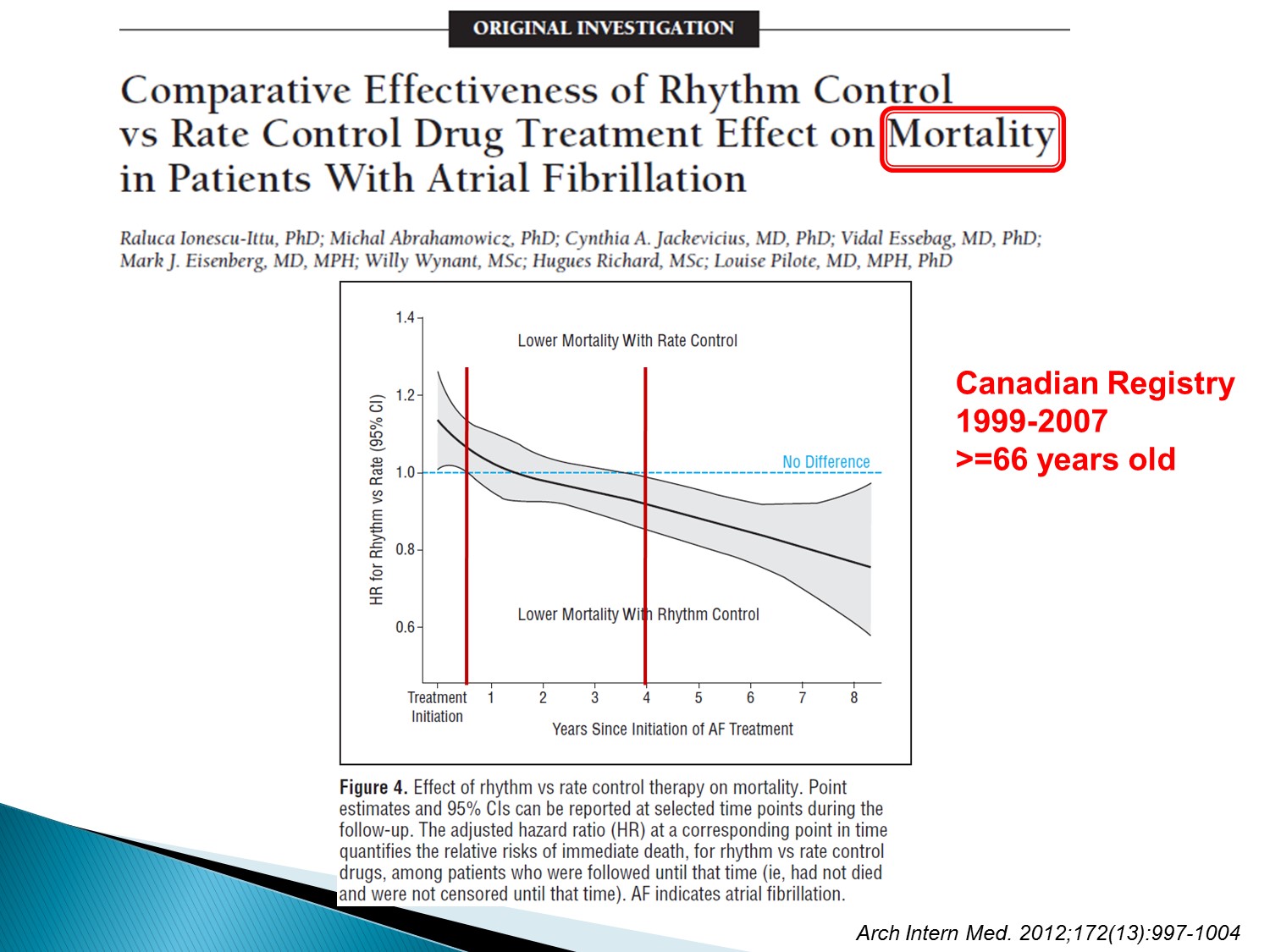
但是觀察時間若拉長,rhythm control似乎活得比較久
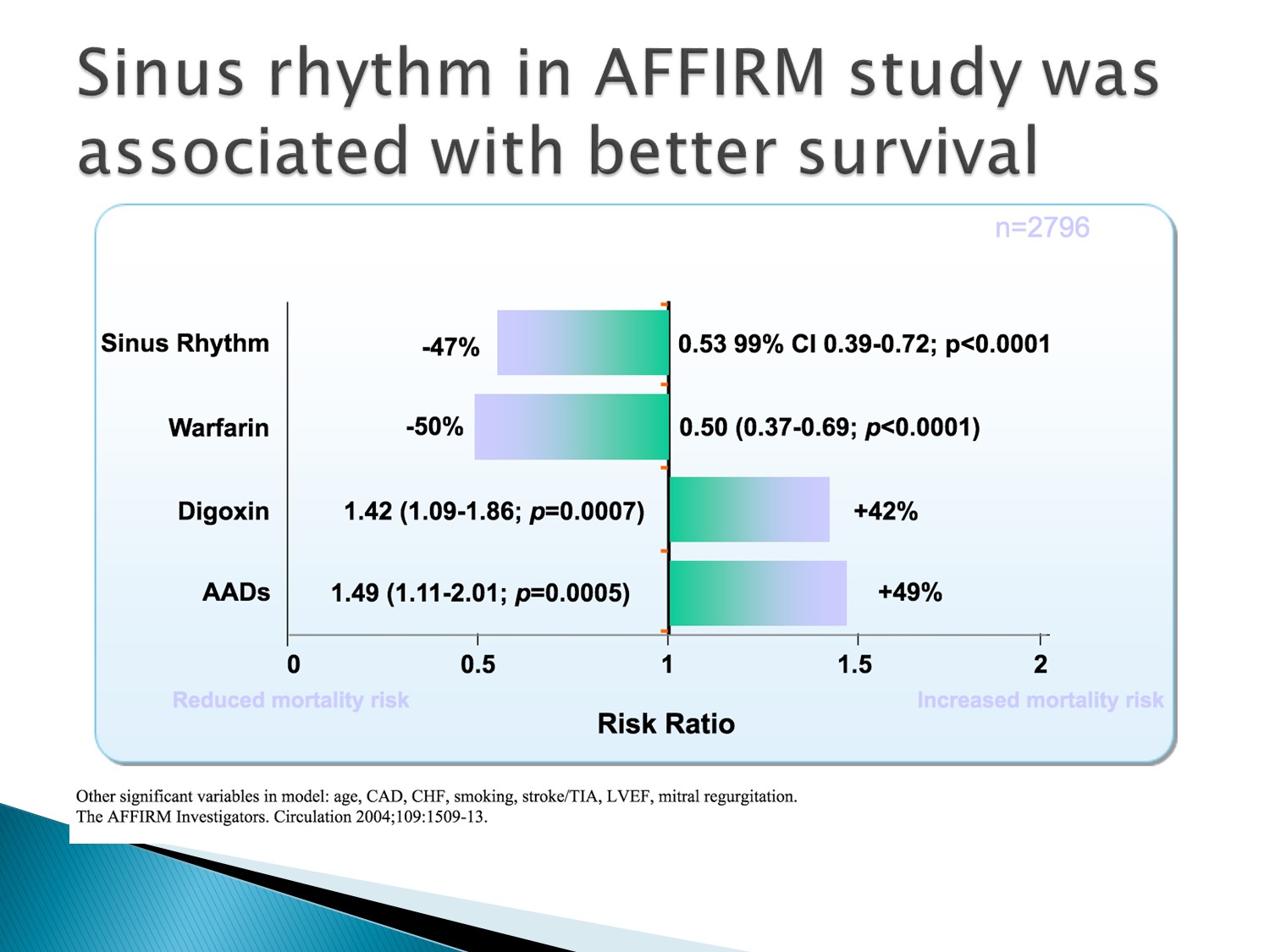
AFFIRM studies 裡,all-cause mortality 做不出差異的原因在於全部因素混在一起
若單獨看,sinus rhythm 的 survival 是較好的,造成 survival 差的部分在於 digoxin 及 anti-arrythmia drug 的使用增加了 mortality
綜合起來抵銷了 sinus rhythm 的效果
故原因在於藥物的使用不當
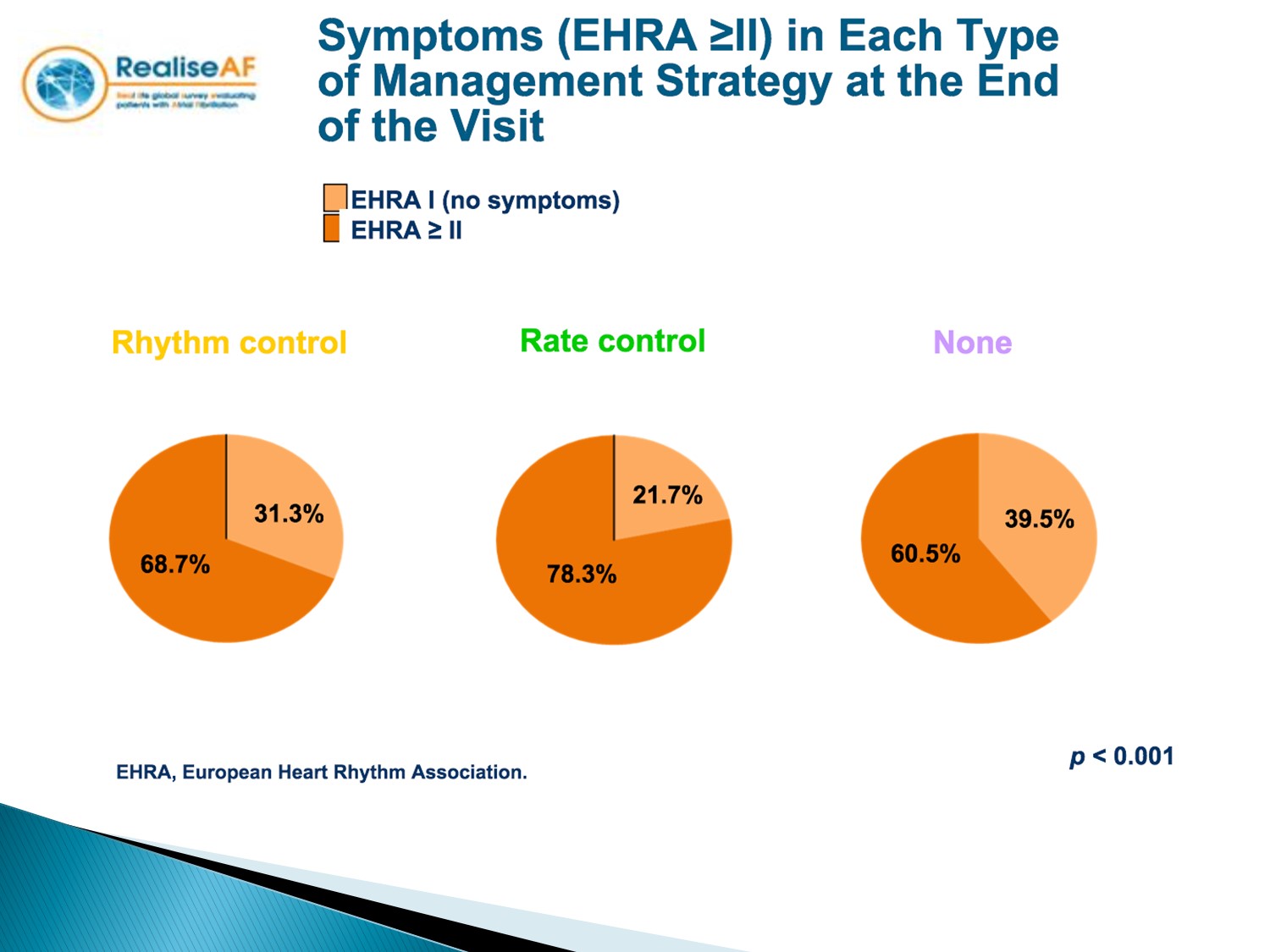
另外在 symptoms control 上,rhythm control 效果較佳
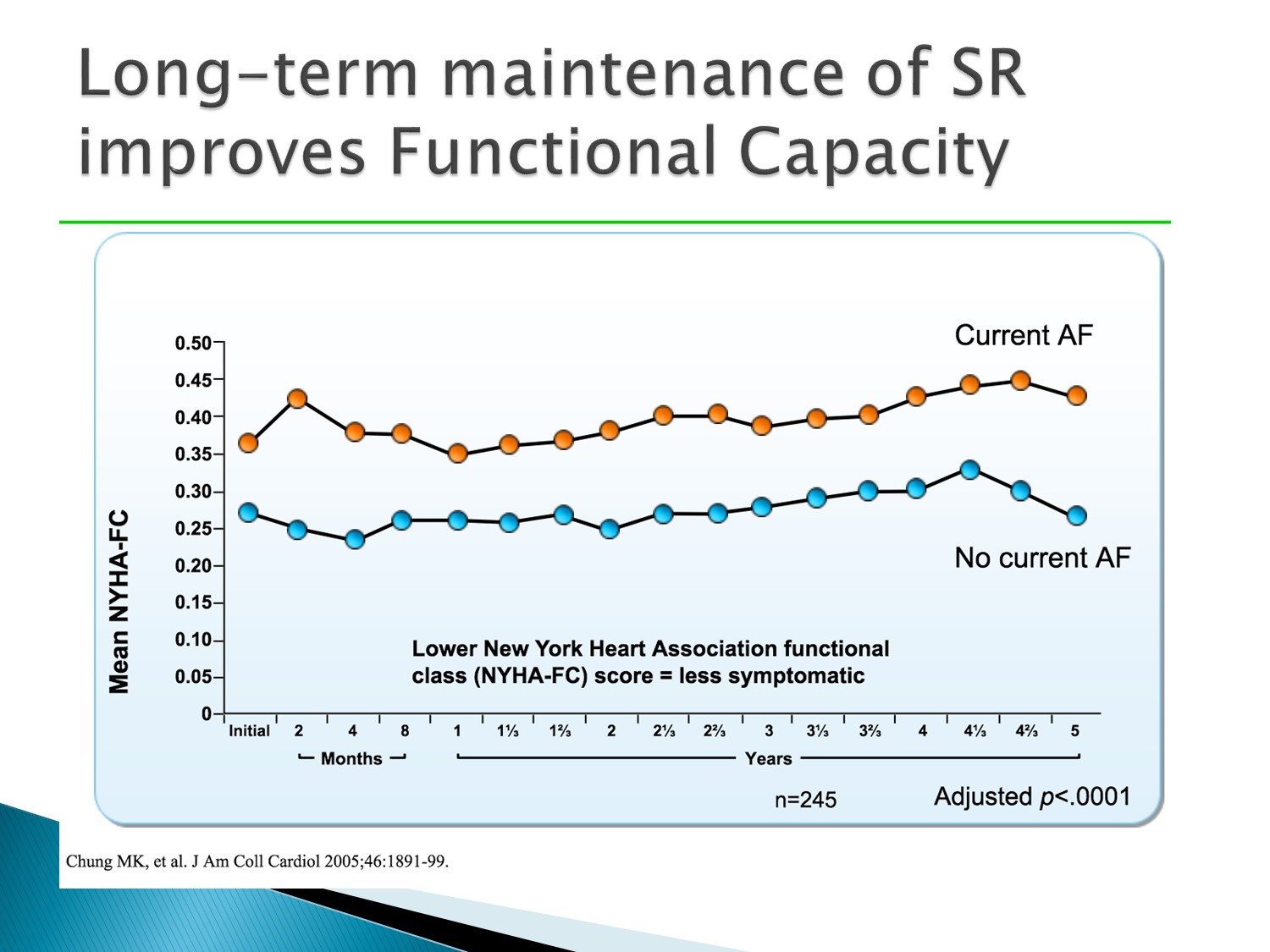
Functional capacity 的表現上,sinus rhythm 較佳
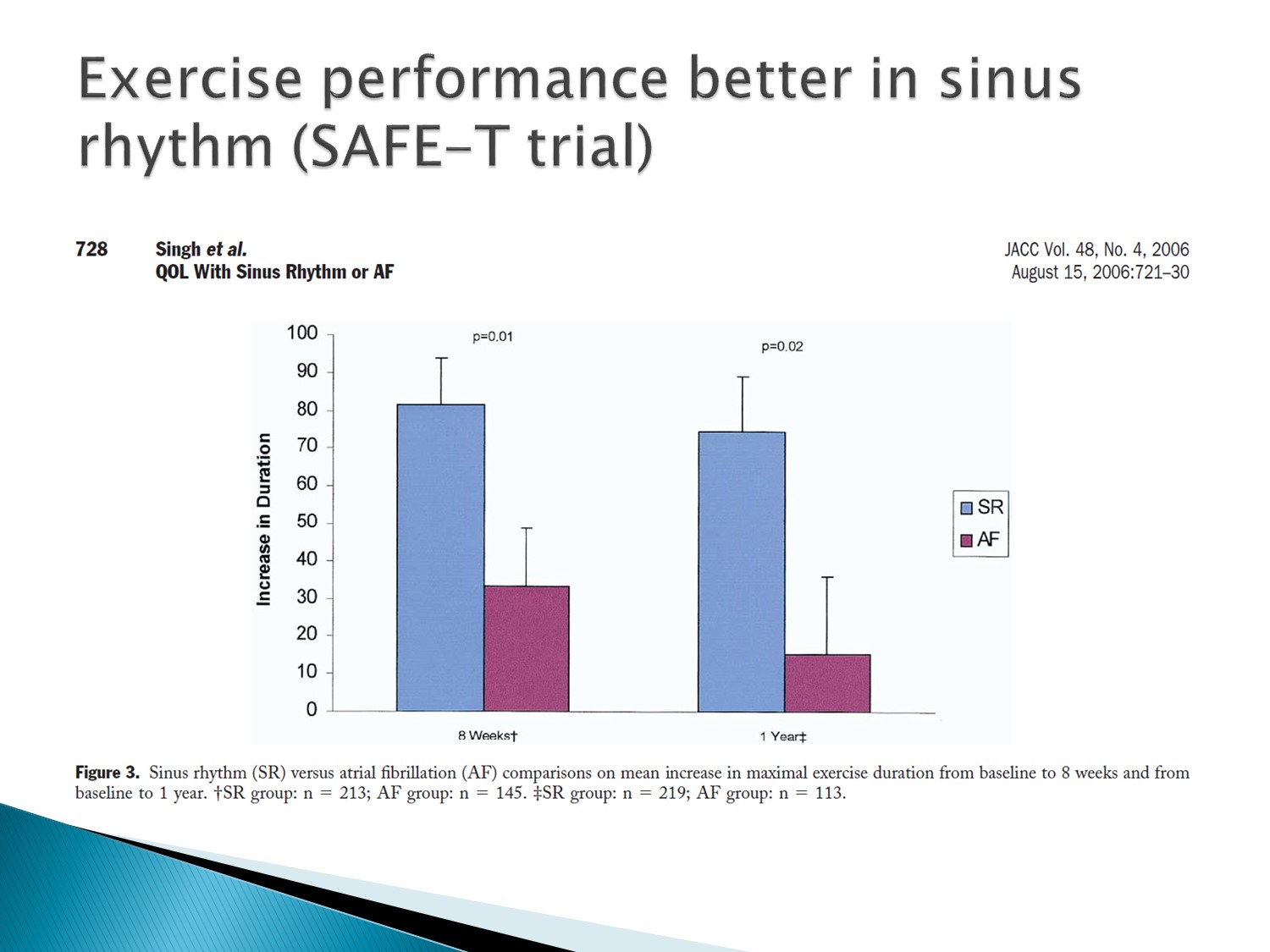
Exercise performance 表現上,sinus rhythm 較佳
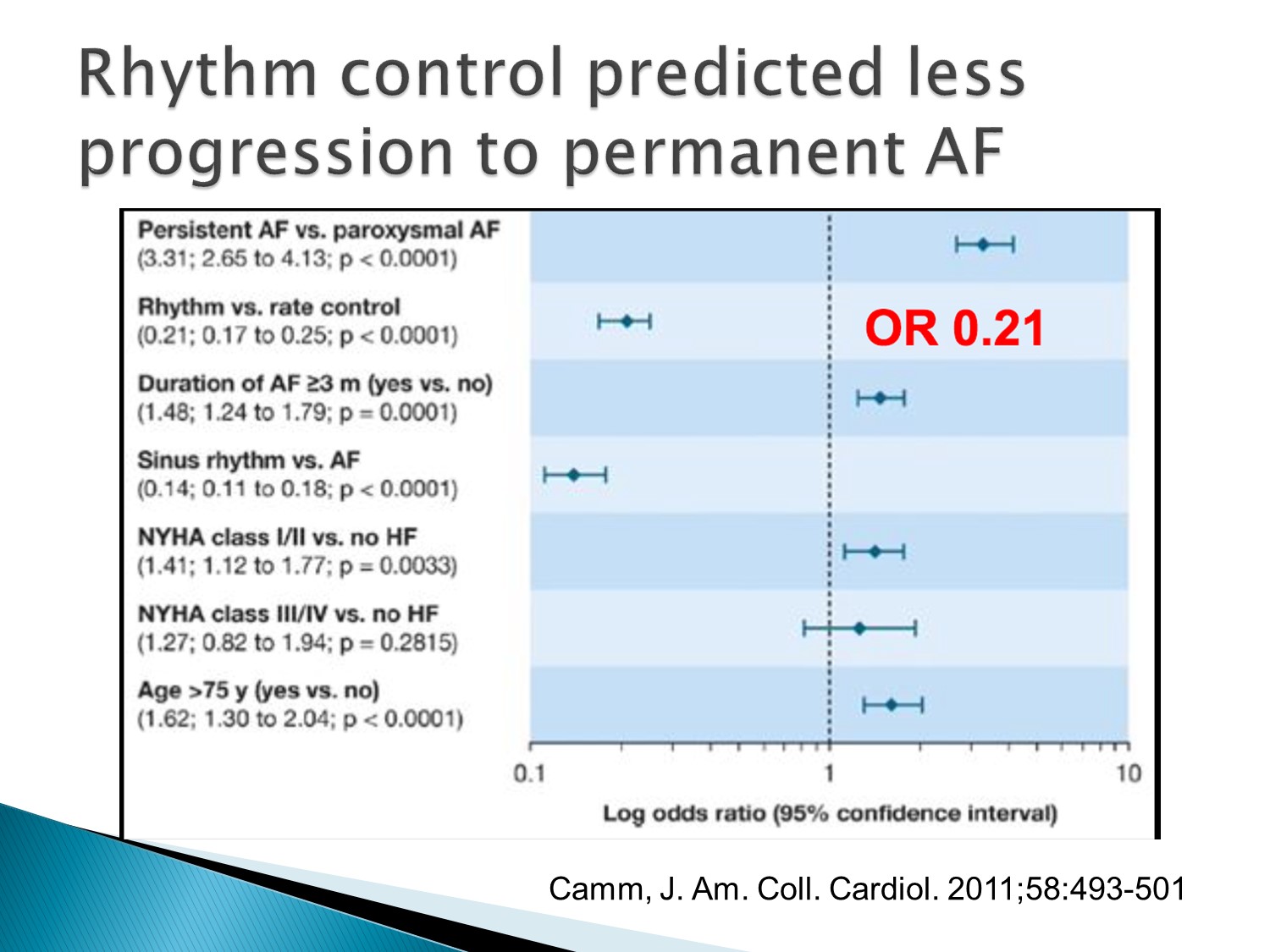
Rhythm control也比較不會進展到permanent A fib
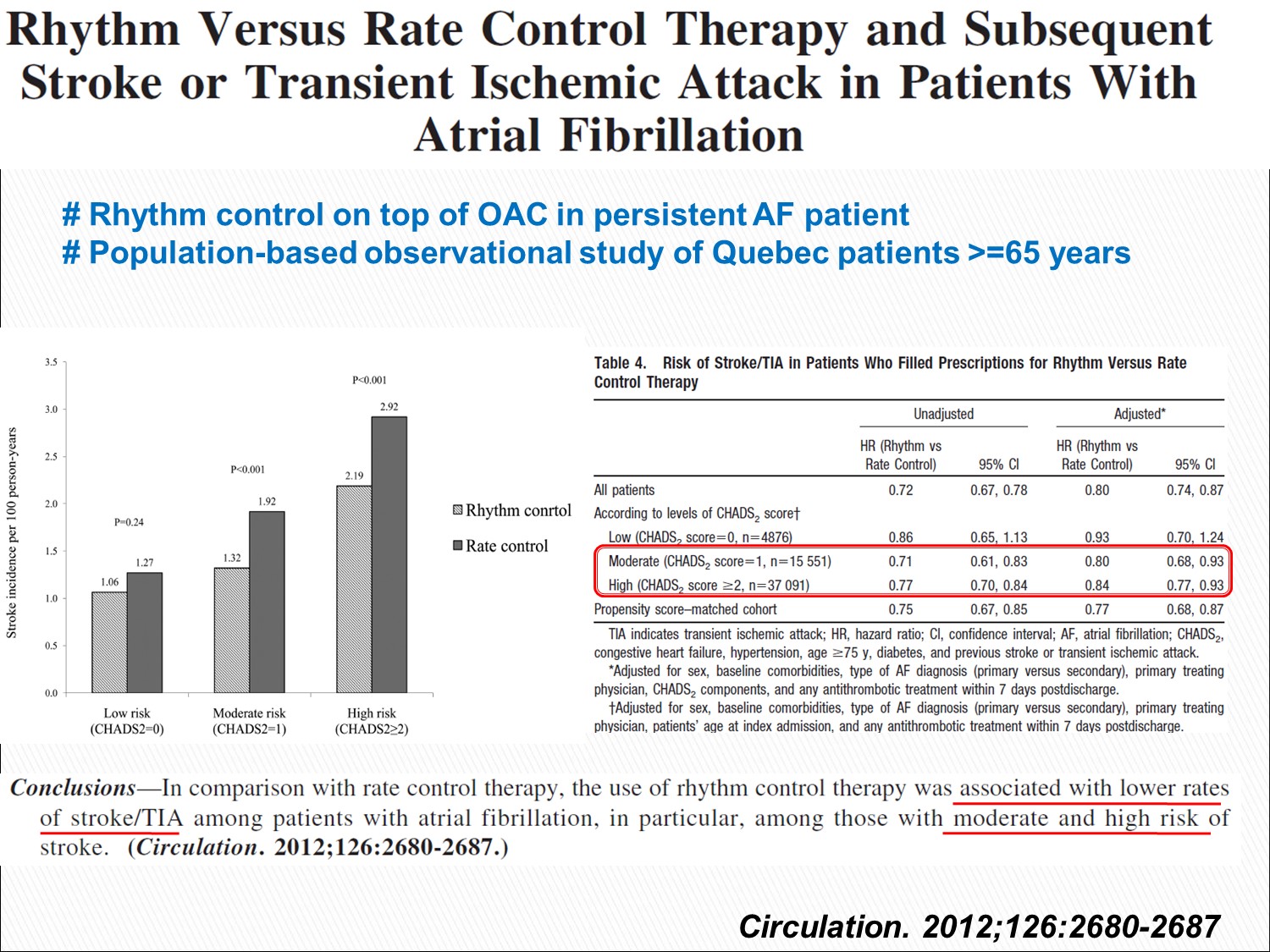
這篇與 AFFIRM 的結果不同,這篇顯示 rhythm control 的中風機會較少
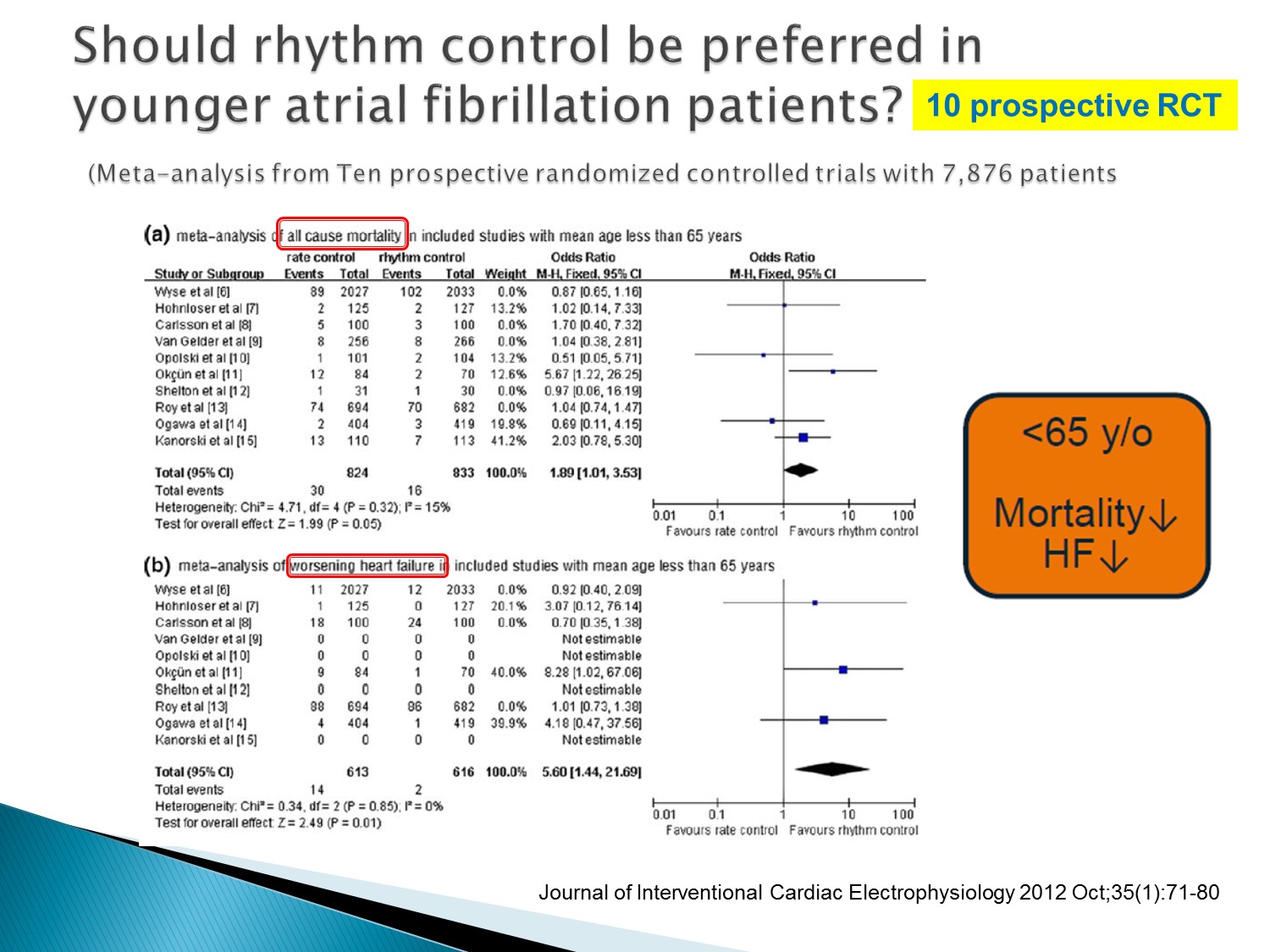
年輕病人使用 rhythm control,mortality 以及 HF 的機會下降
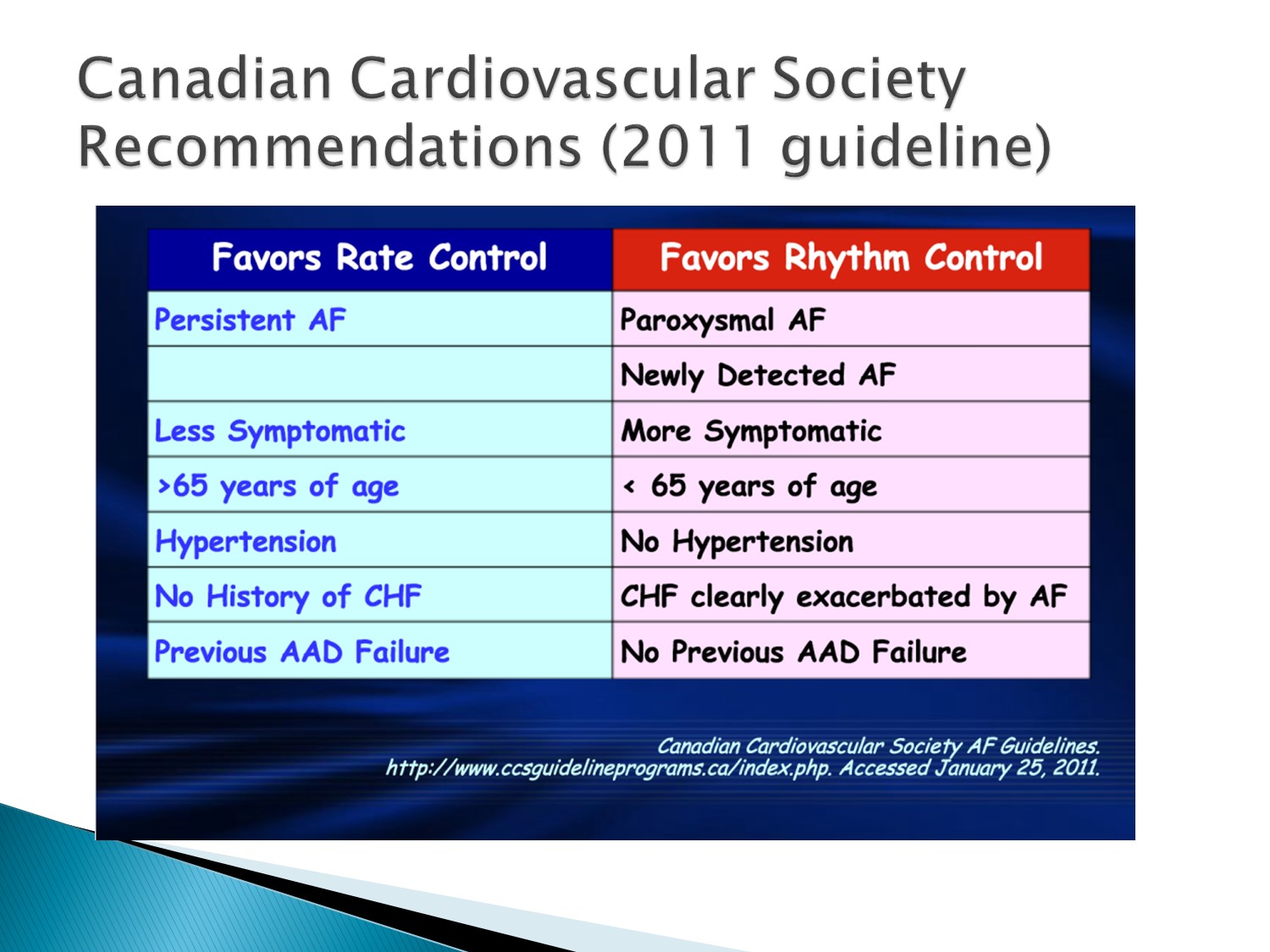
哪些人favor rhythm control:較 fresh、較年輕、Underlying disease 較少、symptoms 較嚴重、HF 會被 A fib 誘發、functional capacity 較好者
以下為林廷遠醫師ppt檔案原本就有的內容:
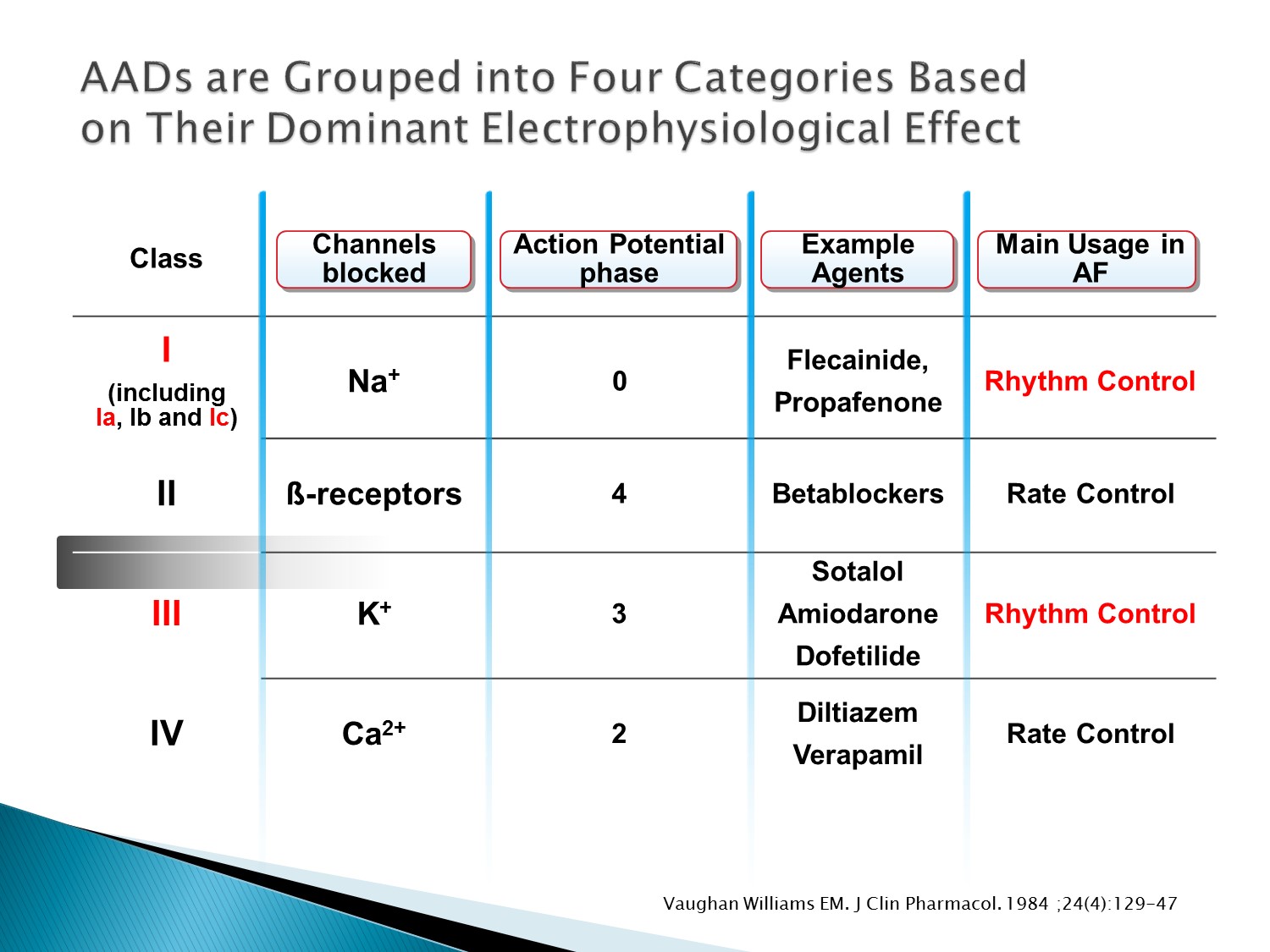
- Anti-arrhythmic drugs act through electrophysiological mechanisms by blocking the ionic channels across cell membranes that create the action potentials.
- AADs can be used for rhythm restoration, including cardioversion, and for maintenance of sinus rhythm.
- AADs are commonly grouped into four broad categories by the Vaughan Williams classification, based on their dominant electrophysiological effect.
- For example, class I drugs block Na+ channels, thus acting on phase 0 of the action potential. They include Flecainide and Propafenone, and due to their mode of action are primarily used as rhythm control drugs.
Reference:
Vaughan Williams EM. J Clin Pharmacol. 1984 Apr;24(4):129-47
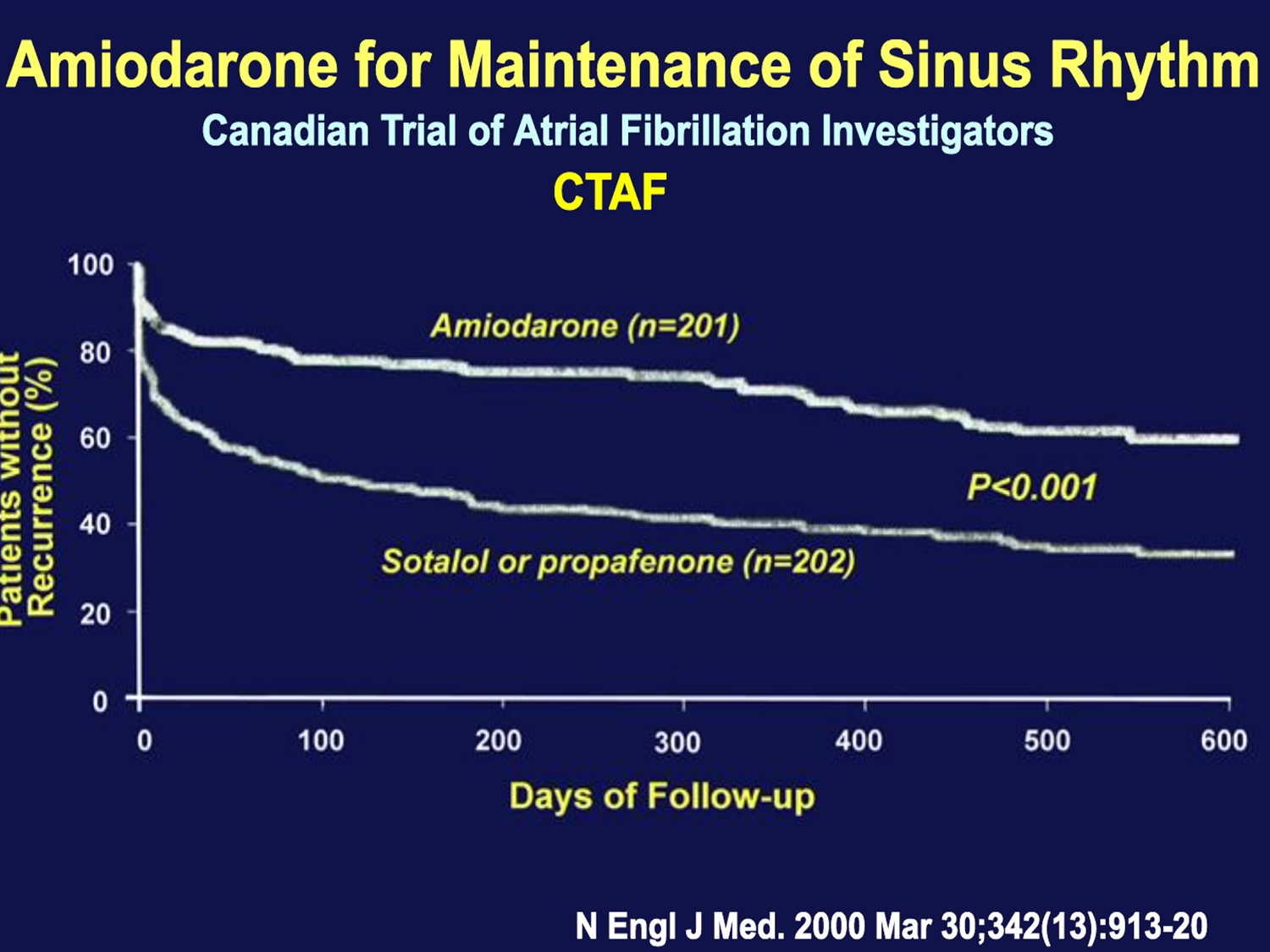
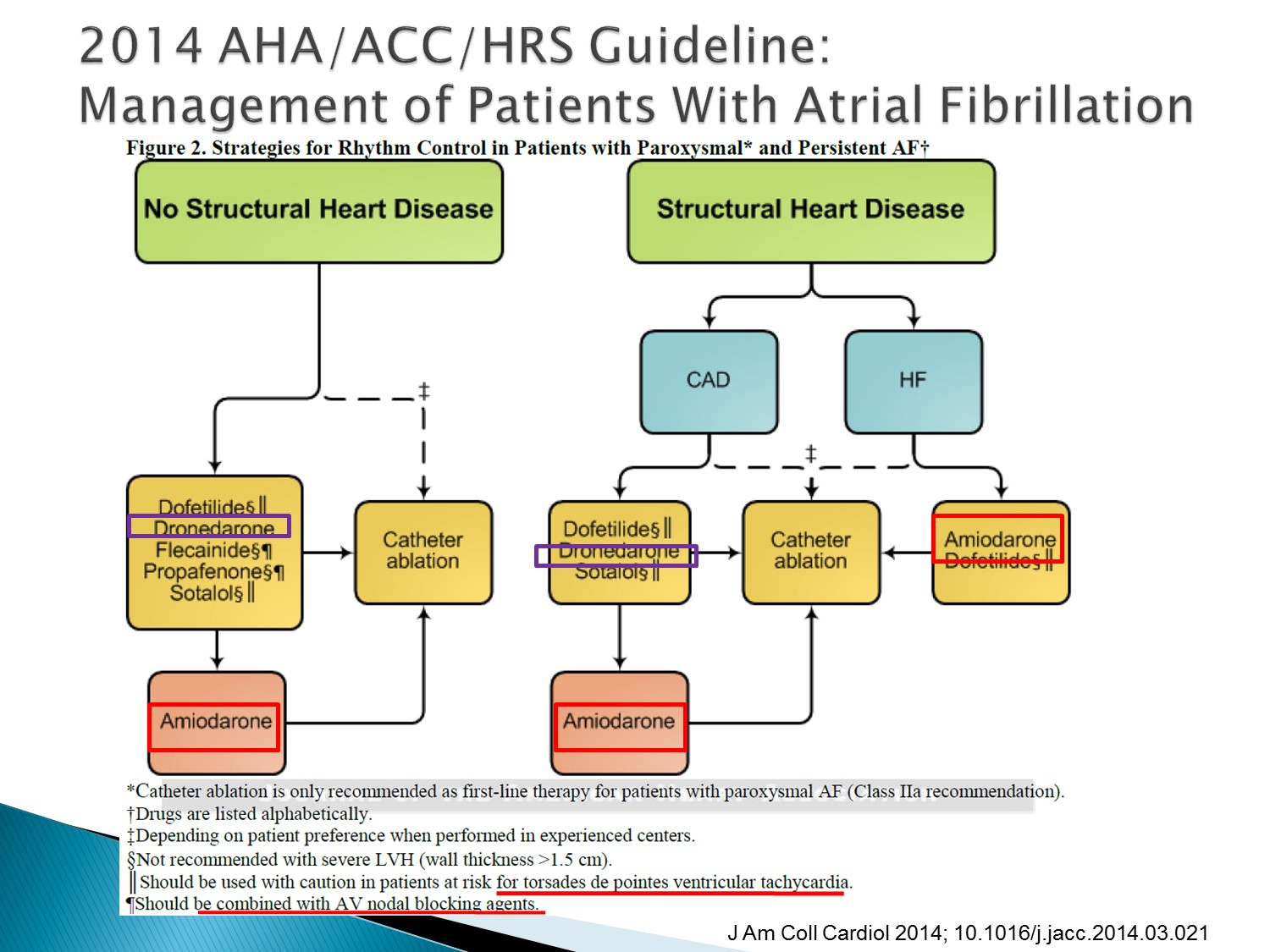
在maintain sinus rhythm方面Amiodarone是最有效的藥物
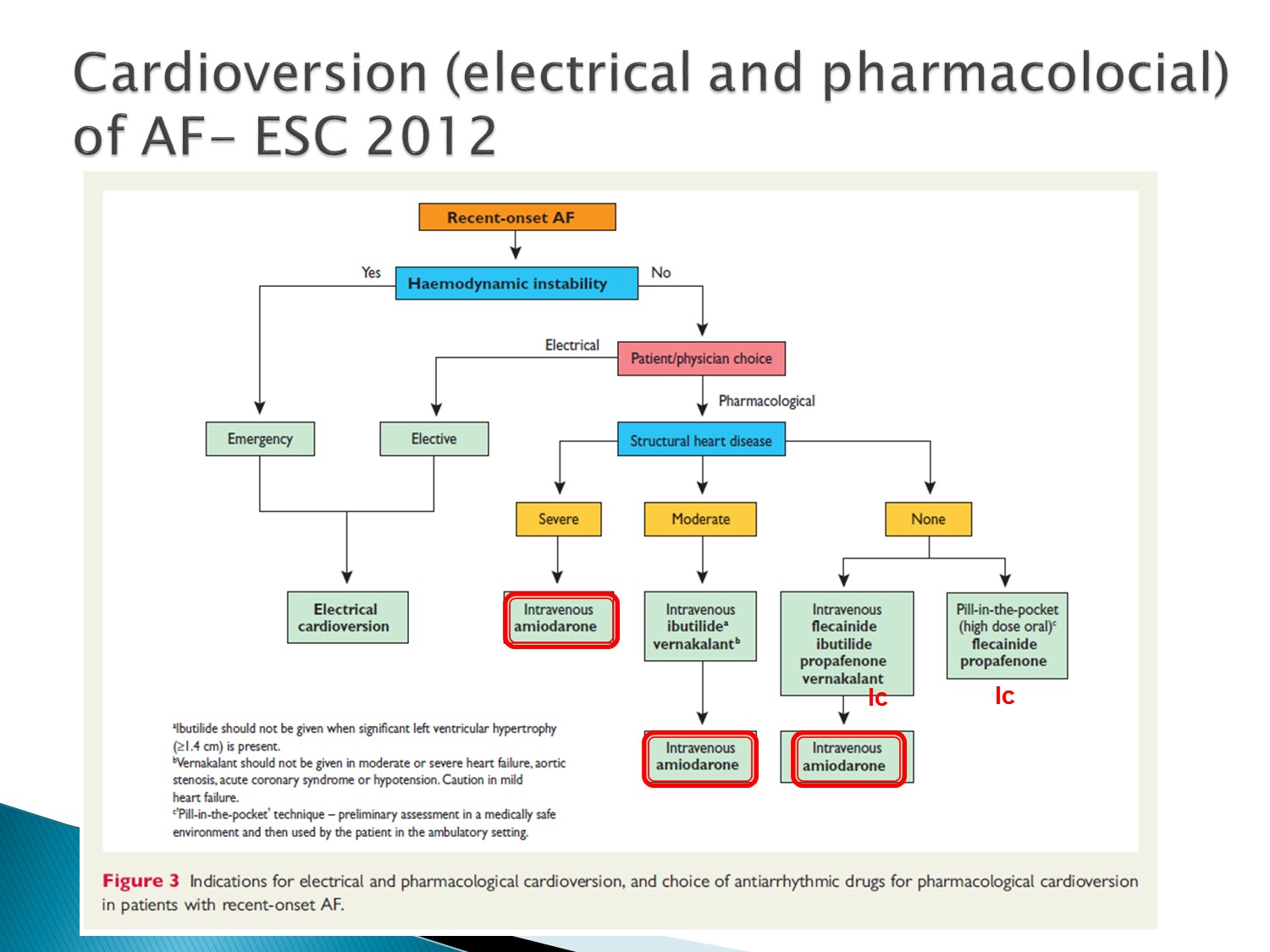
在 conversion 部分,根據有無 structural heart disease 來選擇藥物
在國外若 structural heart disease不嚴重,則有其他藥物可以使用,而 amiodarone 因為 side effect 放在後線
但台灣只有 amiodarone 可以使用
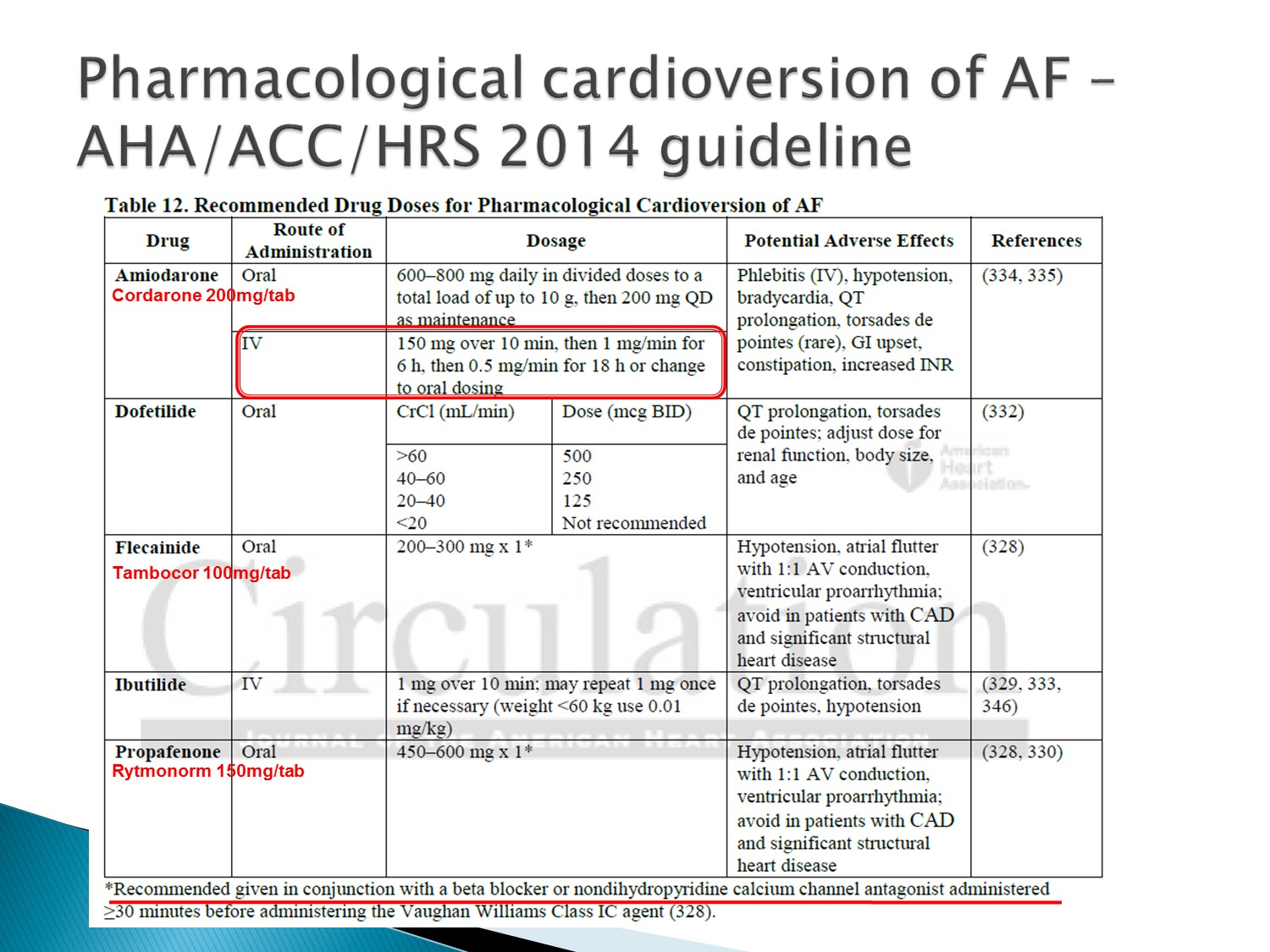
ACC guideline
Amiodarone 的泡法:6 支泡 500ml 前 6 小時 run 33 cc/hr,後 18 小時run 17cc/hr
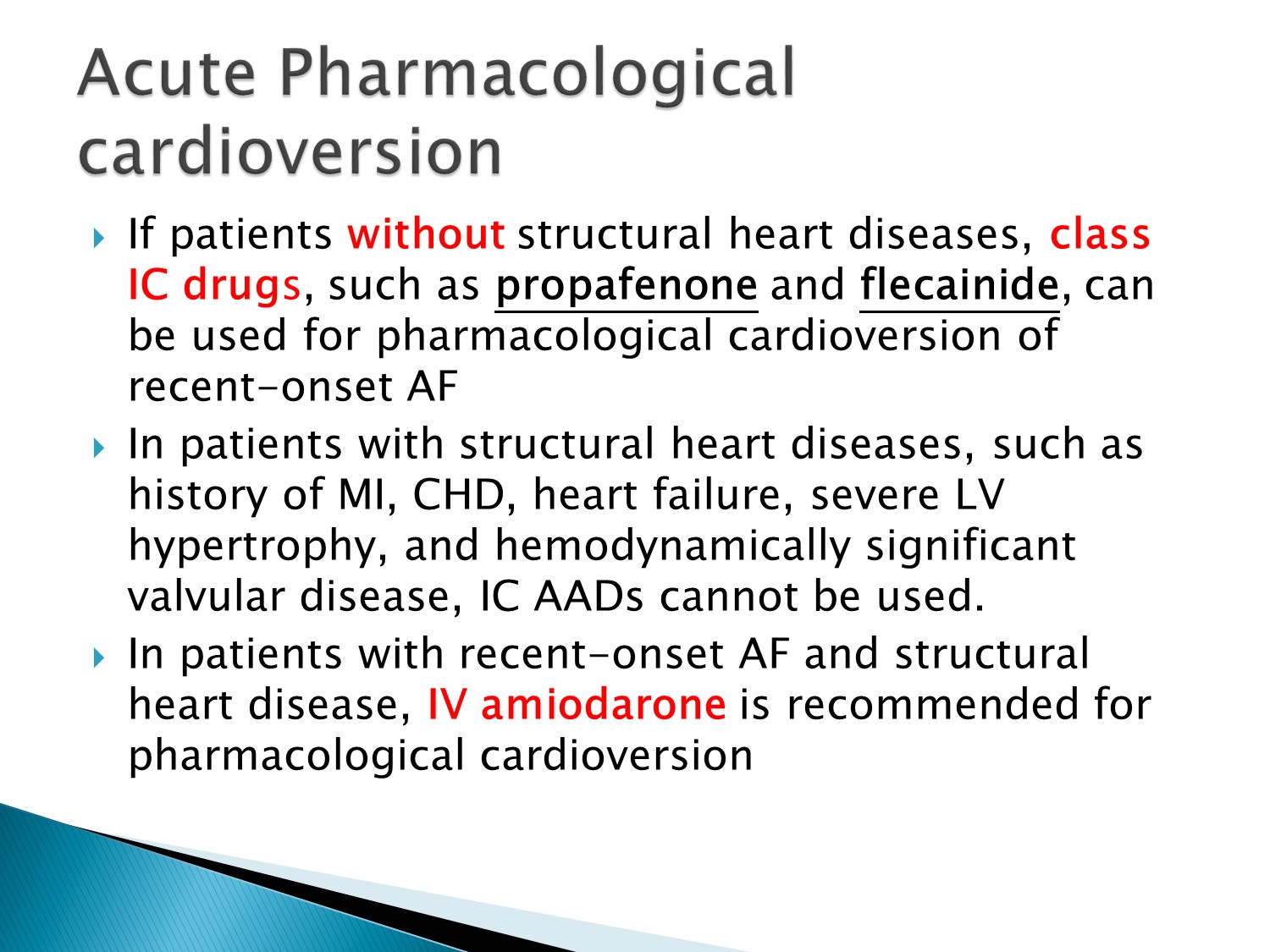
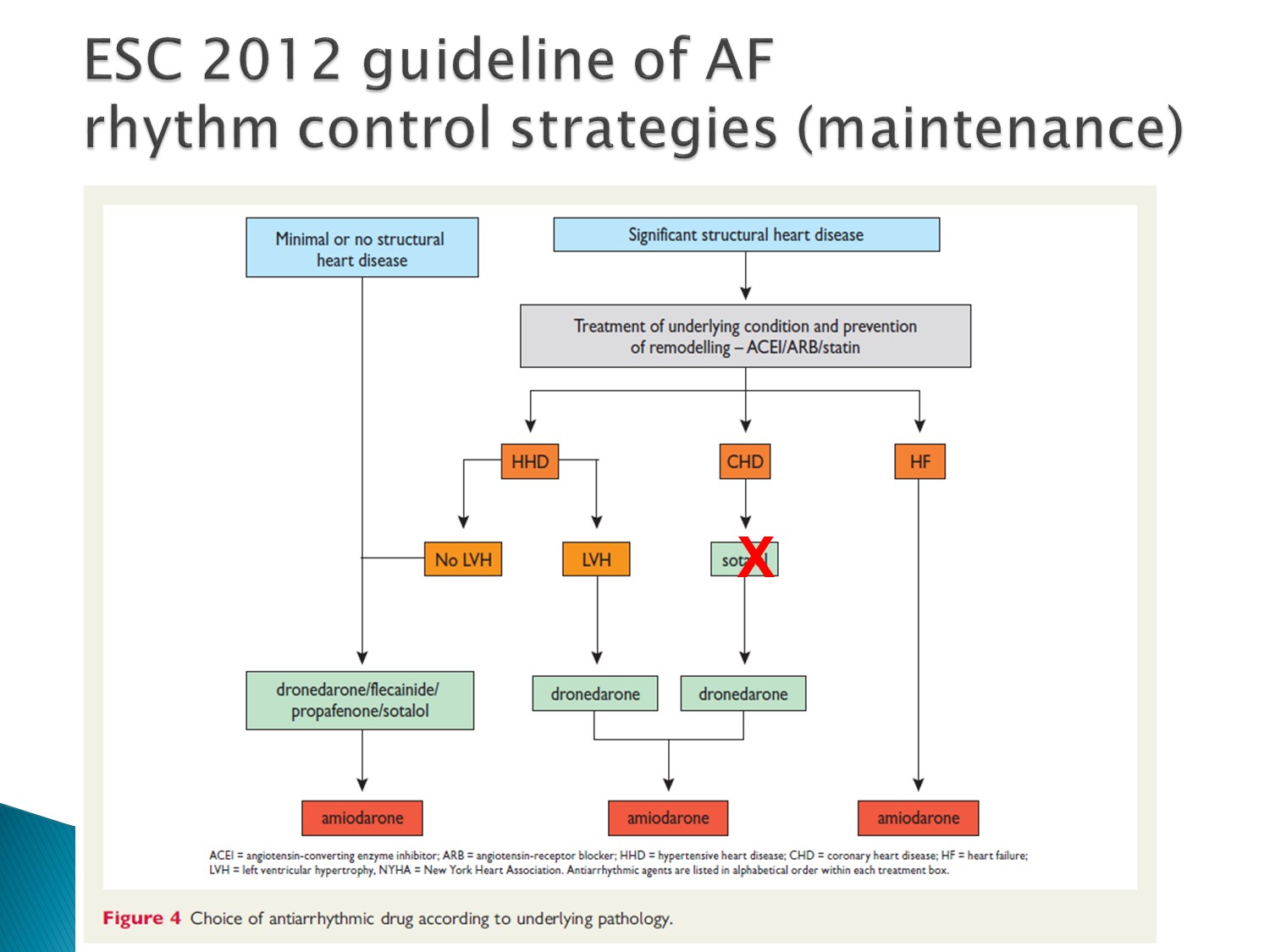
看有無 structural heart disease 決定用藥
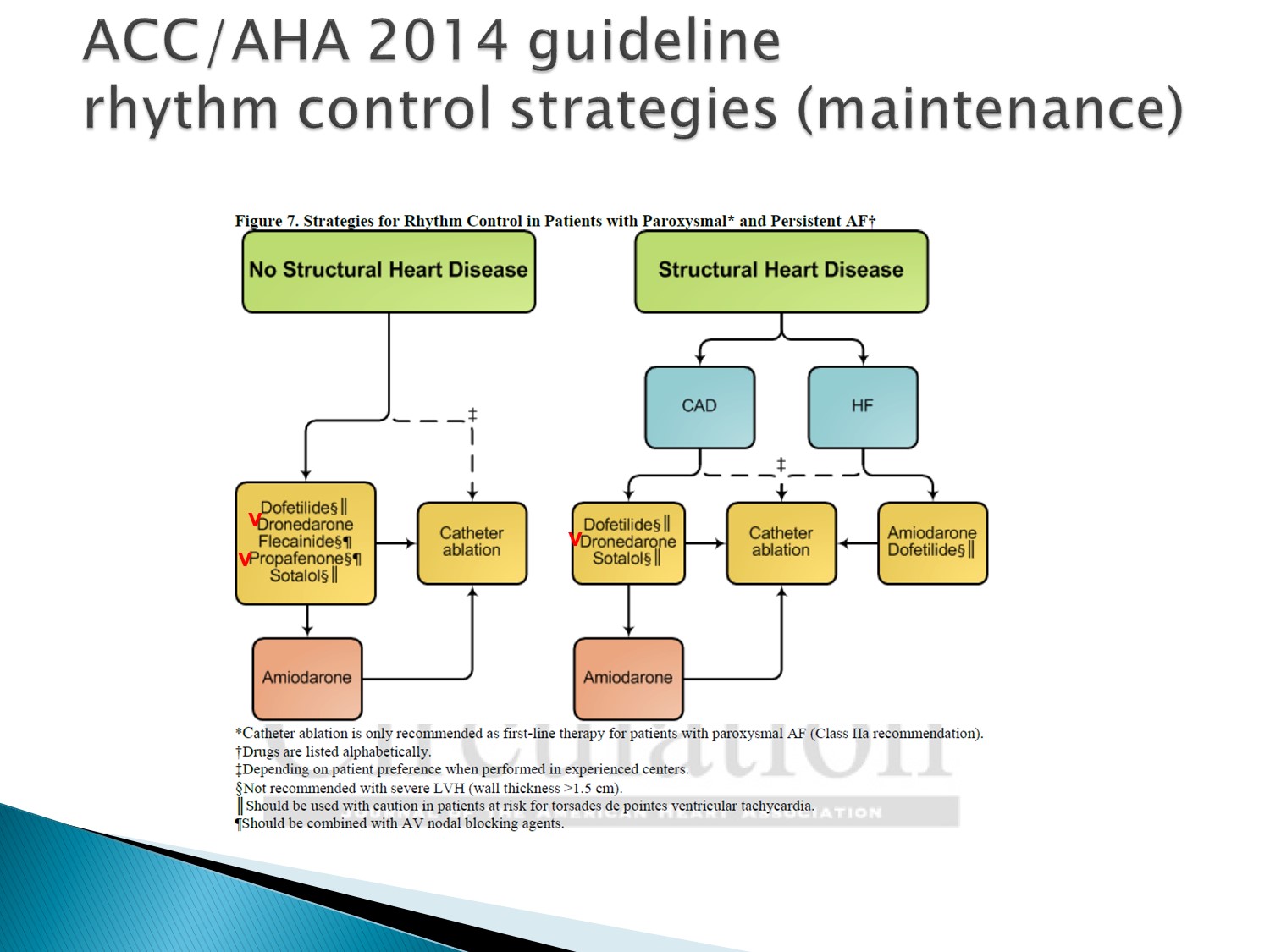
在台灣,有 HF 者,只有 amiodarone 可以用
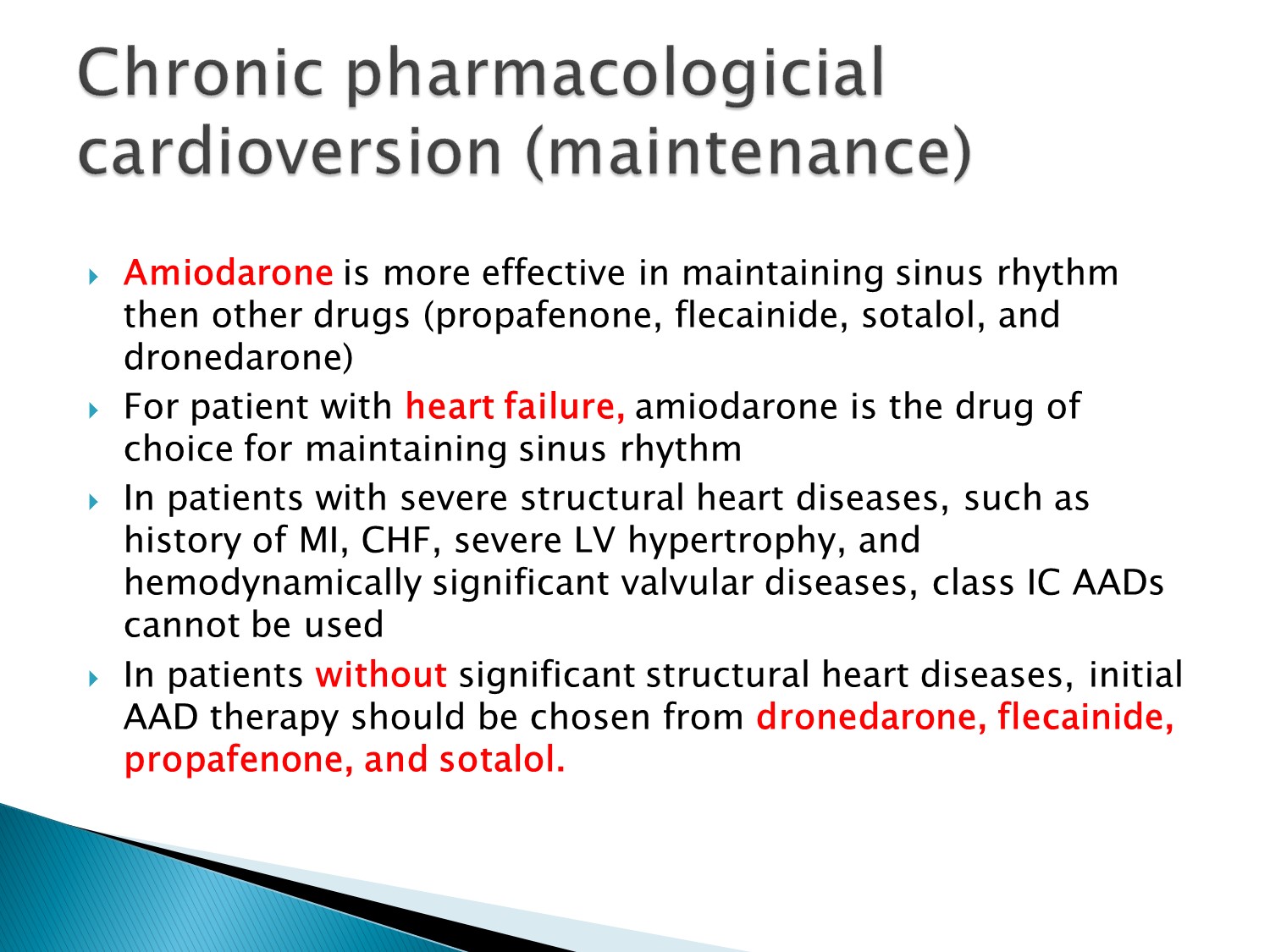
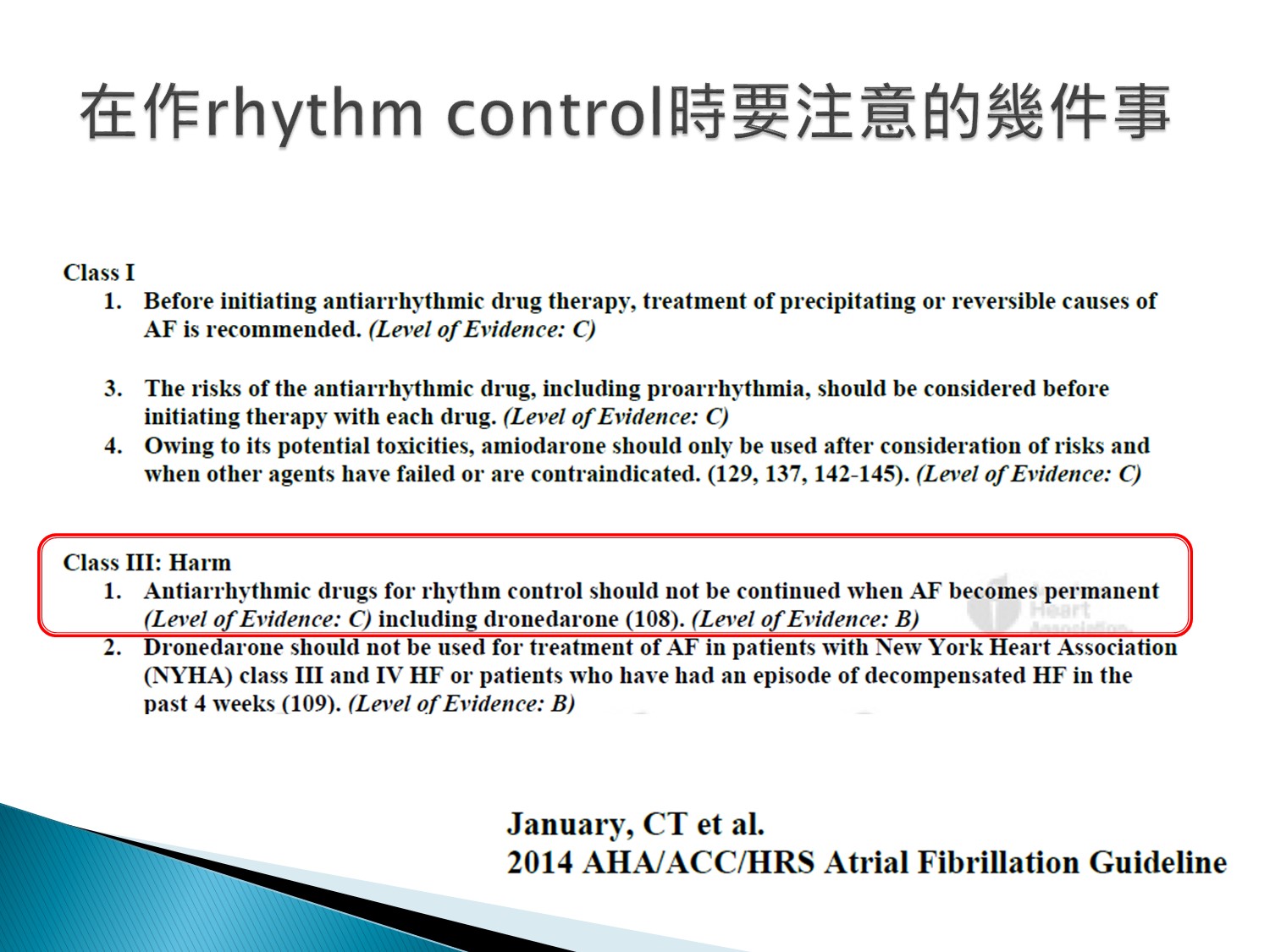
若已是 permanent A fib,就不要再做 rhythm control 了
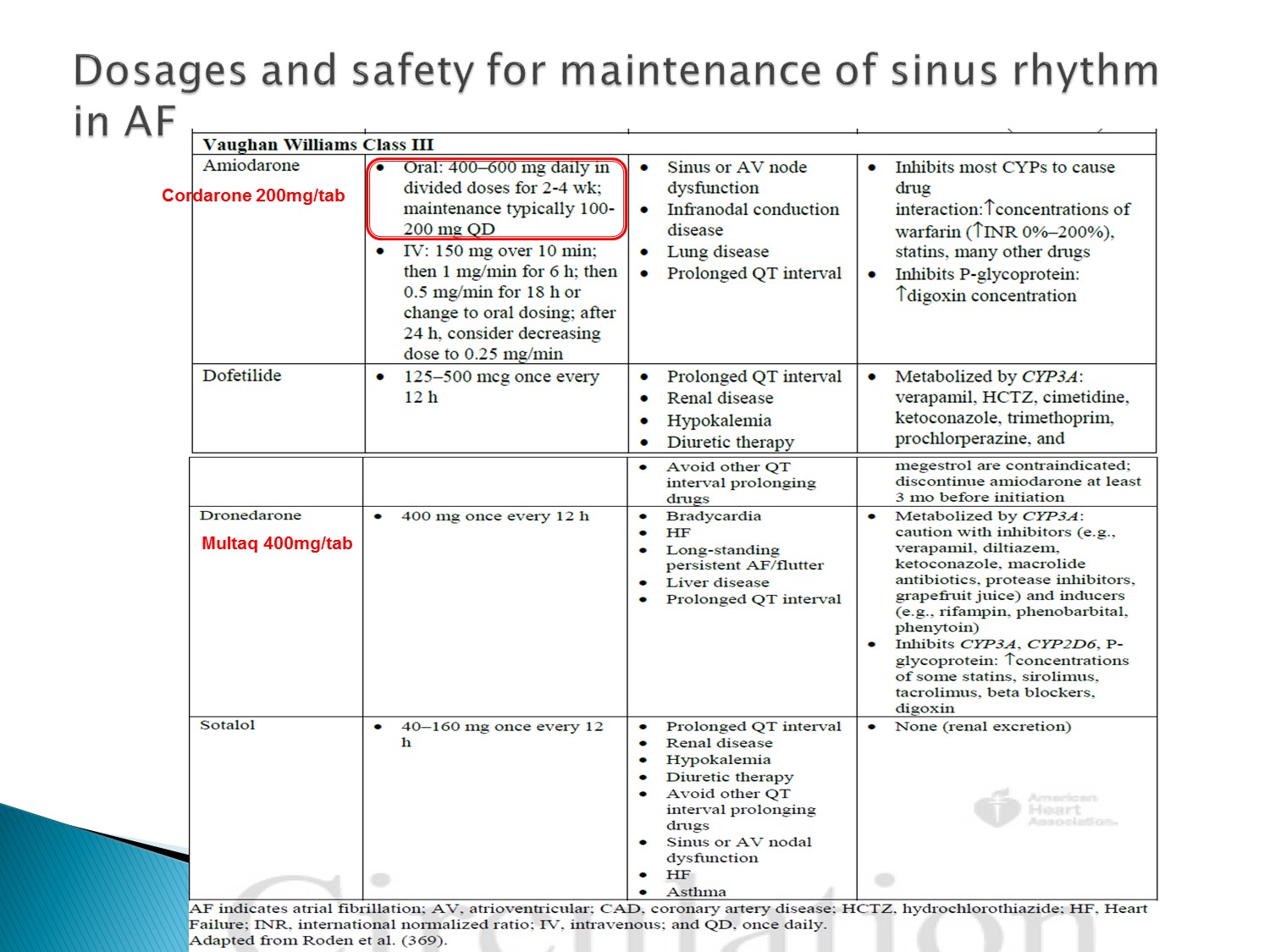
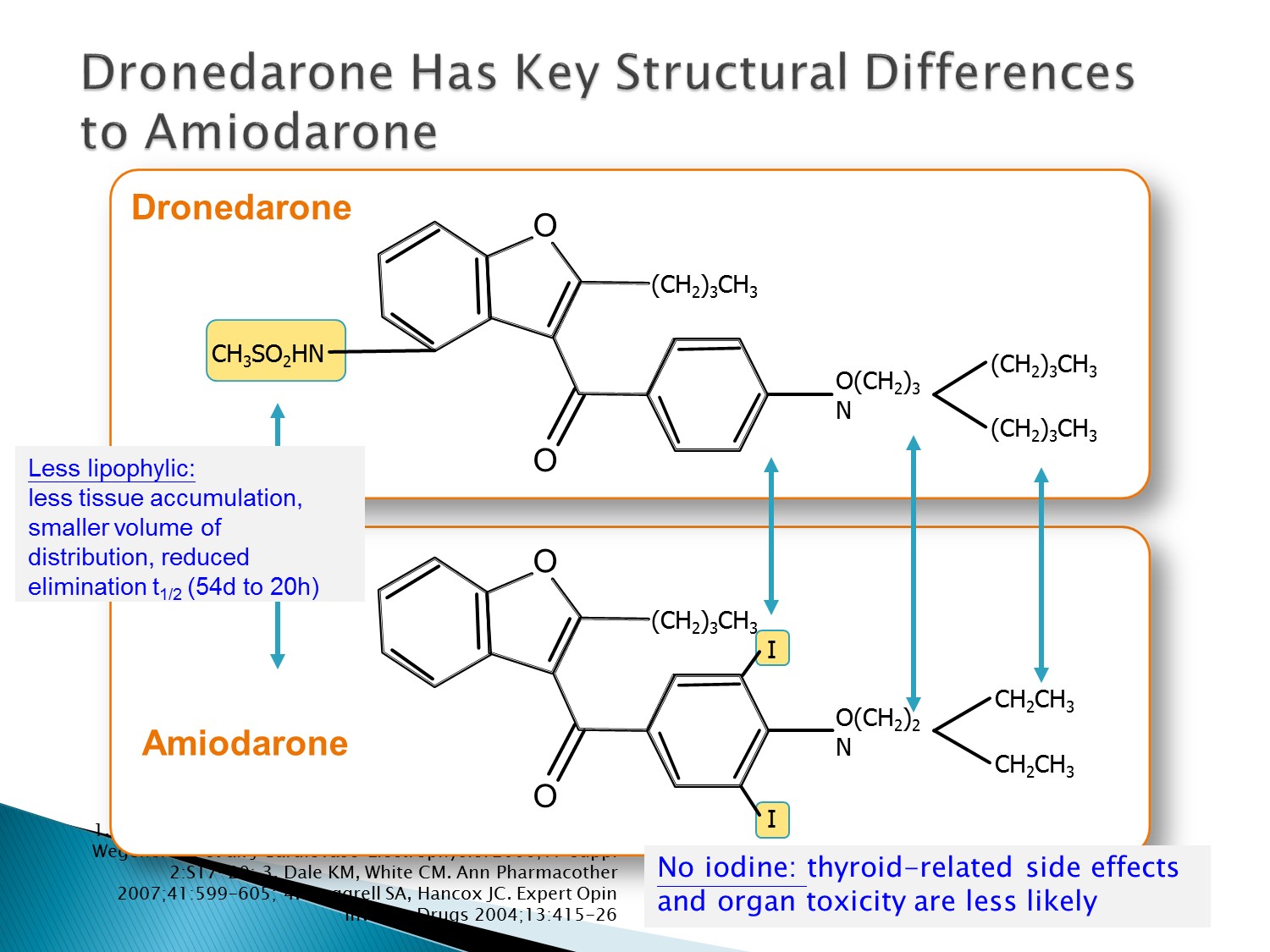
Dronedarone 沒有碘,不會有甲狀腺副作用
半衰期 20 小時,比 amiodarone 短很多,造成 bradycardia 時也不用觀察這麼久
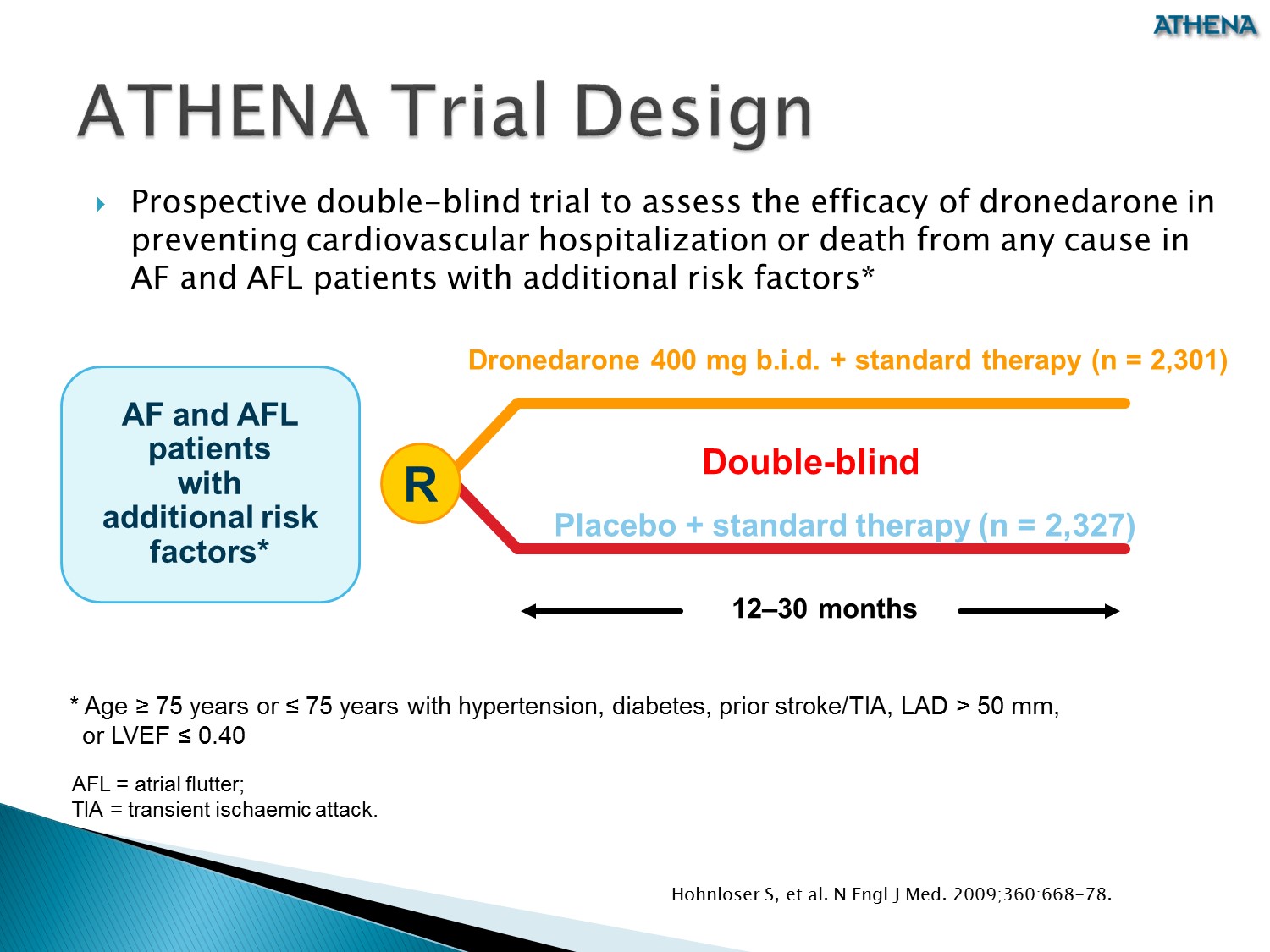
之前的心律不整藥物對於死亡率的結果都是 neutral
ATHENA trial 發現,dronedarone 對於預防 A fib 方面,可以降低死亡率以及 CV 原因的住院率
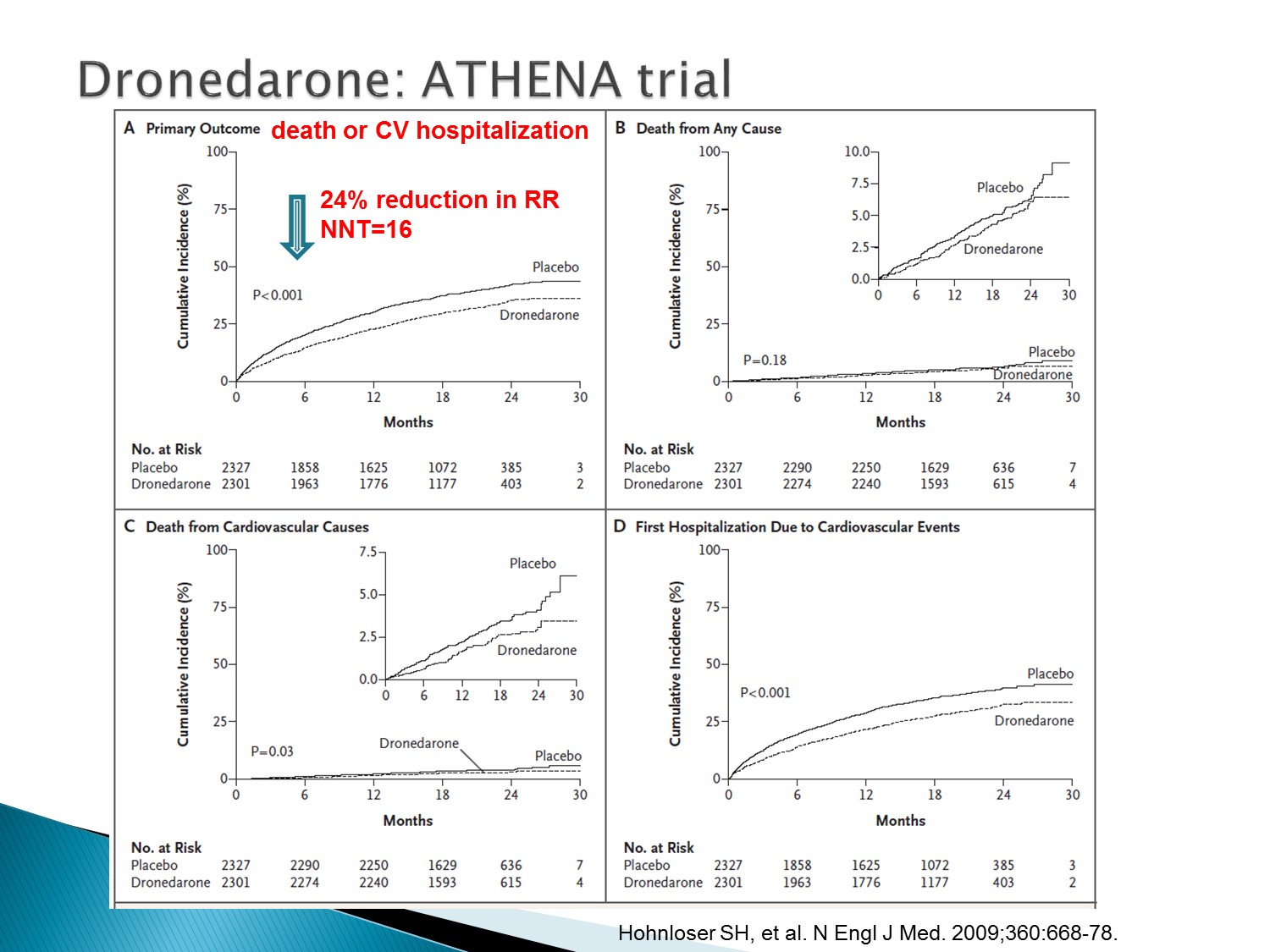
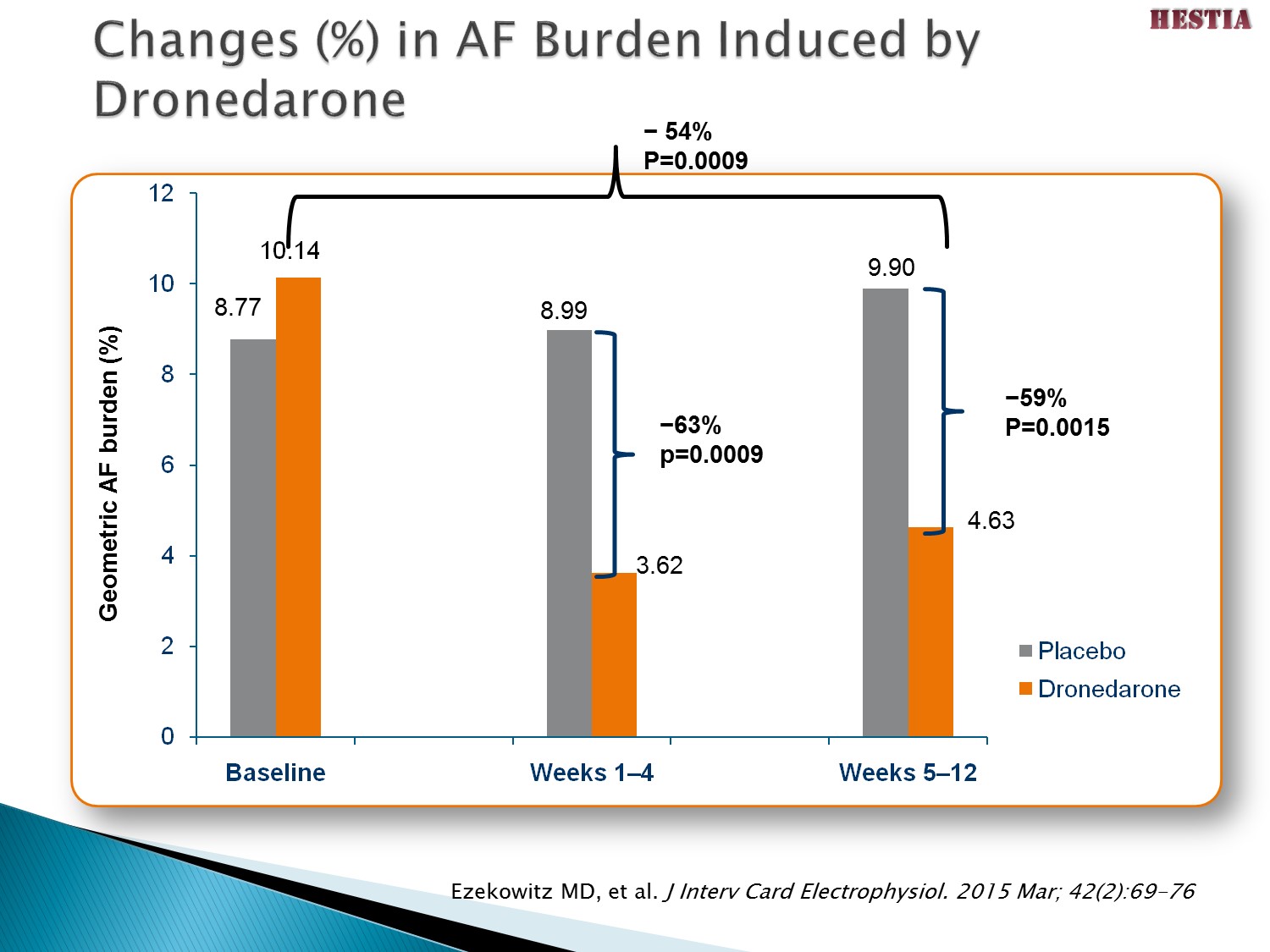
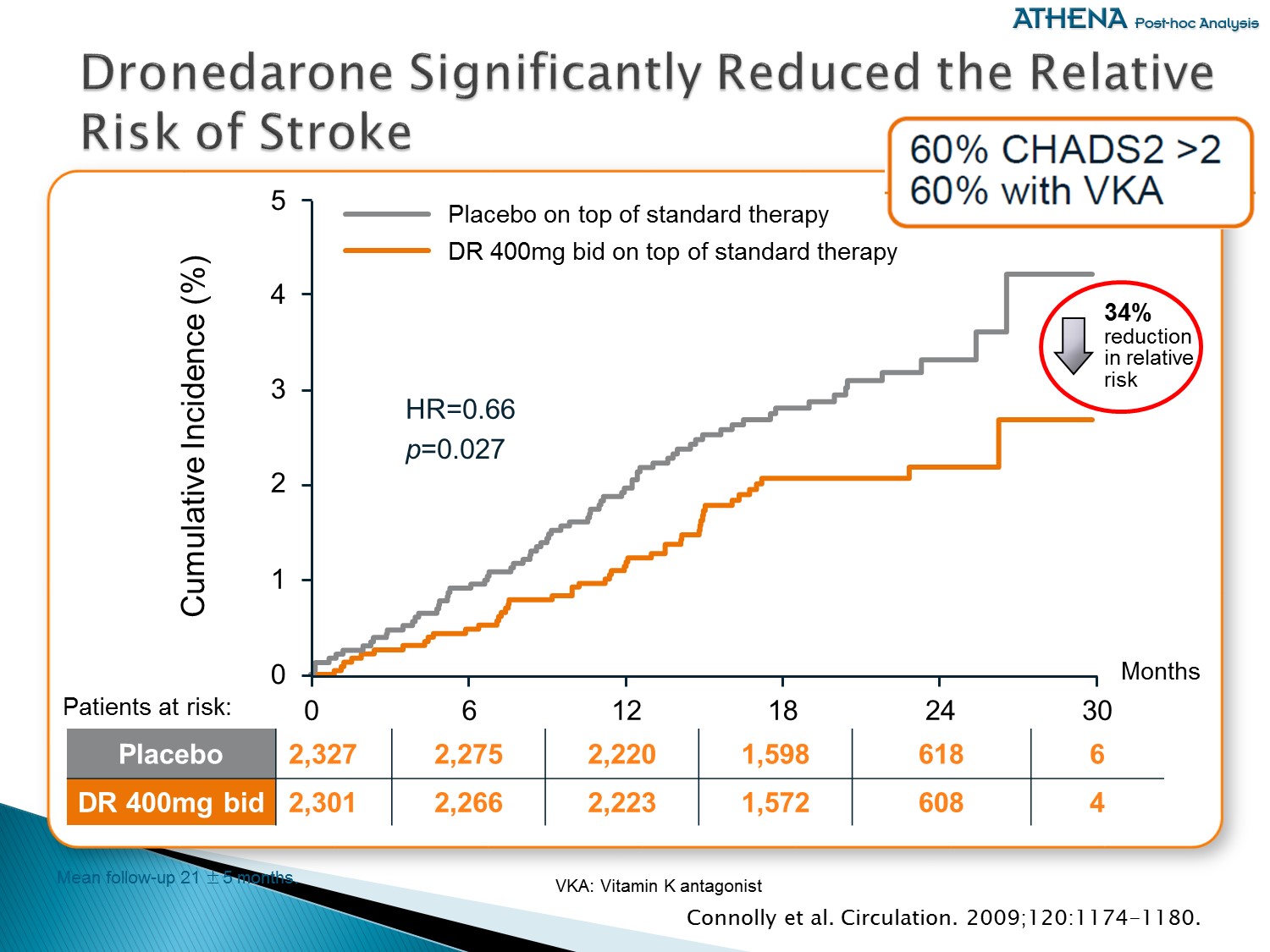
重點:
ATHENA 以事後檢定分析,發現可以有效減少中風風險達 34 % (一年約 1.2 % 發生比例),有專家學者認為是 Multaq 維持 SR、減少 AF burden,且併用 OAC 的緣故
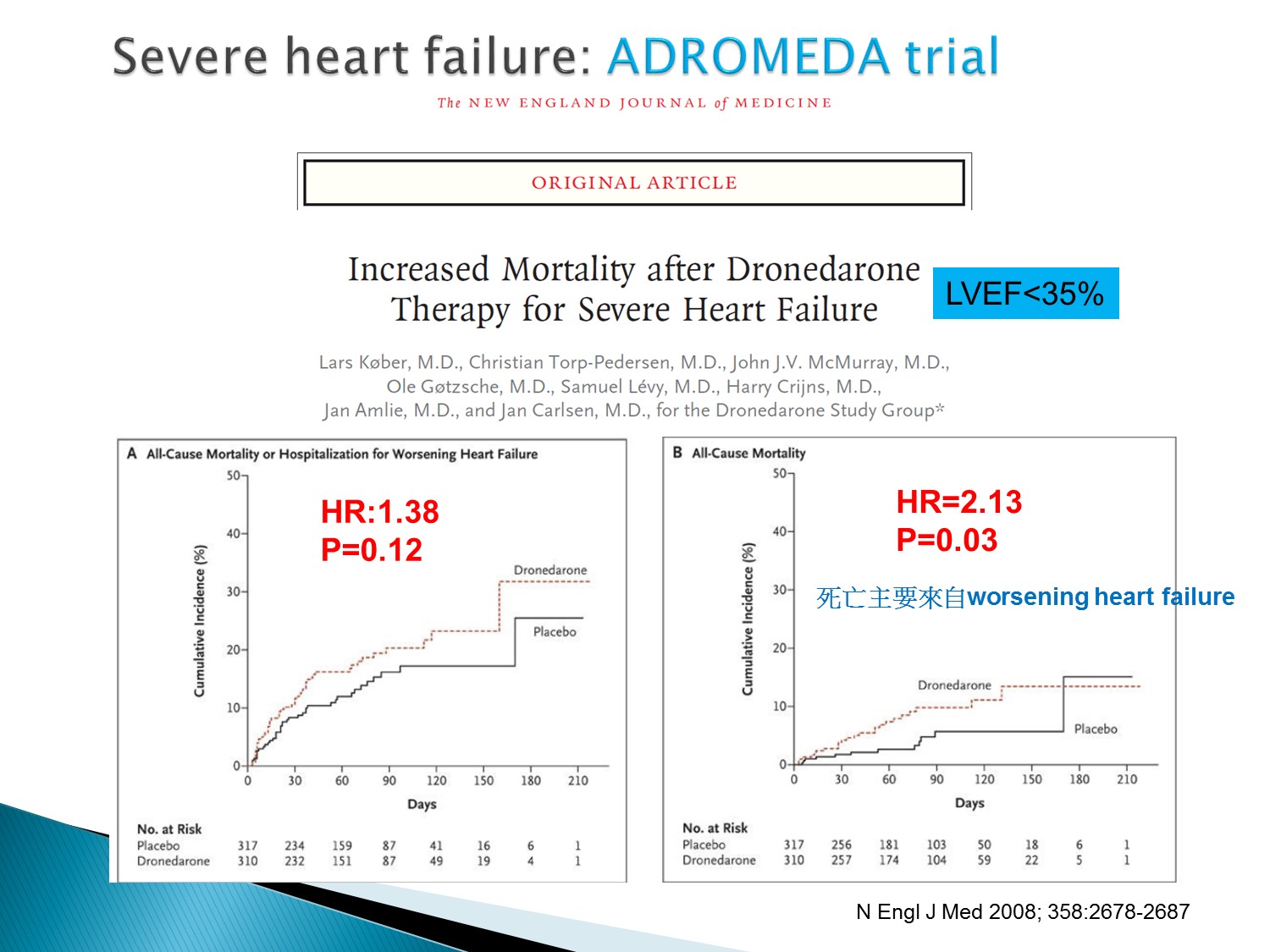
Dronedarone 的缺點:LVEF < 35% 不可使用
會使 HF 惡化,造成死亡率上升
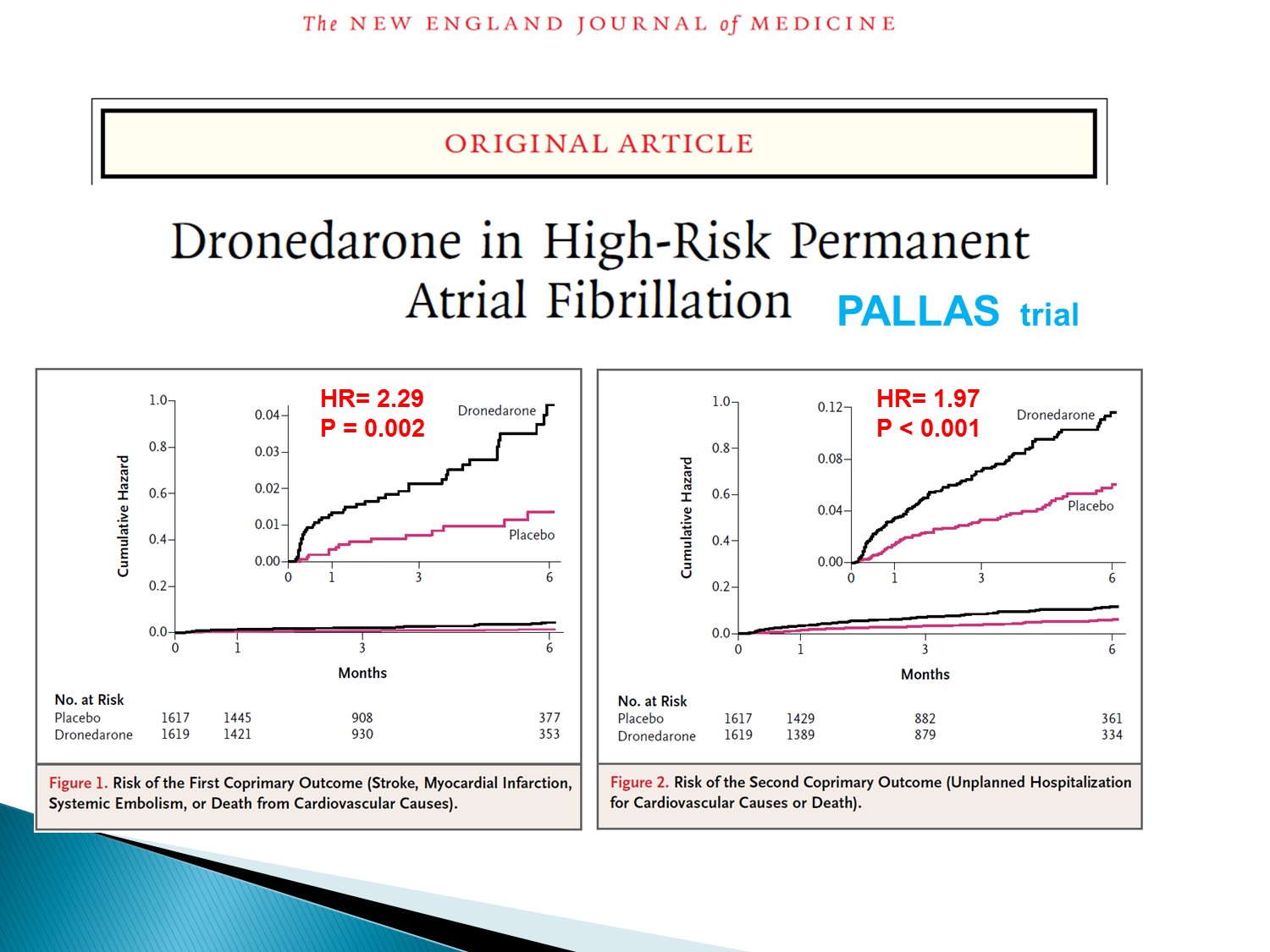
Dronedarone 的缺點:permanent A fib 不可使用
會使 MI, stroke, embolism, 死亡率上升
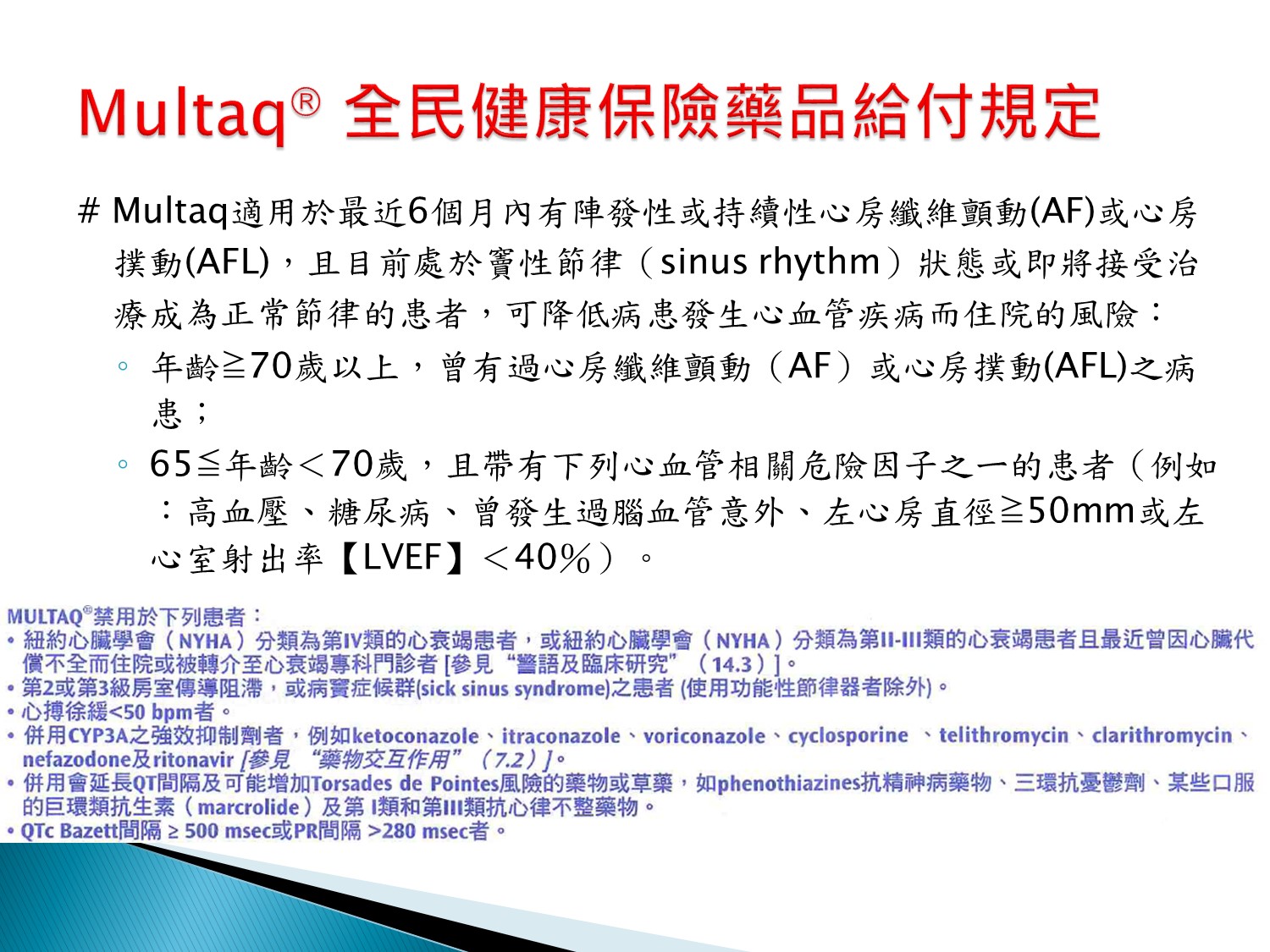
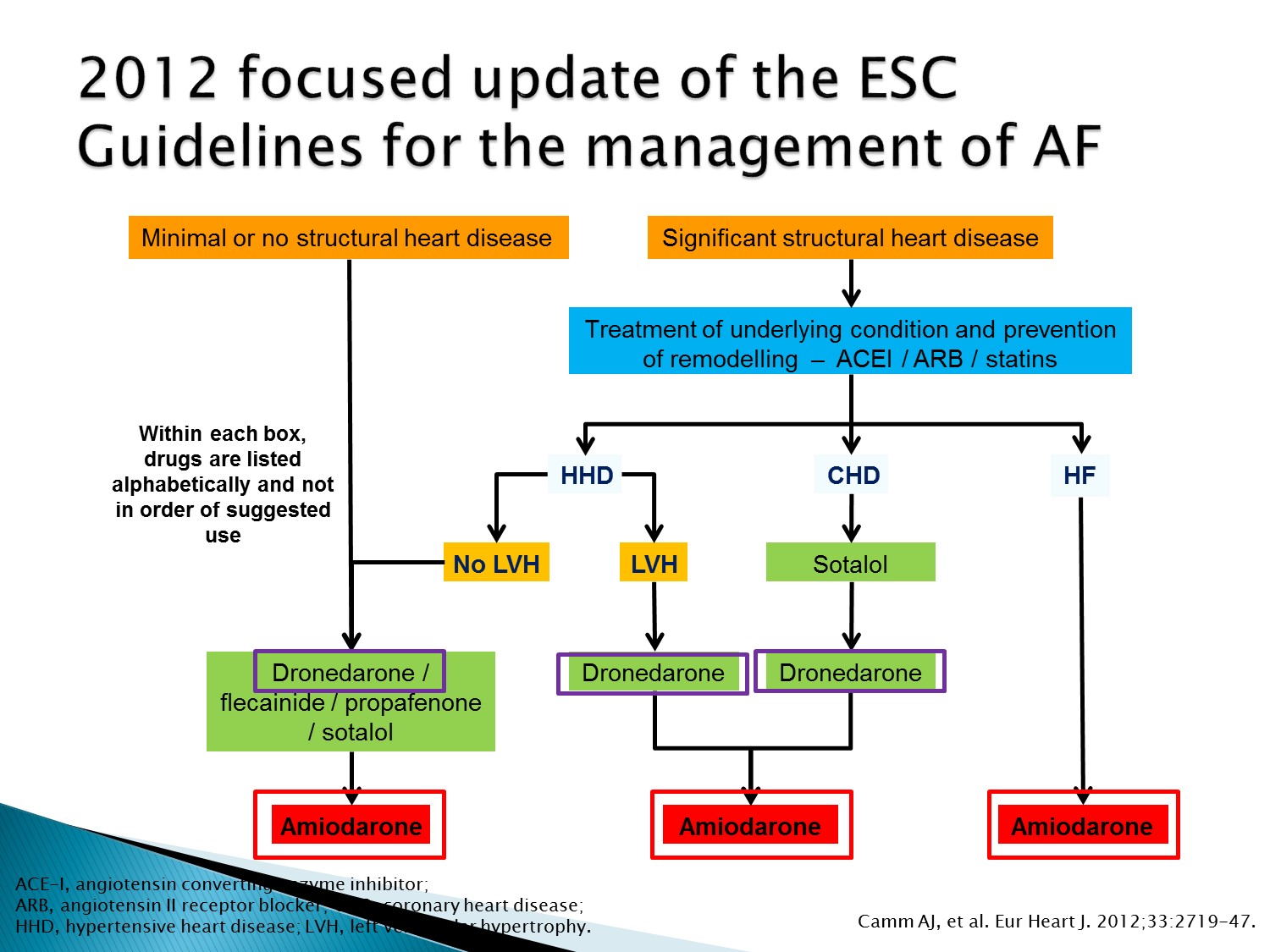
Dronedarone 用在沒 structural heart disease、CAD 者、LVH 者
只有 HF 者不可使用
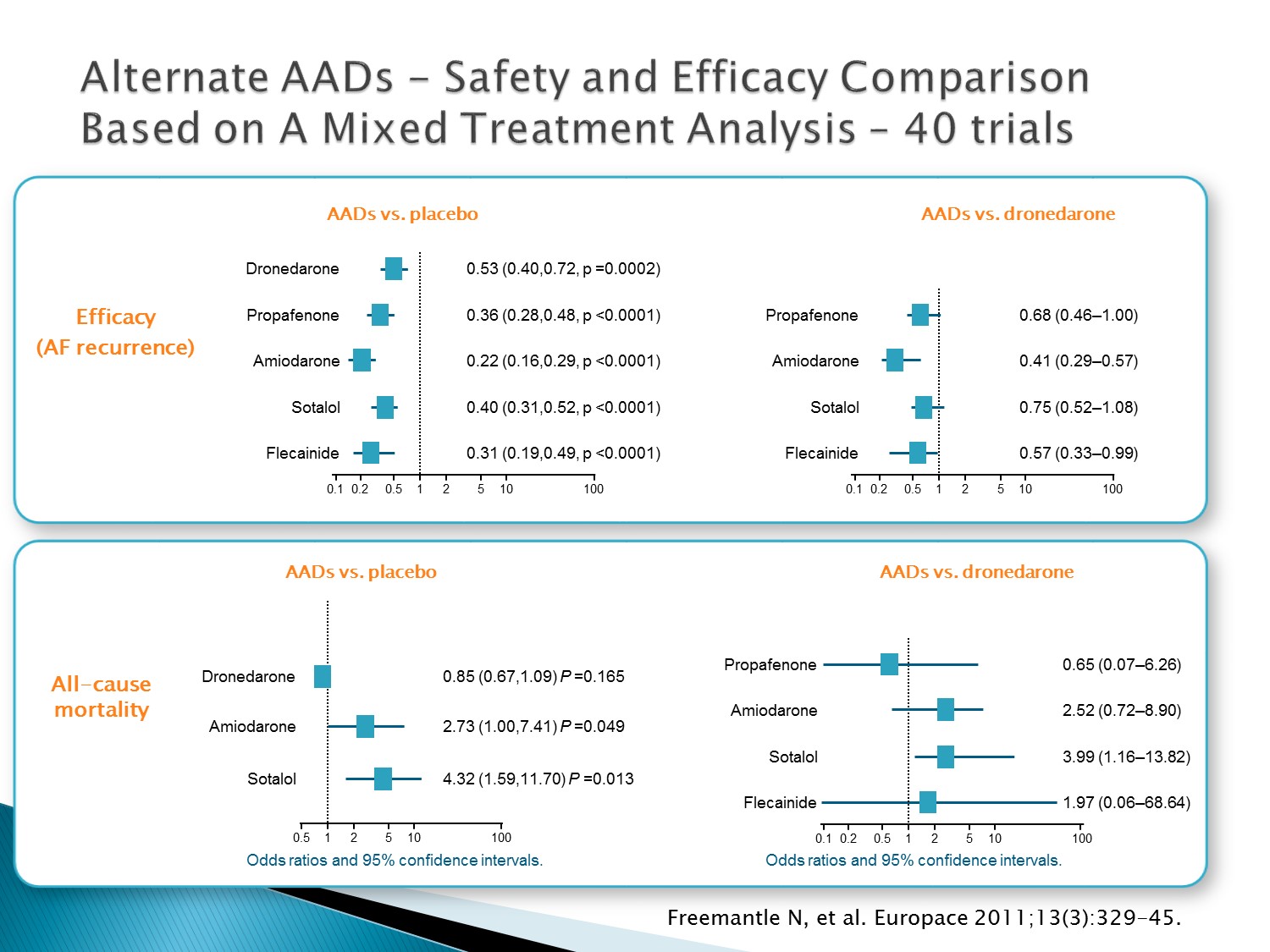
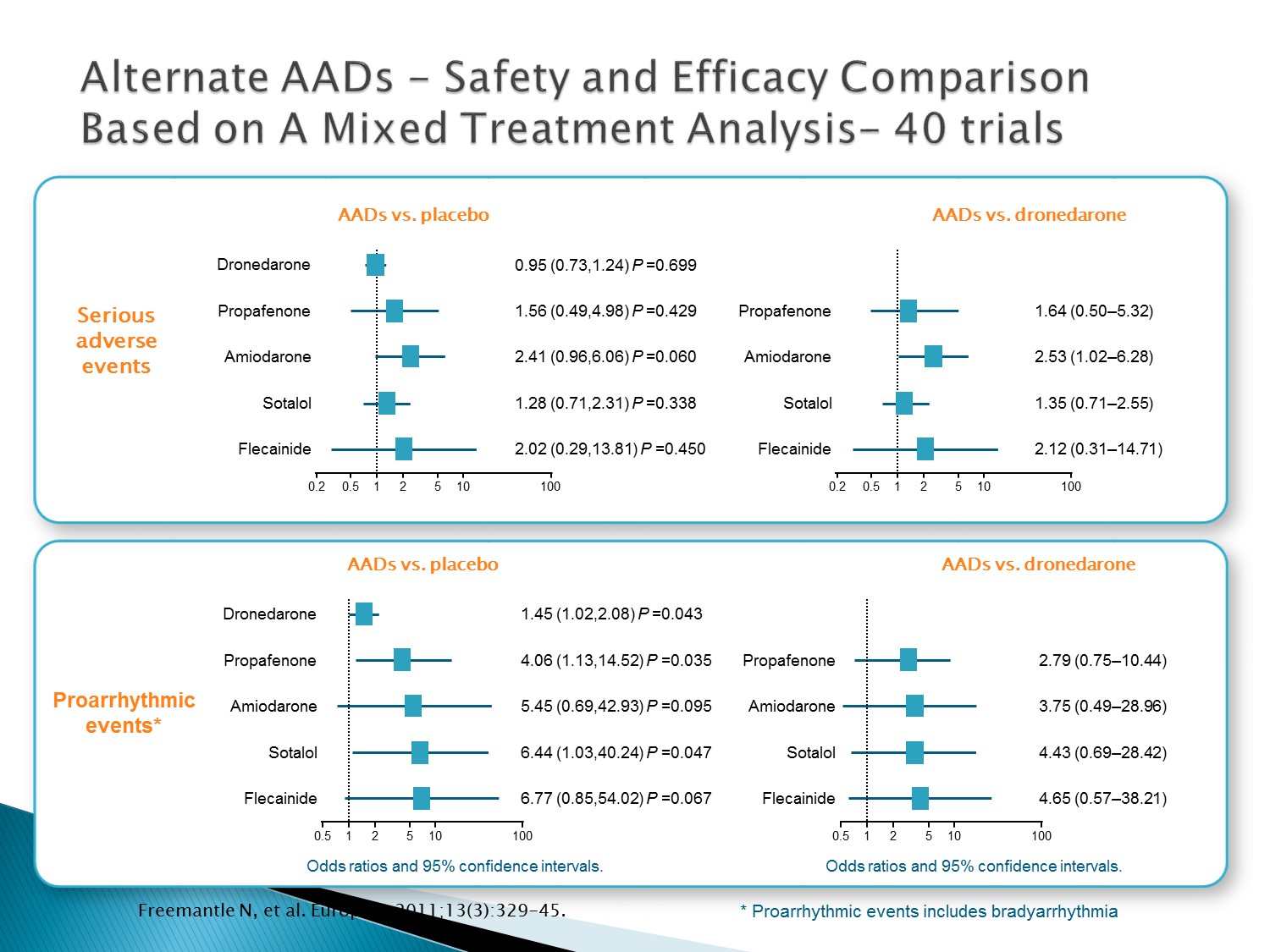
以下為林廷遠醫師ppt檔案原本就有的內容:
Mixed treatment comparison (MTC) is increasingly used to estimate the treatment effects when directly randomised comparisons are not available
Freemantle performed a MTC to compare the risk of morbidity and mortality associated with dronedarone, amiodarone, sotalol, flecainide and propafenone, including the rate of Serious Adverse Events (SAE) associated with each treatment
Freemantle concluded that dronedarone may be associated with less serious adverse events than other AADs, although there is substantial uncertainty on the relative occurrence of SAEs for several AADs
Trials examining effect of AADs in subjects with AF identified using exhaustive searches of Medline and EMBASE
Inclusion criteria:
AF/Atrial Flutter (AFL) population
Randomised Controlled Trials
Exclusion criteria:
Studies enrolling subjects with AF/flutter ≤ 3 months after cardiac surgery.
Minimum duration of follow up for clinical studies: 3 months.
Minimum duration of treatment: 30 days.
Editorials
Case-studies
Outcomes analysed:
All cause mortality
Stroke
Serious Adverse Events
For all serious adverse events:
20 trials / 9734 patients / 1716 experienced at least one SAE
Reference:
Freemantle et al. Europace. 2011;13(3):329-45.
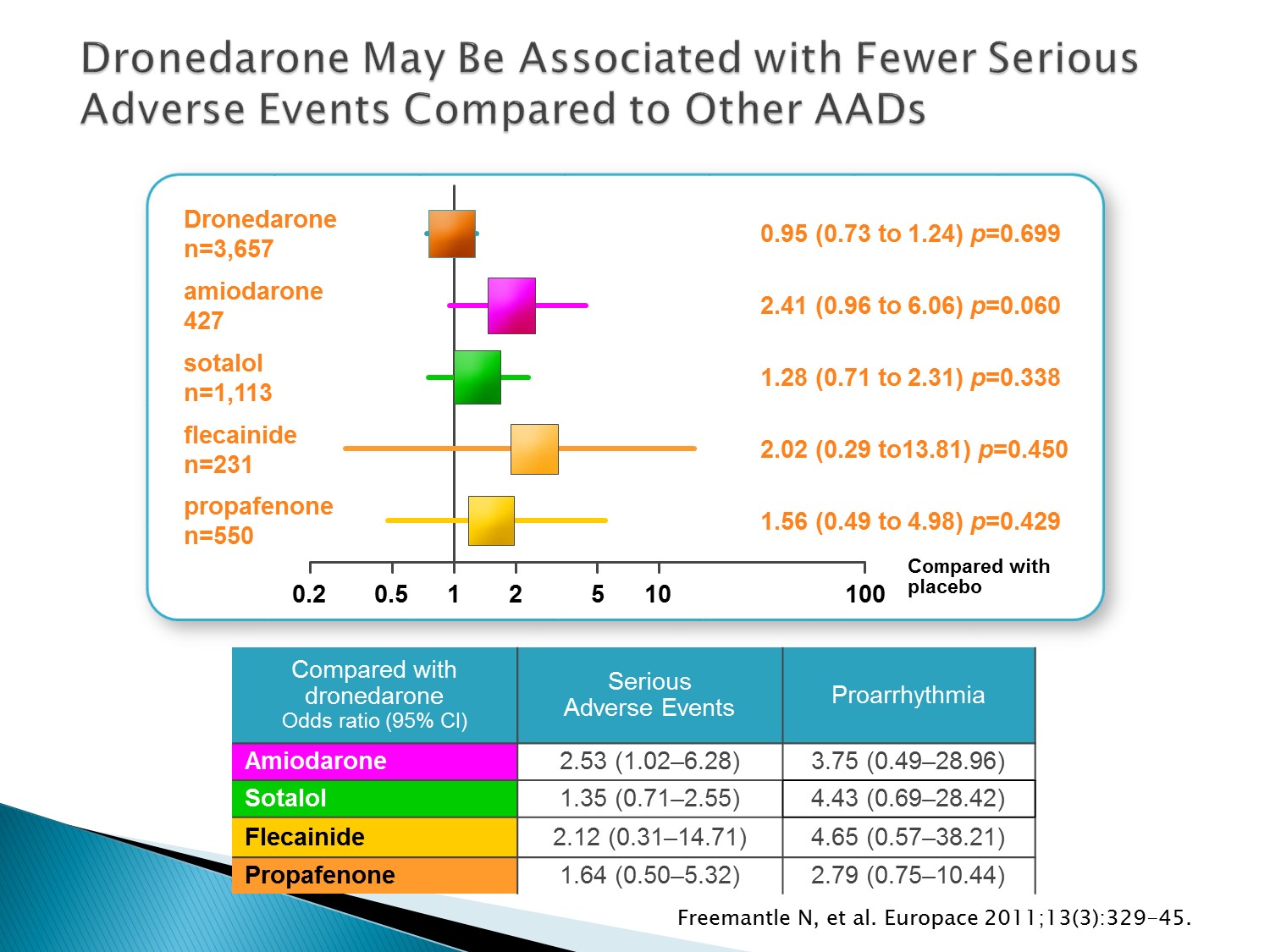
以下為林廷遠醫師ppt檔案原本就有的內容:
Mixed treatment comparison (MTC) is increasingly used to estimate the treatment effects when directly randomised comparisons are not available
Freemantle performed a MTC to compare the risk of morbidity and mortality associated with dronedarone, amiodarone, sotalol, flecainide and propafenone, including the rate of Serious Adverse Events (SAE) associated with each treatment
Freemantle concluded that dronedarone may be associated with less serious adverse events than other AADs, although there is substantial uncertainty on the relative occurrence of SAEs for several AADs
Trials examining effect of AADs in subjects with AF identified using exhaustive searches of Medline and EMBASE
Inclusion criteria:
AF/Atrial Flutter (AFL) population
Randomised Controlled Trials
Exclusion criteria:
Studies enrolling subjects with AF/flutter ≤ 3 months after cardiac surgery.
Minimum duration of follow up for clinical studies: 3 months.
Minimum duration of treatment: 30 days.
Editorials
Case-studies
Outcomes analysed:
All cause mortality
Stroke
Serious Adverse Events
For all serious adverse events:
20 trials / 9734 patients / 1716 experienced at least one SAE
Reference:
Freemantle et al. Europace. 2011;13(3):329-45.
以下為林廷遠醫師ppt檔案原本就有的內容:
Mixed treatment comparison (MTC) is increasingly used to estimate the treatment effects when directly randomised comparisons are not available
Freemantle performed a MTC to compare the risk of morbidity and mortality associated with dronedarone, amiodarone, sotalol, flecainide and propafenone, including the rate of Serious Adverse Events (SAE) associated with each treatment
Freemantle concluded that dronedarone may be associated with less serious adverse events than other AADs, although there is substantial uncertainty on the relative occurrence of SAEs for several AADs
Trials examining effect of AADs in subjects with AF identified using exhaustive searches of Medline and EMBASE
Inclusion criteria:
AF/Atrial Flutter (AFL) population
Randomised Controlled Trials
Exclusion criteria:
Studies enrolling subjects with AF/flutter ≤ 3 months after cardiac surgery.
Minimum duration of follow up for clinical studies: 3 months.
Minimum duration of treatment: 30 days.
Editorials
Case-studies
Outcomes analysed:
All cause mortality
Stroke
Serious Adverse Events
For all serious adverse events:
20 trials / 9734 patients / 1716 experienced at least one SAE
Reference:
Freemantle et al. Europace. 2011;13(3):329-45.

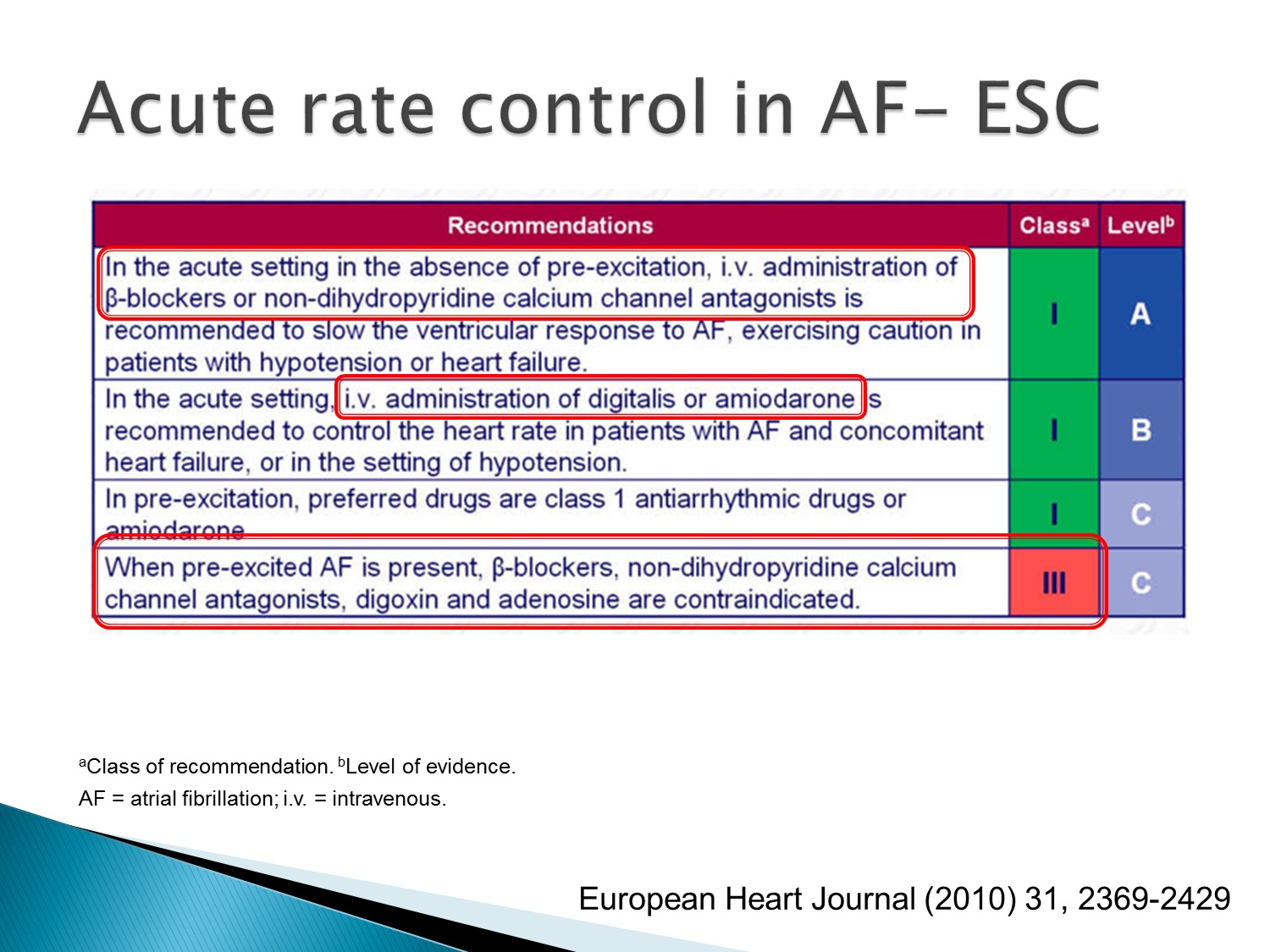
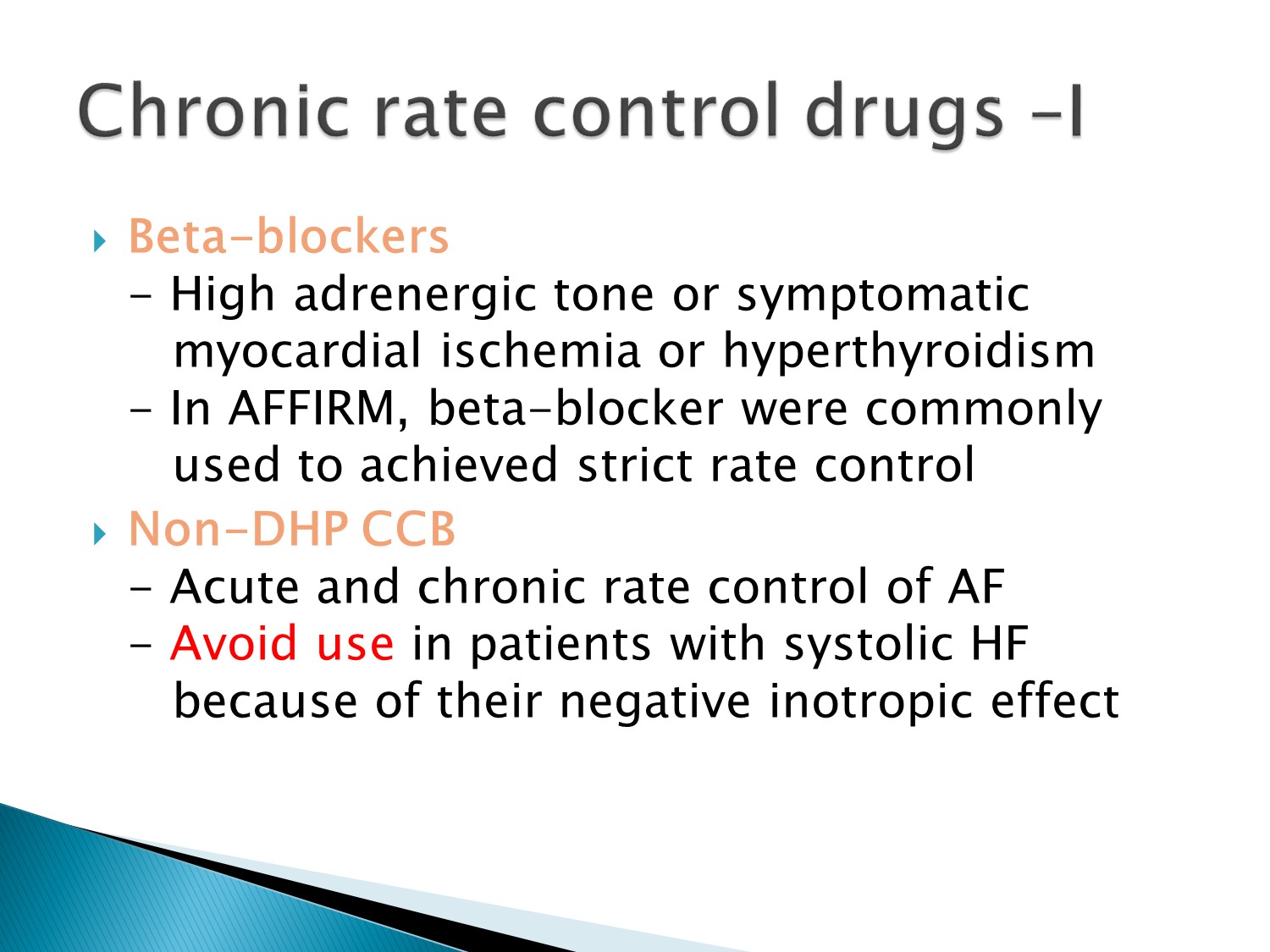
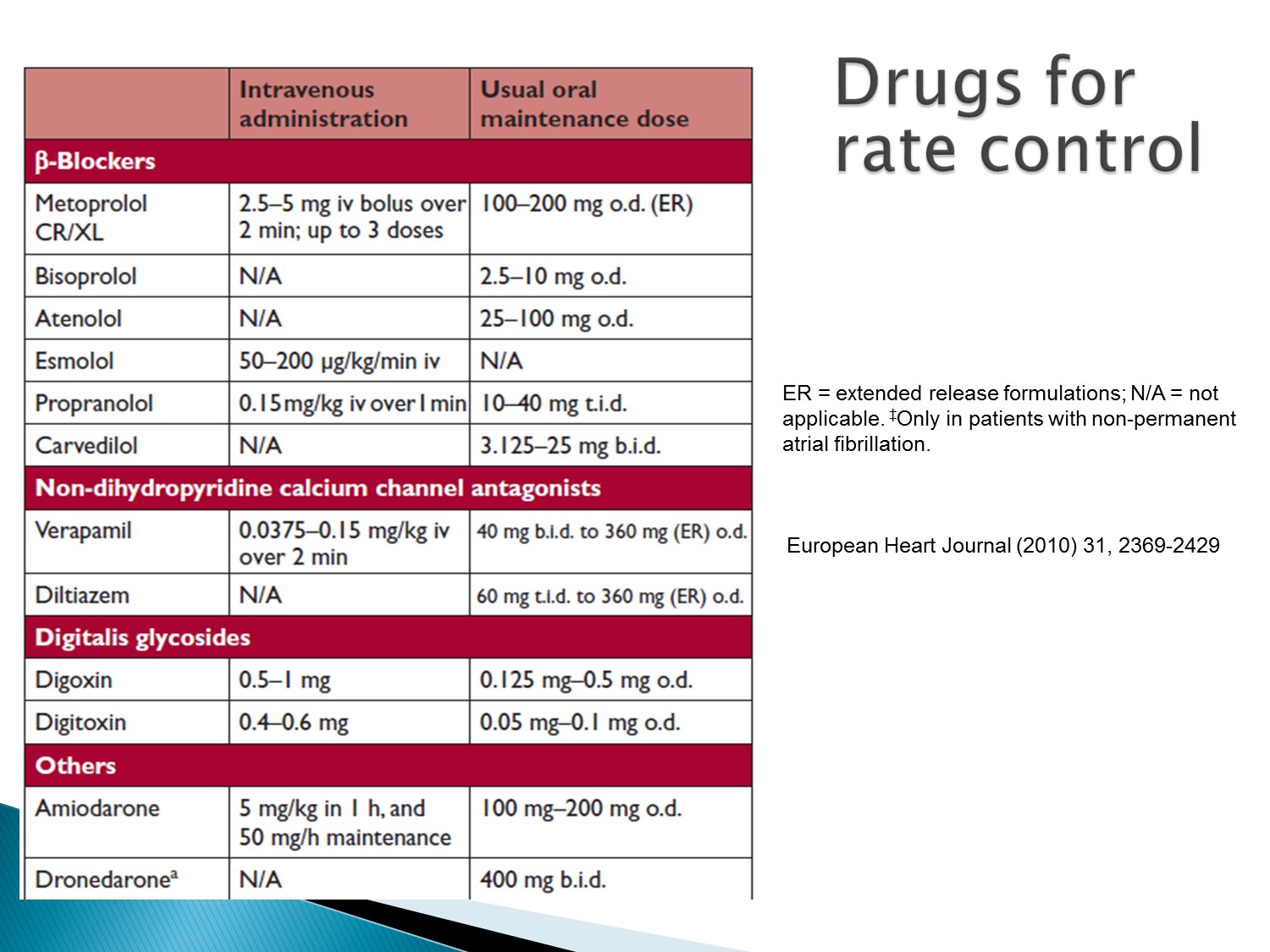
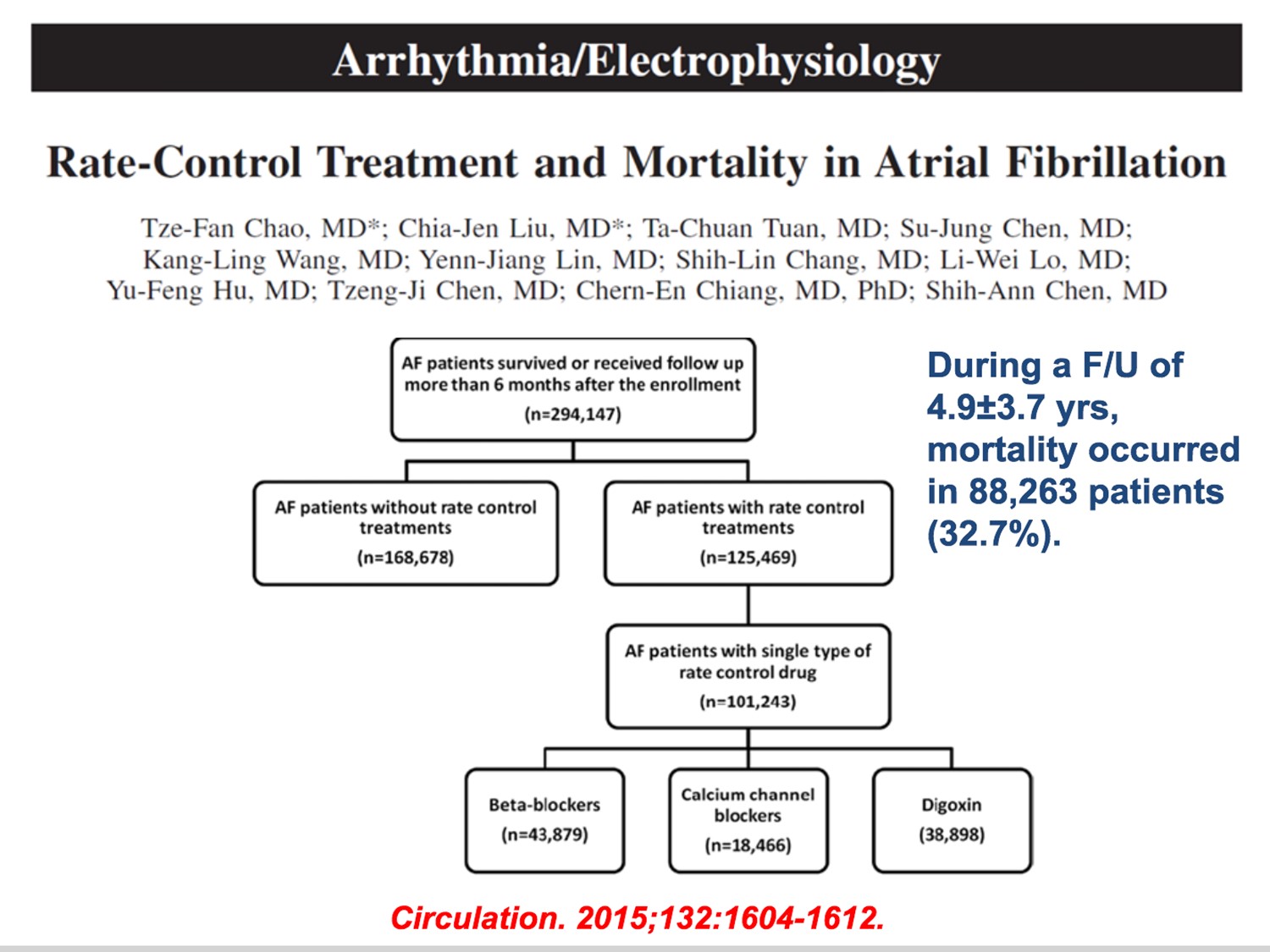
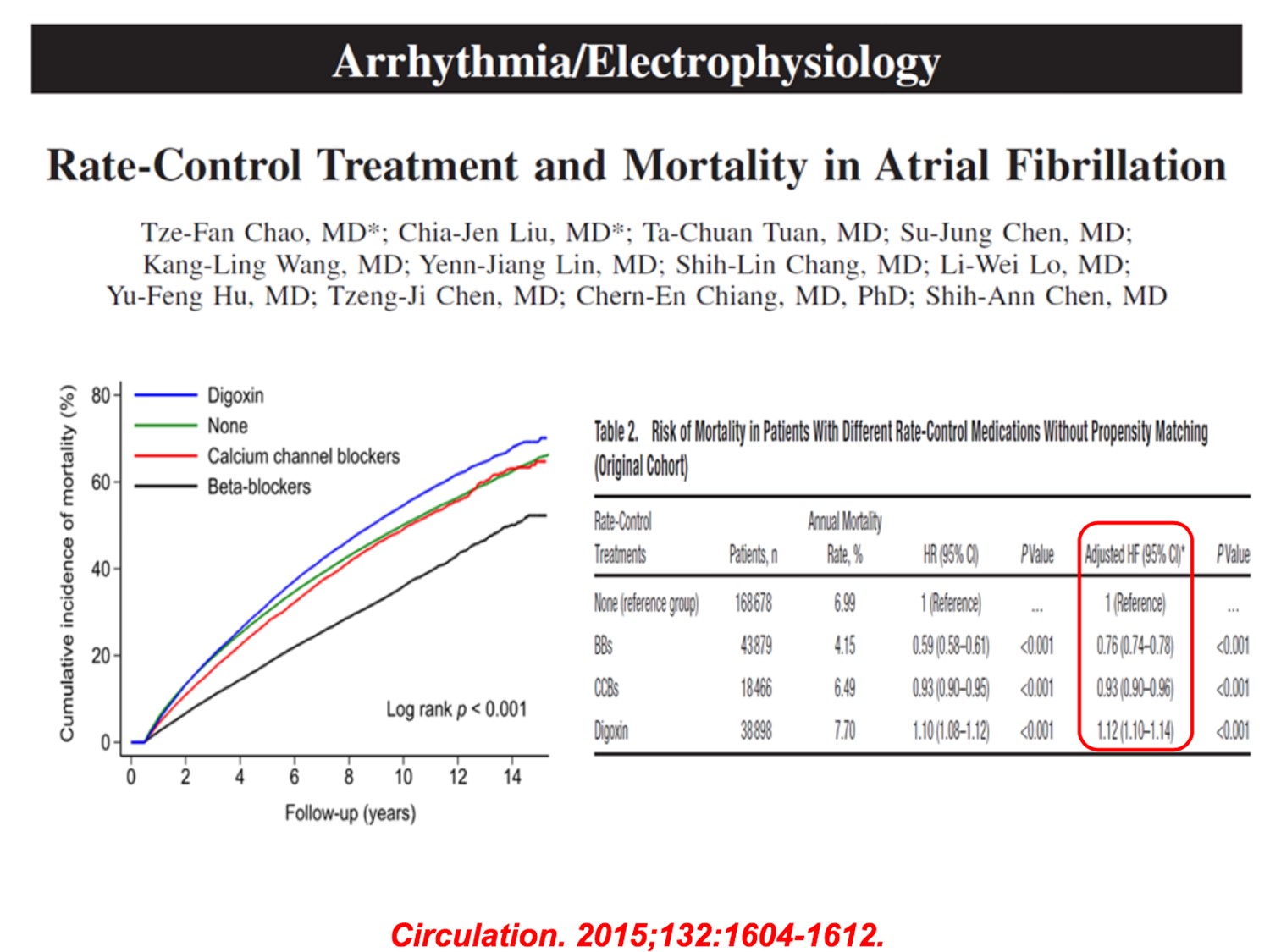
首選 IV beta blocker、IV non-DHP CCB
但當 Af 同時併有 HF、hypotension 時,使用 digoxin 或 amiodarone
但當有 pre-excitation A fib 時,不可用 beta blocker、CCB、Digoxin、adenosine
(2010 年未列 amiodarone,但是實際上不能用,後來 2014 年改版已加入)
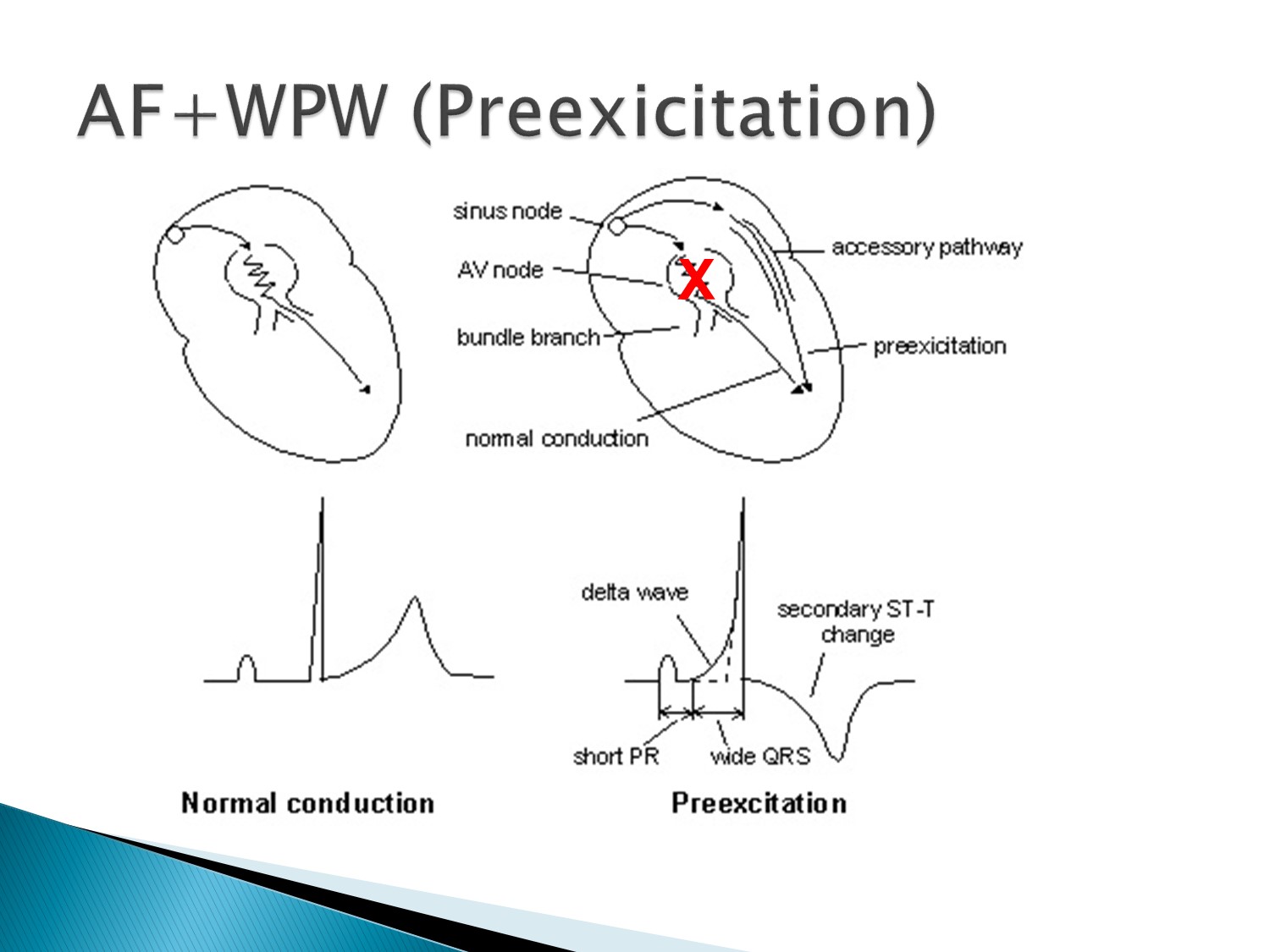
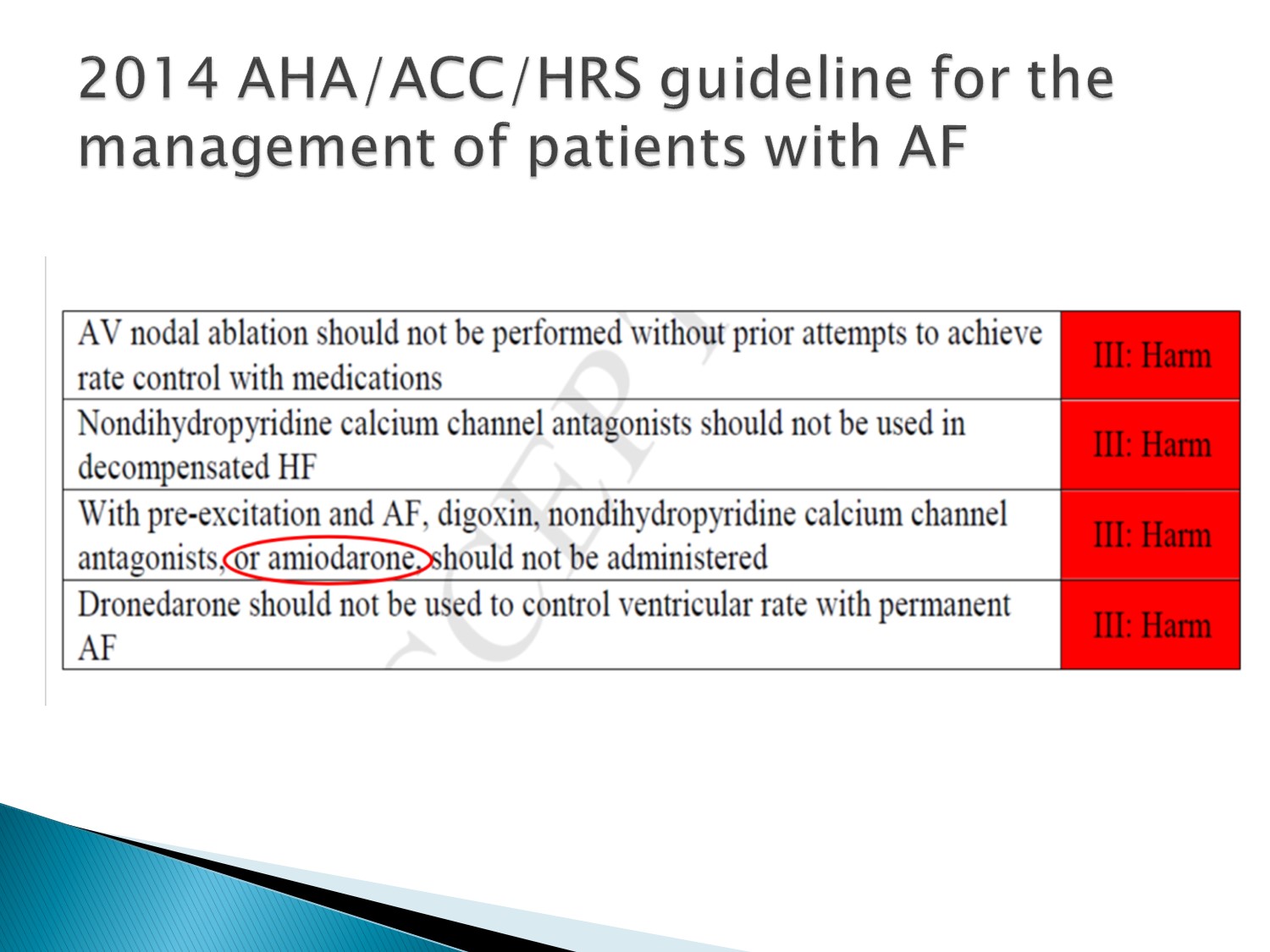
2014 年改版,當有 pre-excitation A fib 時,amiodarone 也是不可使用的
(台灣只能電擊)
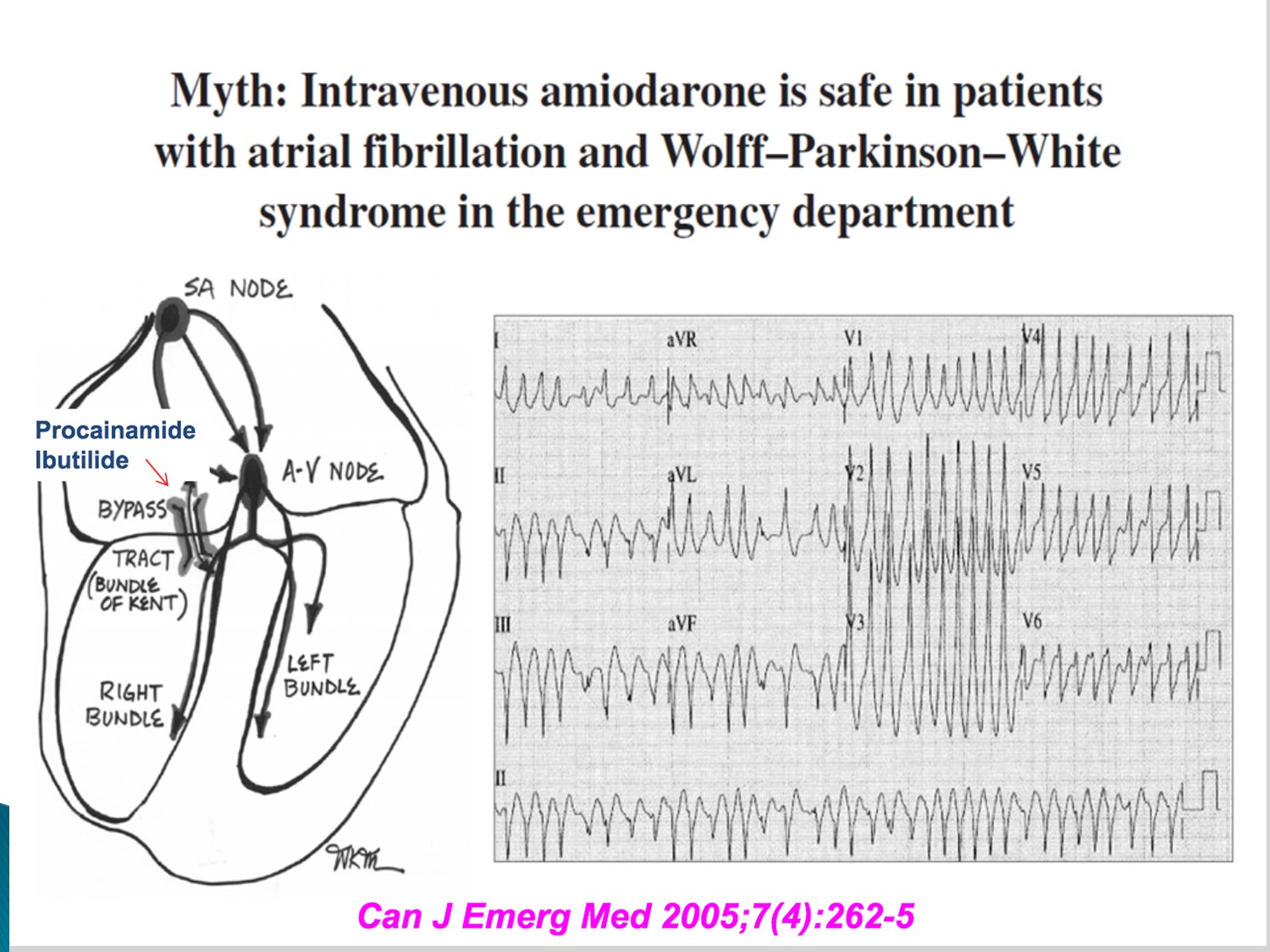
Ia、Ic 可以 block AV node 及 accessory pathway
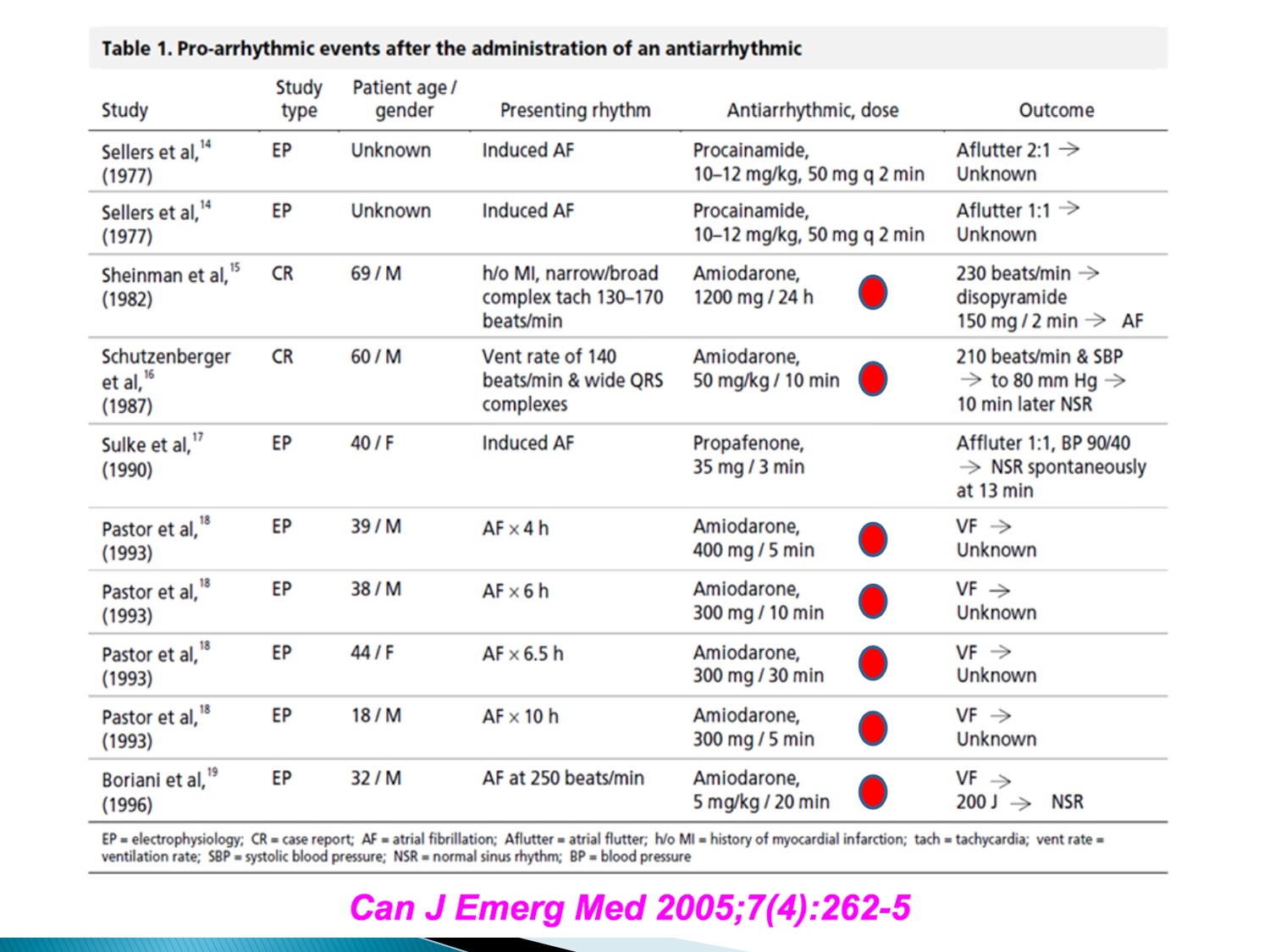
Amiodarone 會使 Afib + WPW 變成 VF,而需要電擊
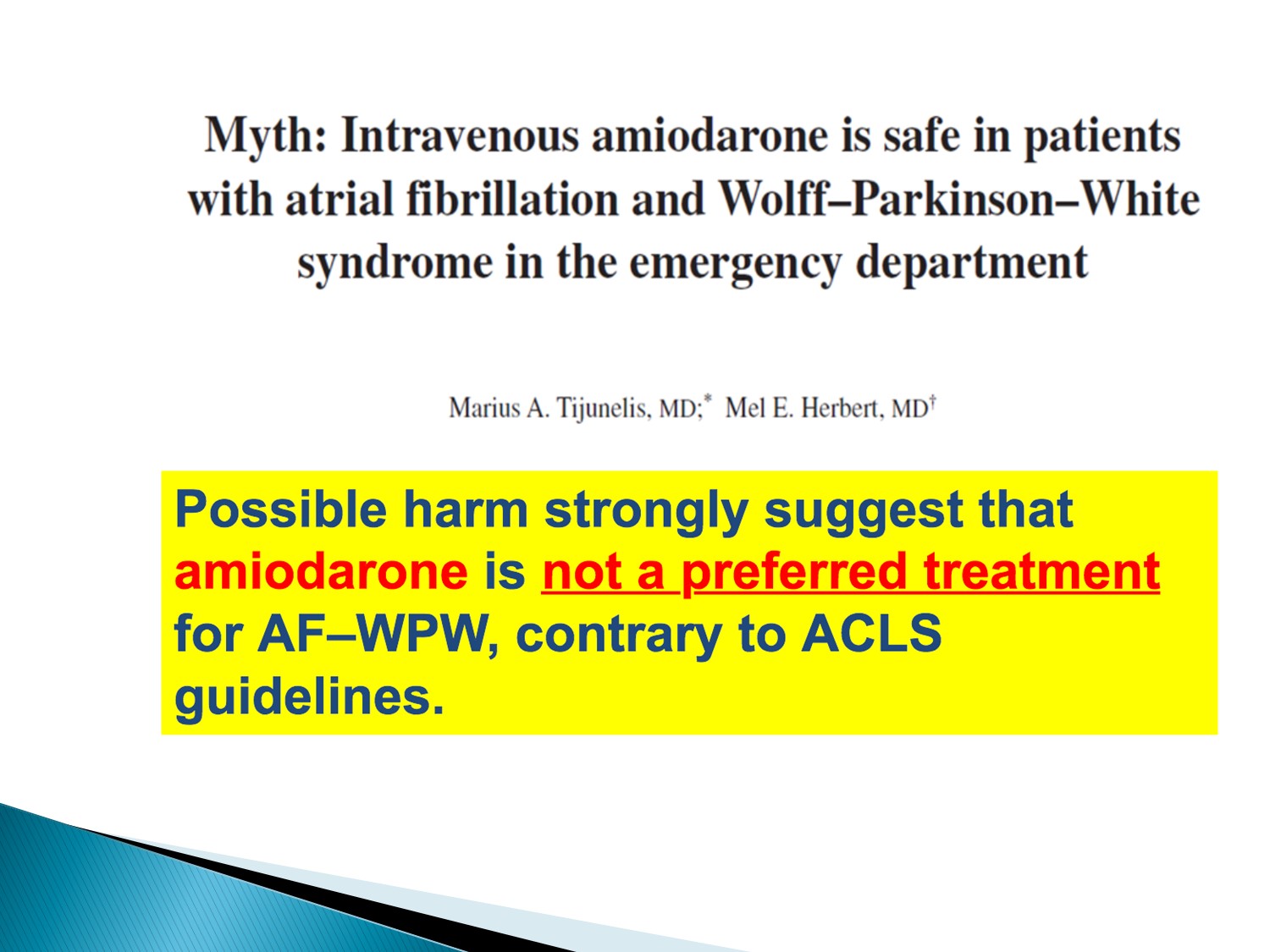
故 A fib + WPW 不可使用 amiodarone
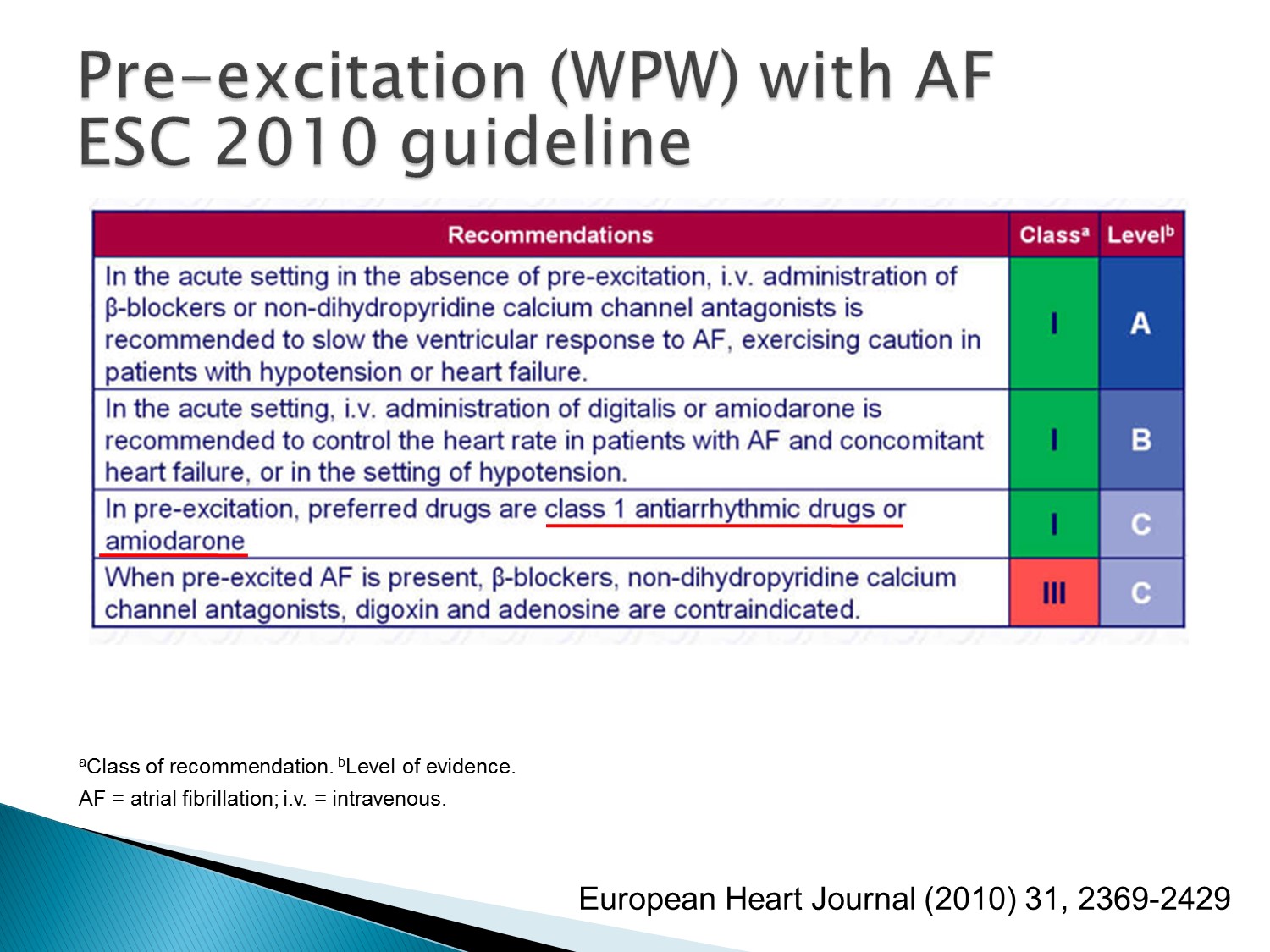
原本 2010 年 guideline,amiodarone 在 pre-excitation 是 class I
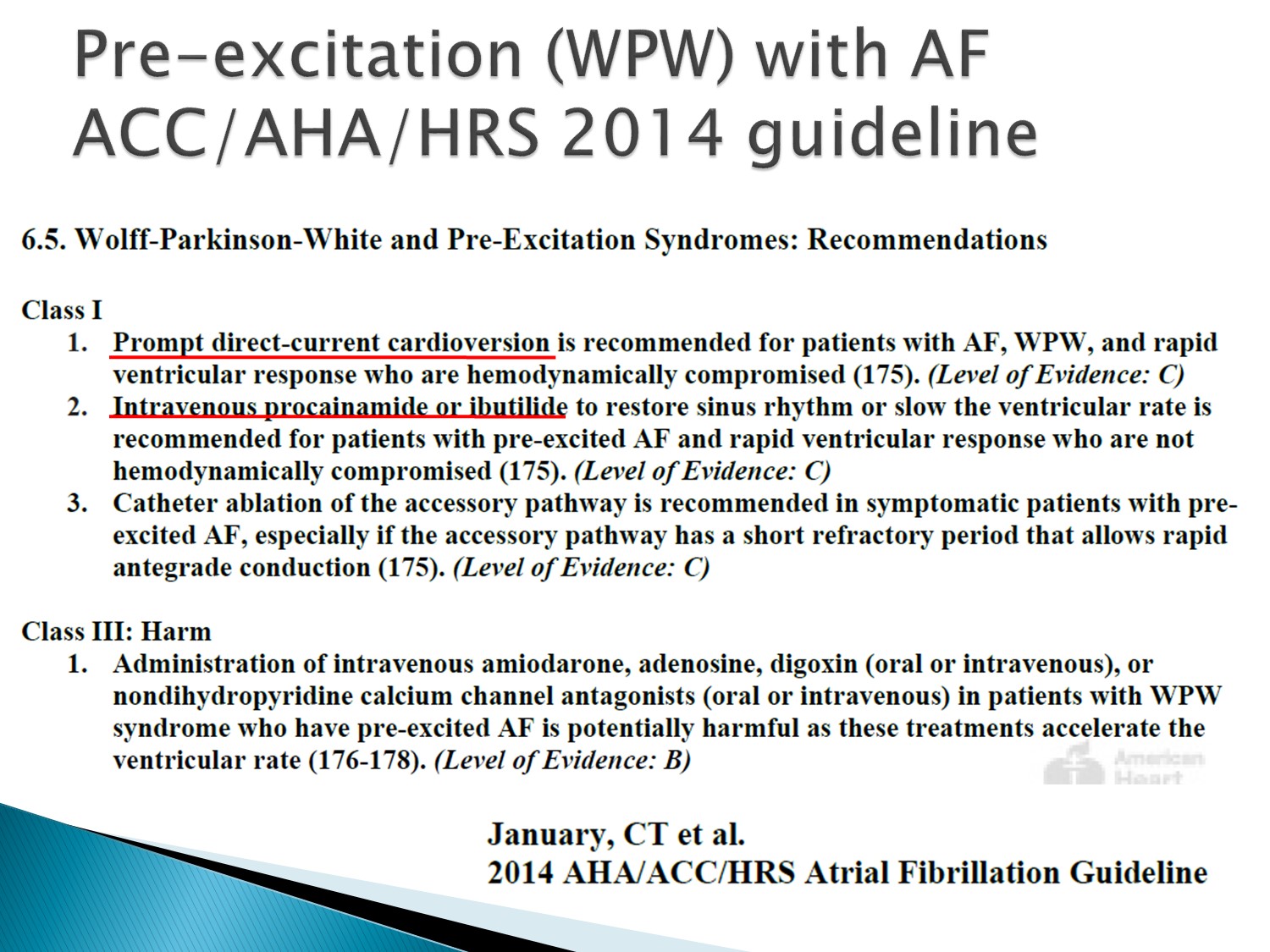
到 2014 年 guideline,amiodarone 變成 class III (有害)
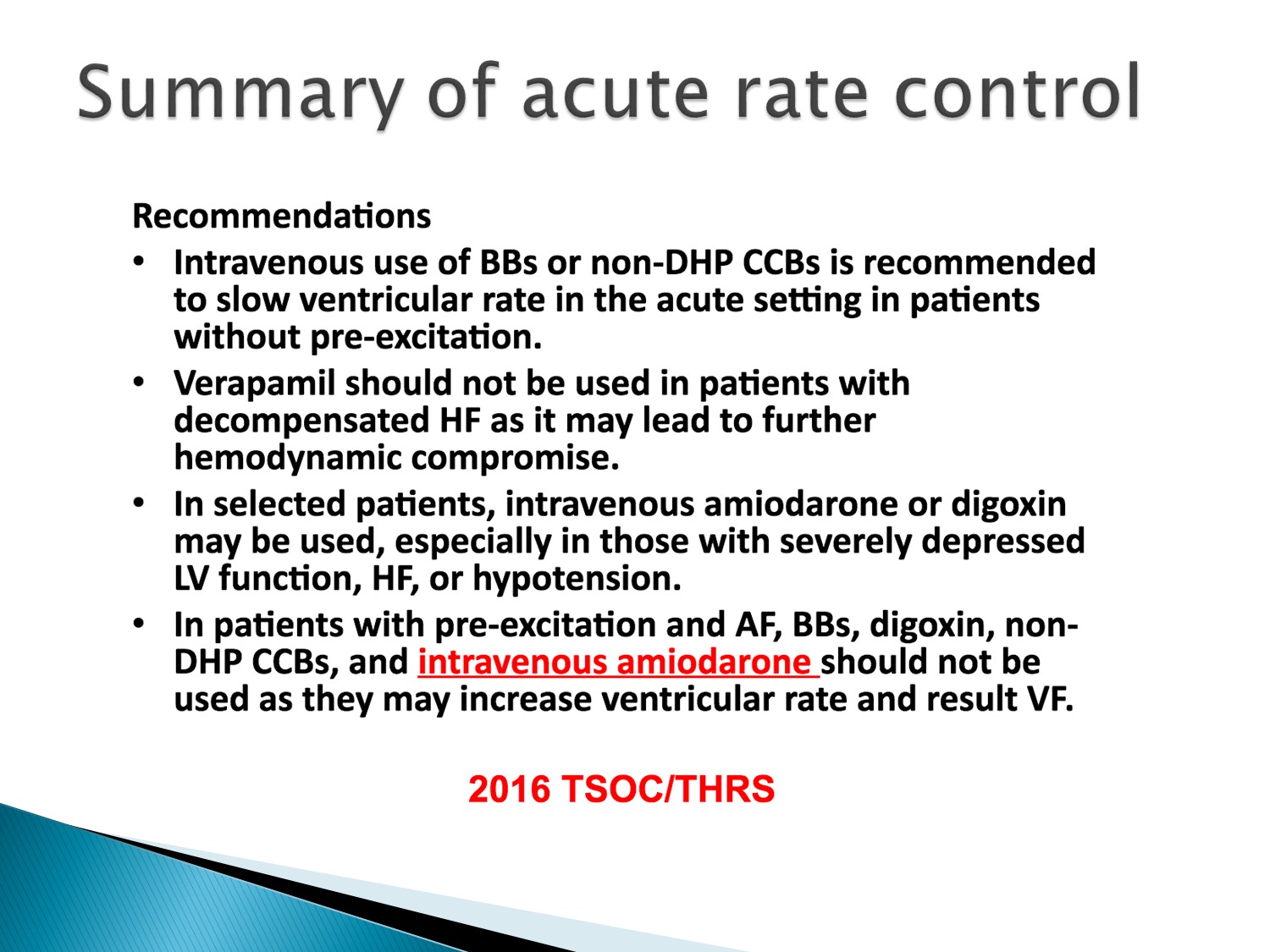
台灣心臟學會:IV amiodarone 在 pre-excitation A fib 是禁忌症
總結:
Acute rate control:選 beta blocker、CCB
若 HF 或 hemodynamic 不穩:amiodarone 或 digoxin
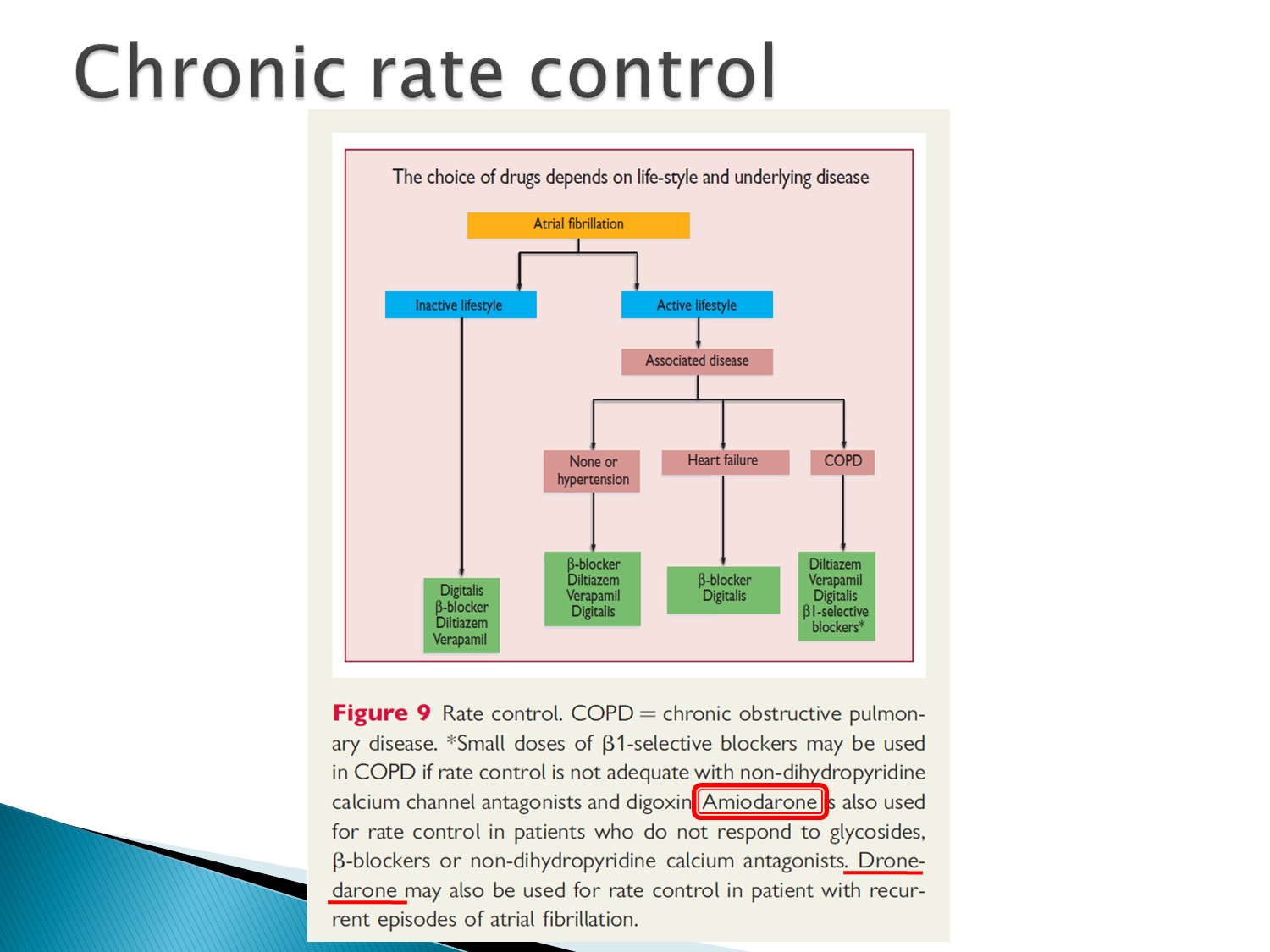
看 underlying disease:
COPD:beta 1 selective beta blocker、CCB
HF:beta blocker、digoxin
Hypertension:beta blocker、CCB、digoxin
Amiodarone 在上述藥物使用後,效果不佳時才使用
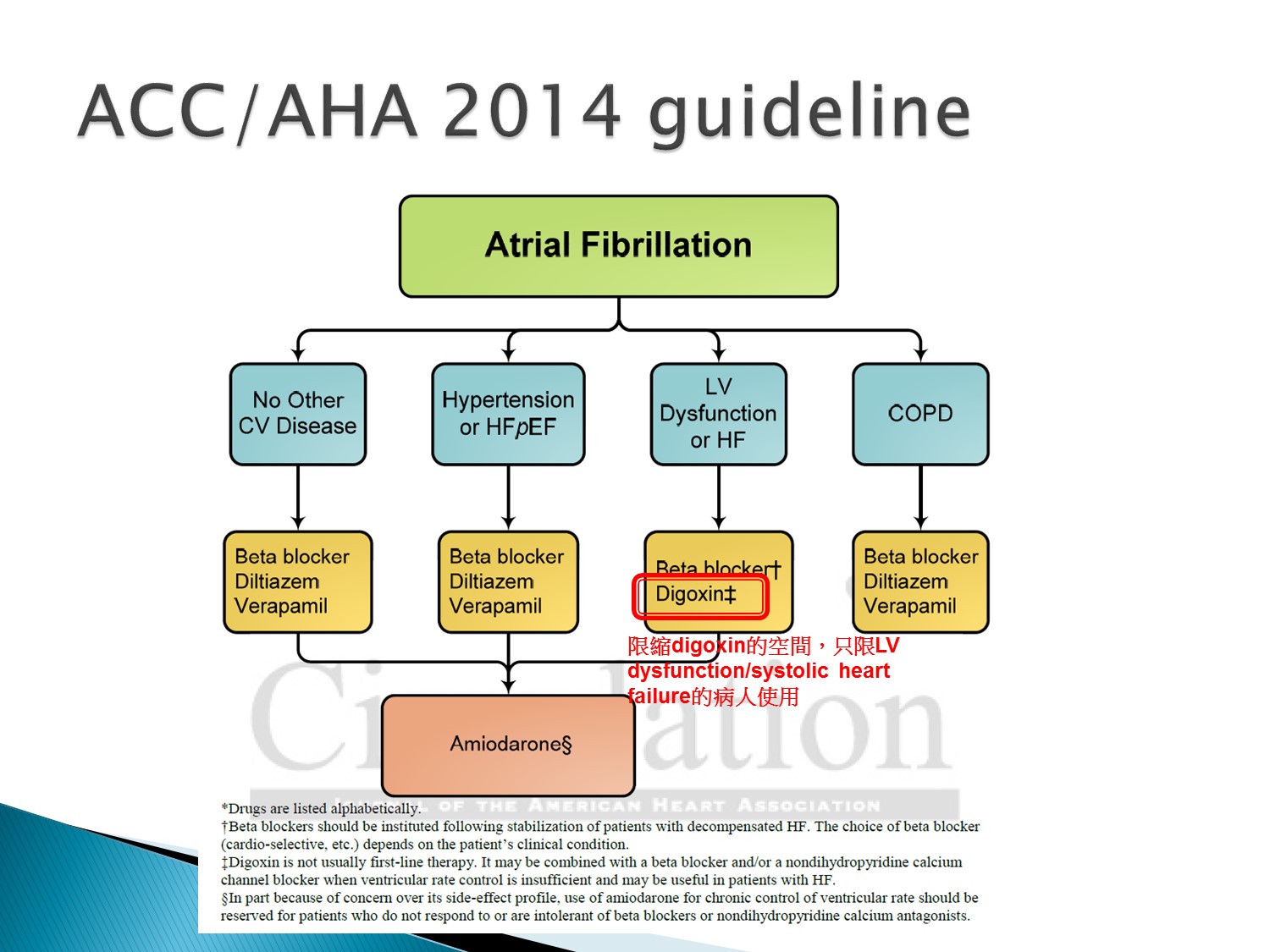
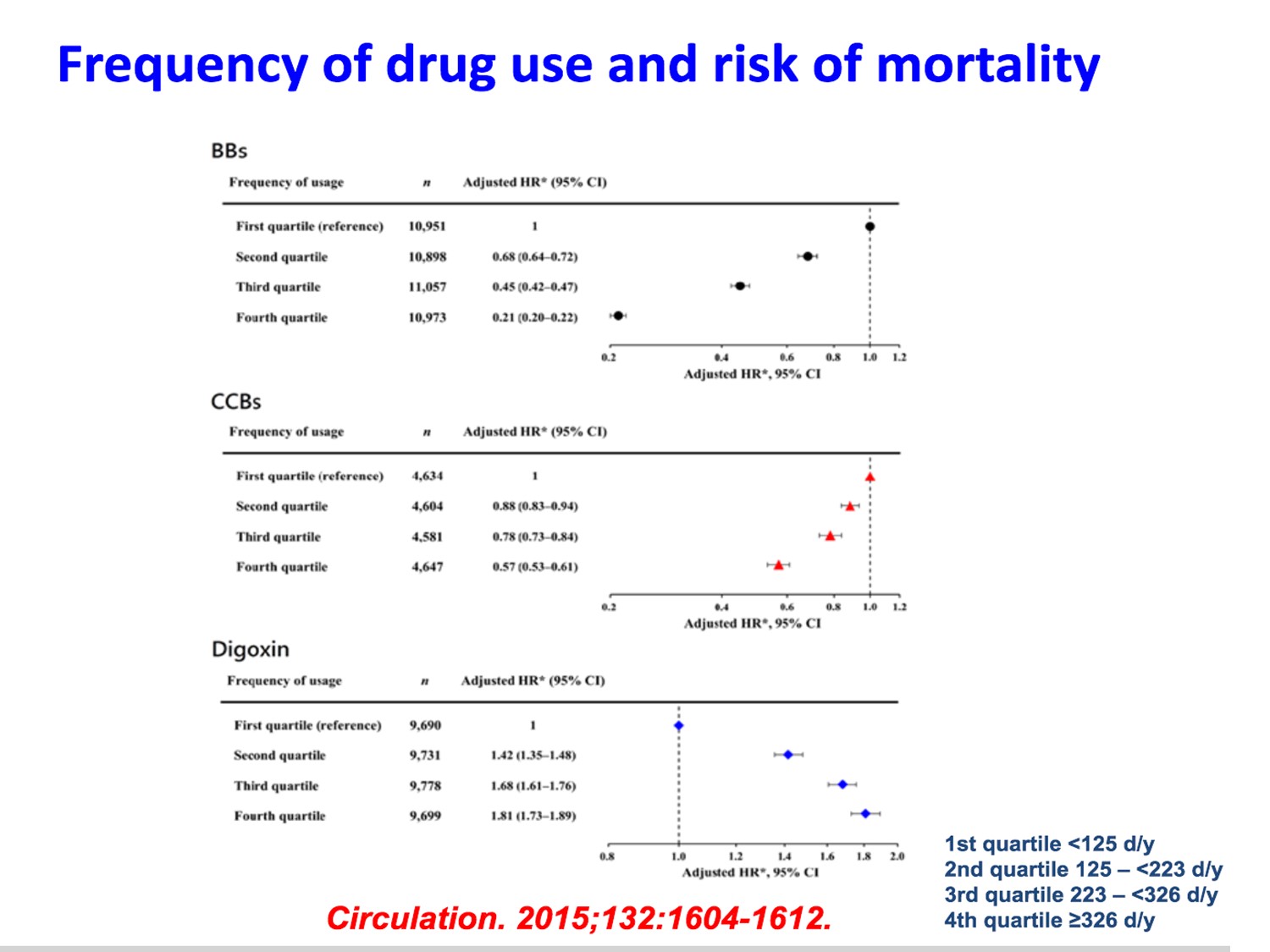
Digoxin 的角色限縮,只用在 systolic heart failure 病人身上
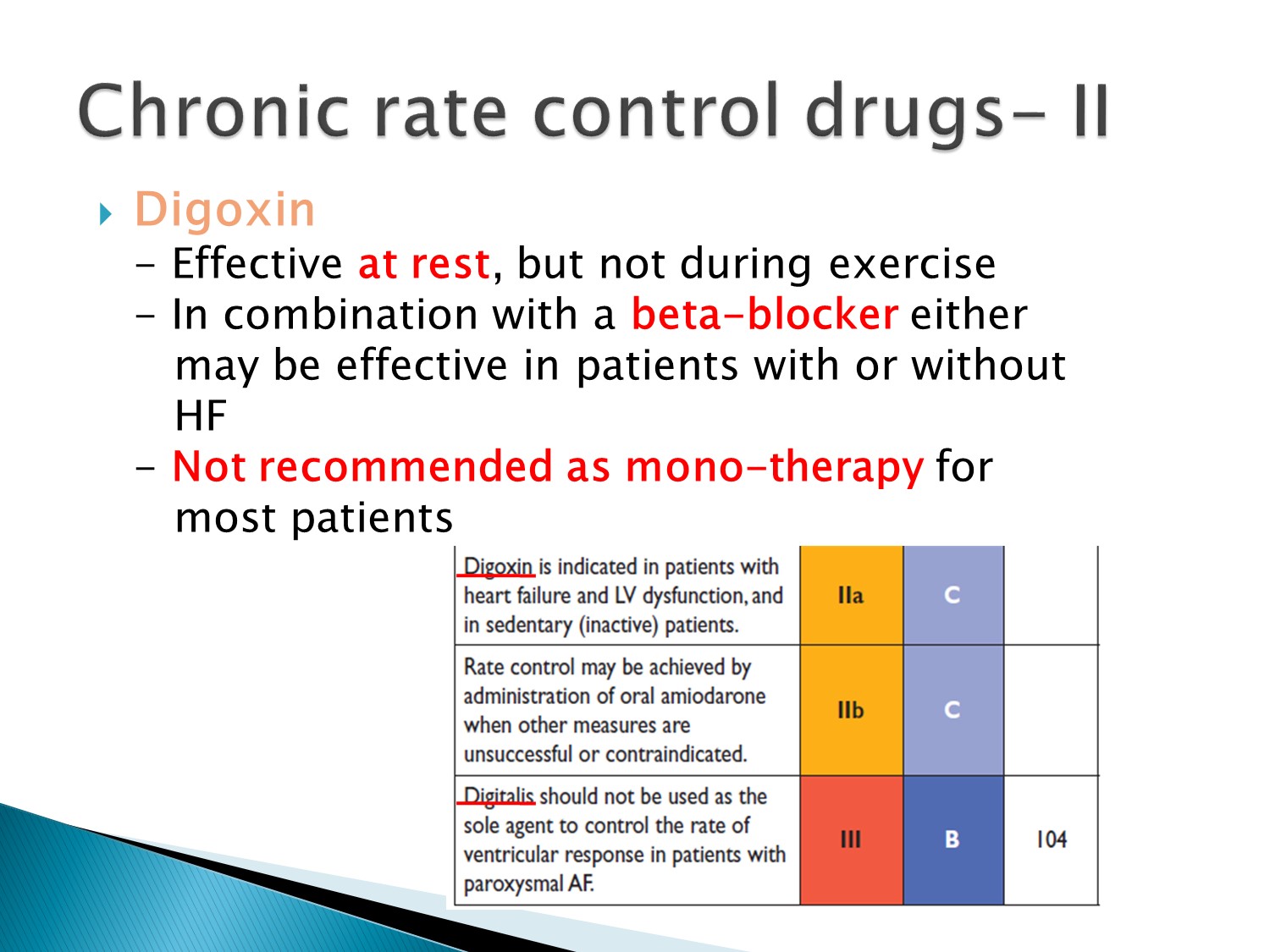
Digoxin 的效果差,對於臥床者效果 OK,但對有活動者效果差
不建議單獨使用,建議與 beta blocker 併用
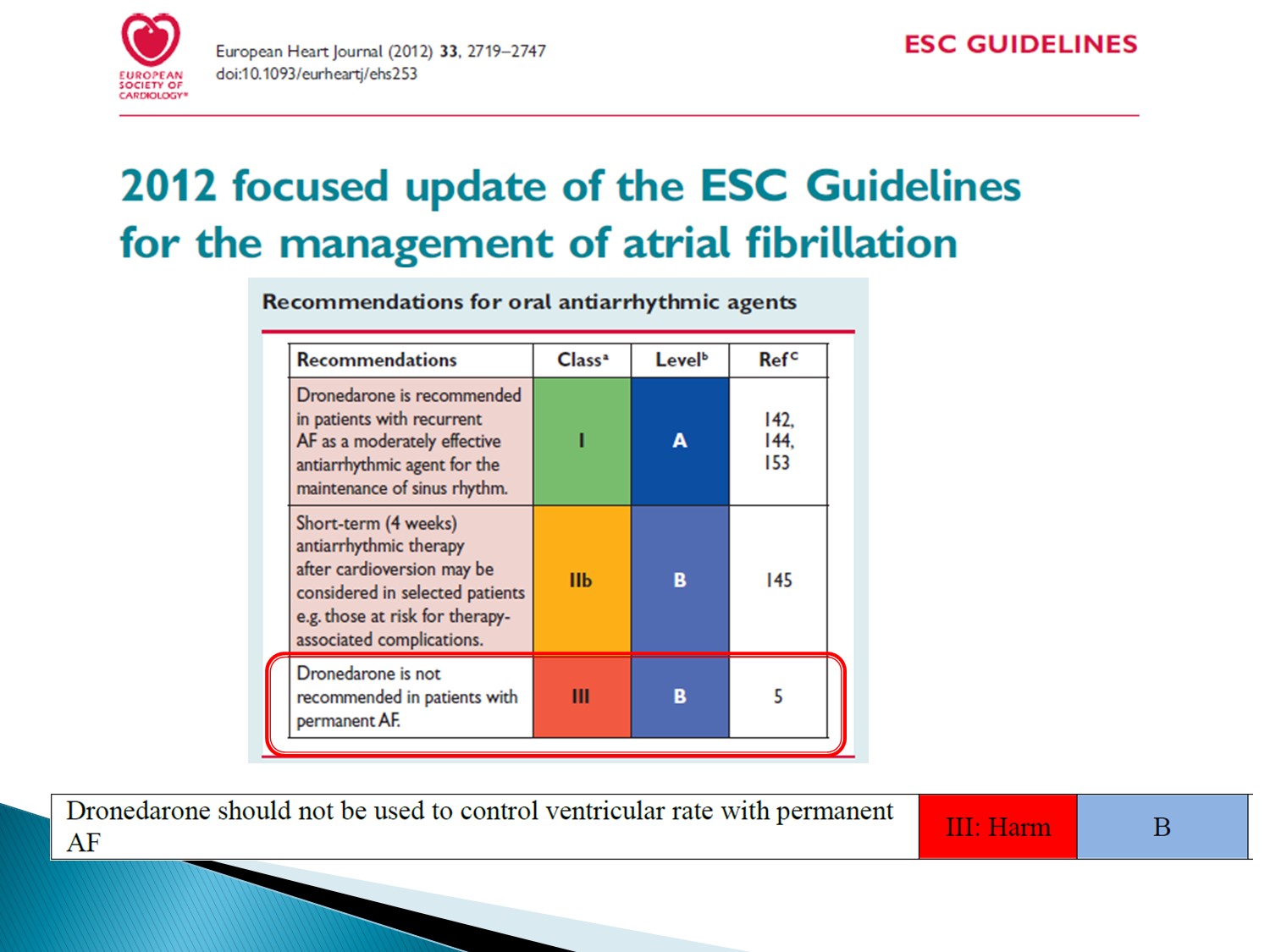
Permanent A fib 不可使用 dronedarone
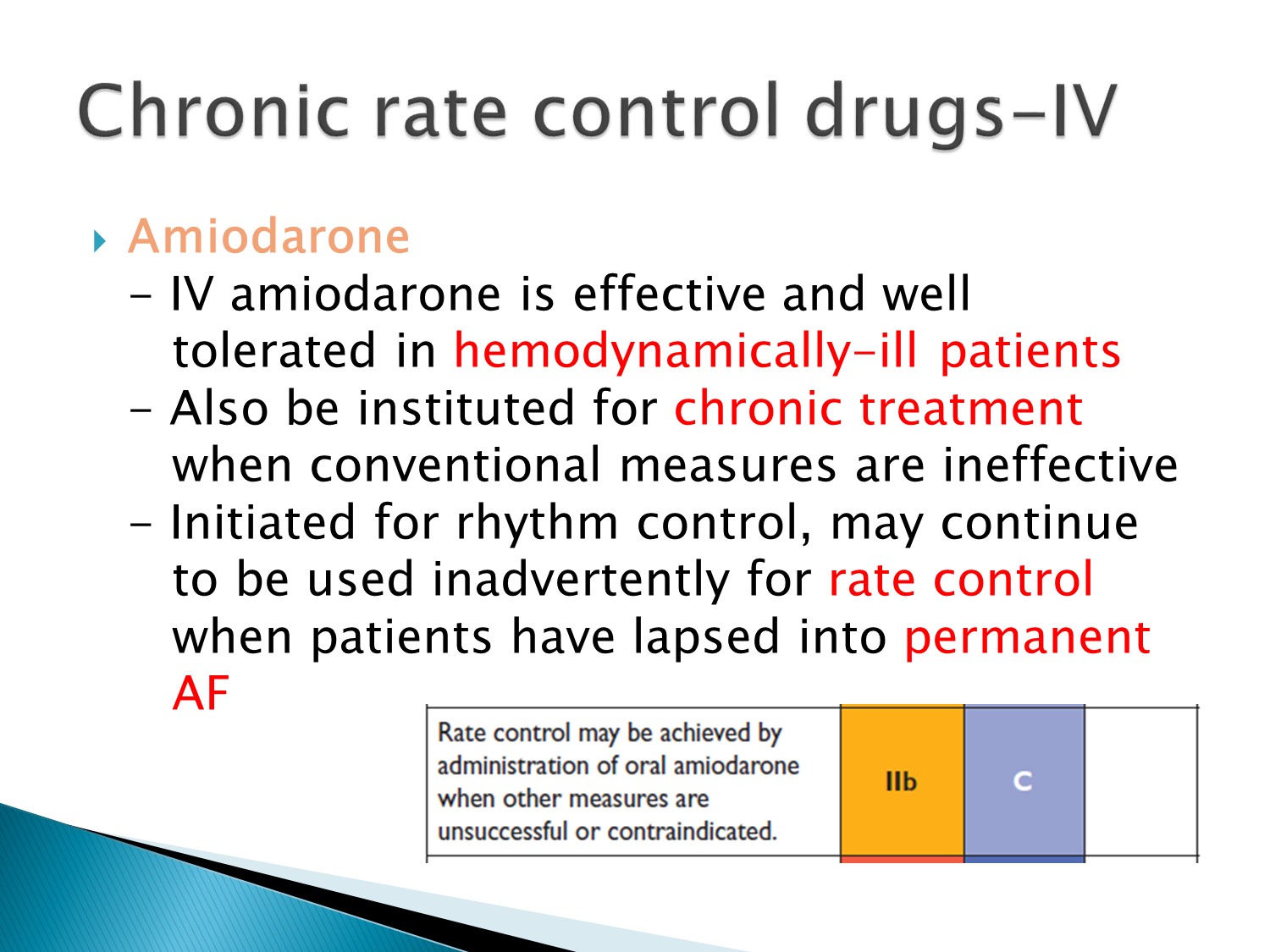
Amiodarone 可以用在 rate 及 rhythm control,只是較為後線
對於 hemodynamic 不好者可以用
慢性使用要小心副作用


Q1.CADàstructural heart diseaseà不可用Icà沒HF、沒permanent Afibà選dronedarone
Q2.理論上LVEF<35%才不可用dronedarone,但建議有HF就不要用à選amiodarone
Q3.有COPD、HTNà選CCB、beta blocker(beta 1)à效果不好再用amiodarone
Q4.有HF,選beta blocker或digoxin
