
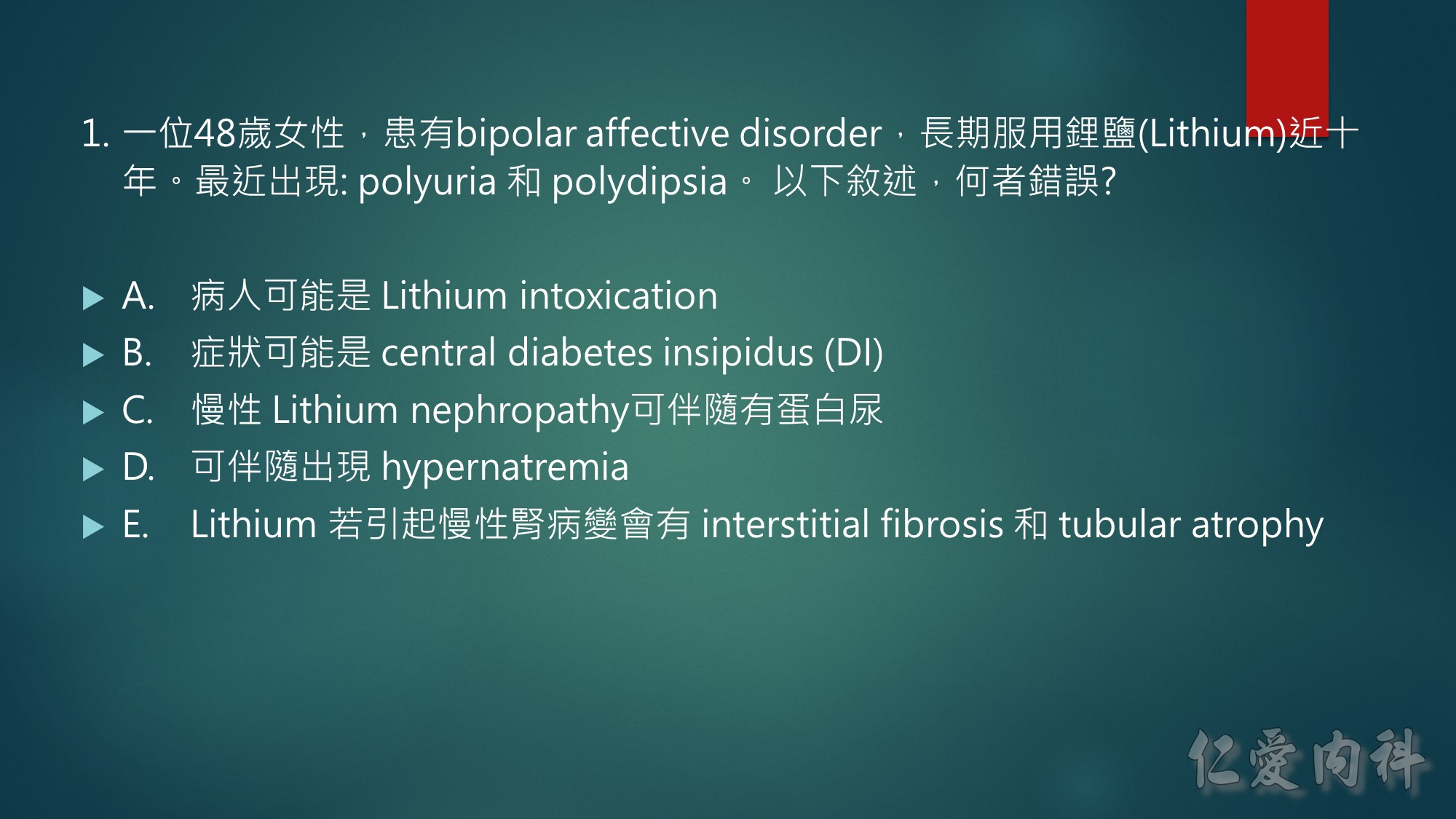
Tubular 遠端
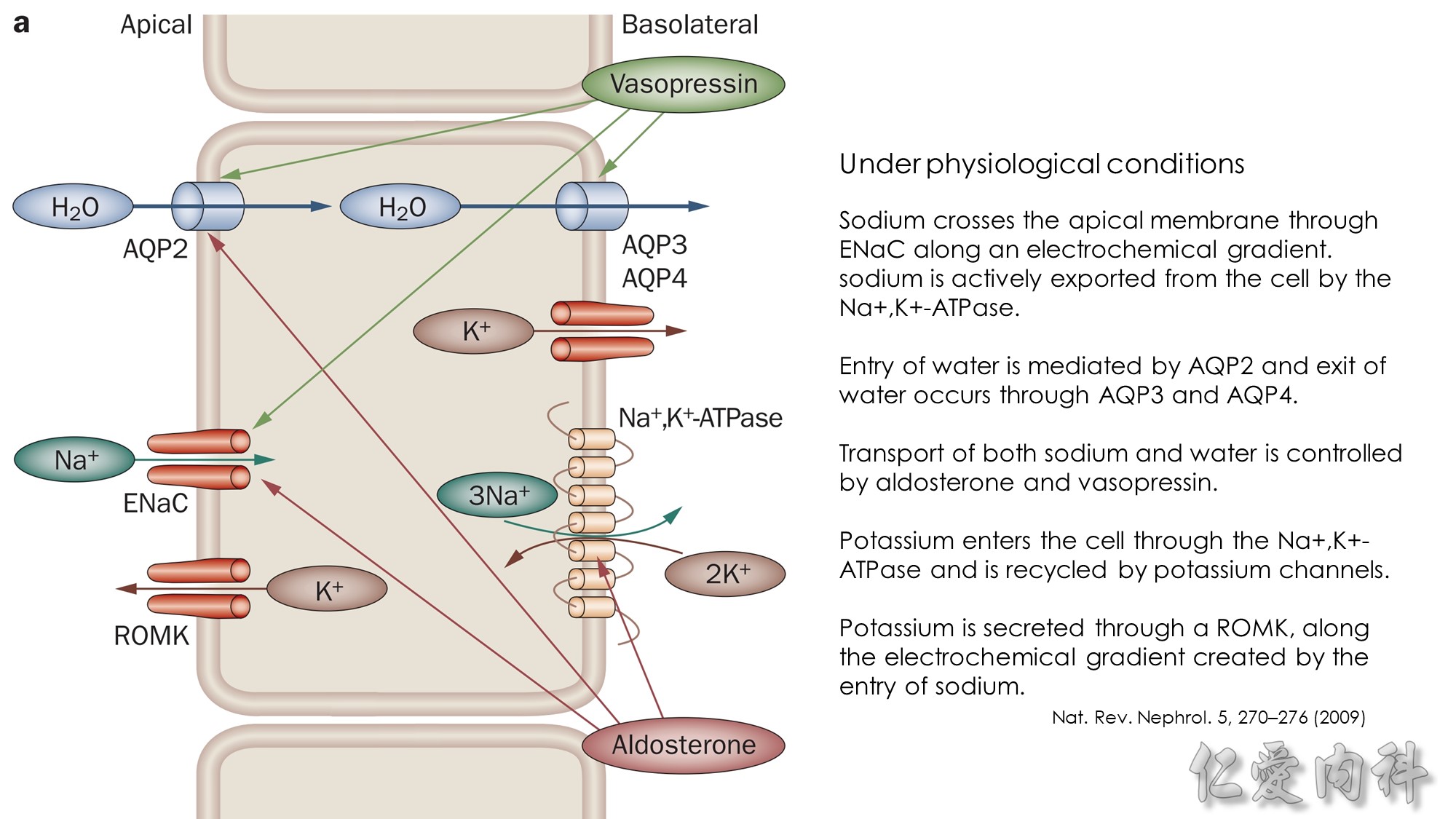
* ADH(vasopressin)作用在AQP2(Aquaporin 2) receptor→吸水
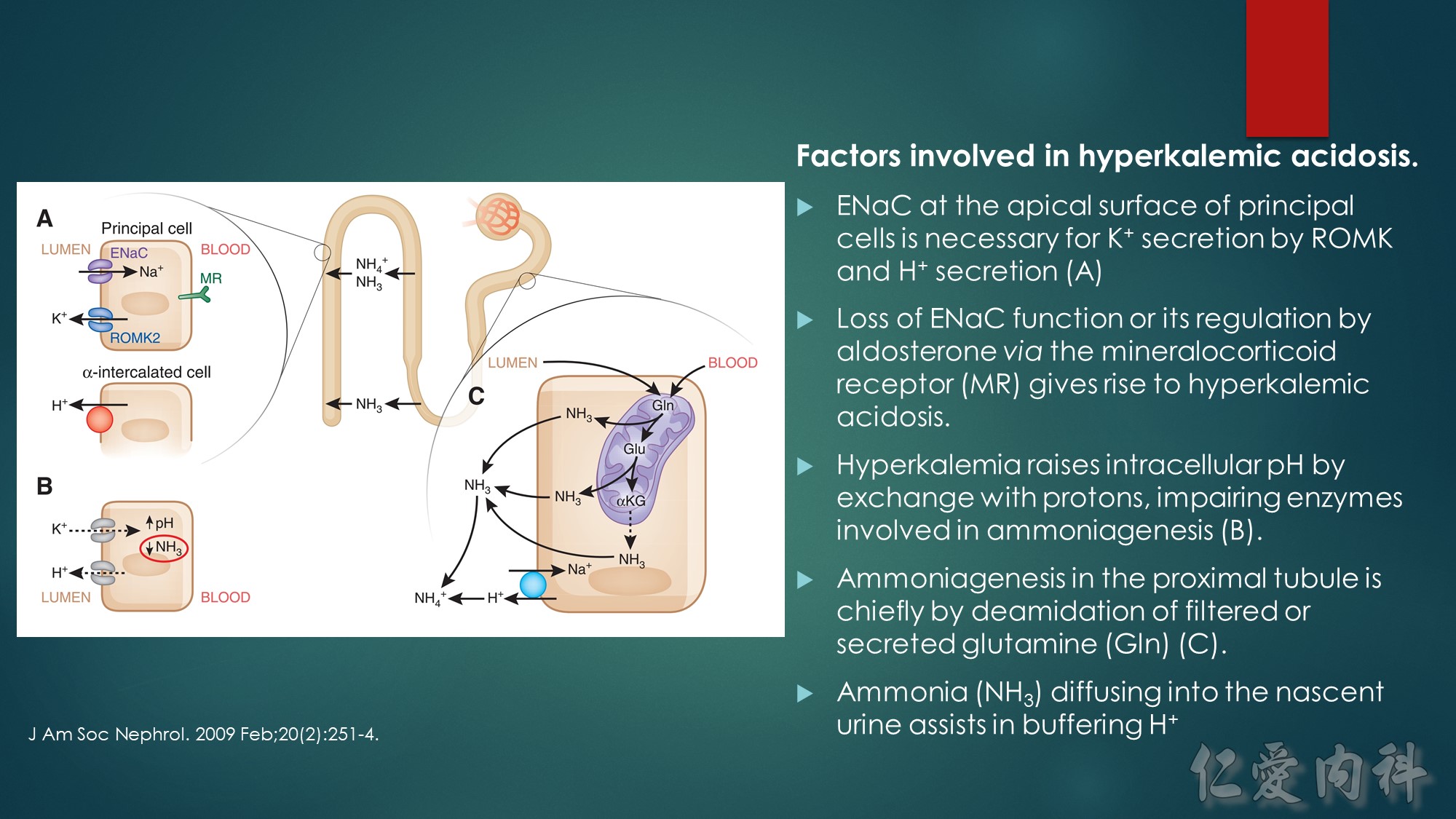
* Aldosterone則作用在三個channel(Na-K ATPase, ENaC, potassium channel),作用在Na-K-ATPase致Na打出細胞、K進細胞產生gradien後Na從apical端ENaC進細胞,一個陽離子進入伴隨一個陽離子出去,因此一個K從apical 端出細胞,有時是H出去→因此secondary hypertension/aldosteronism的病人會低血鉀、alkalosis、Na高血壓高。
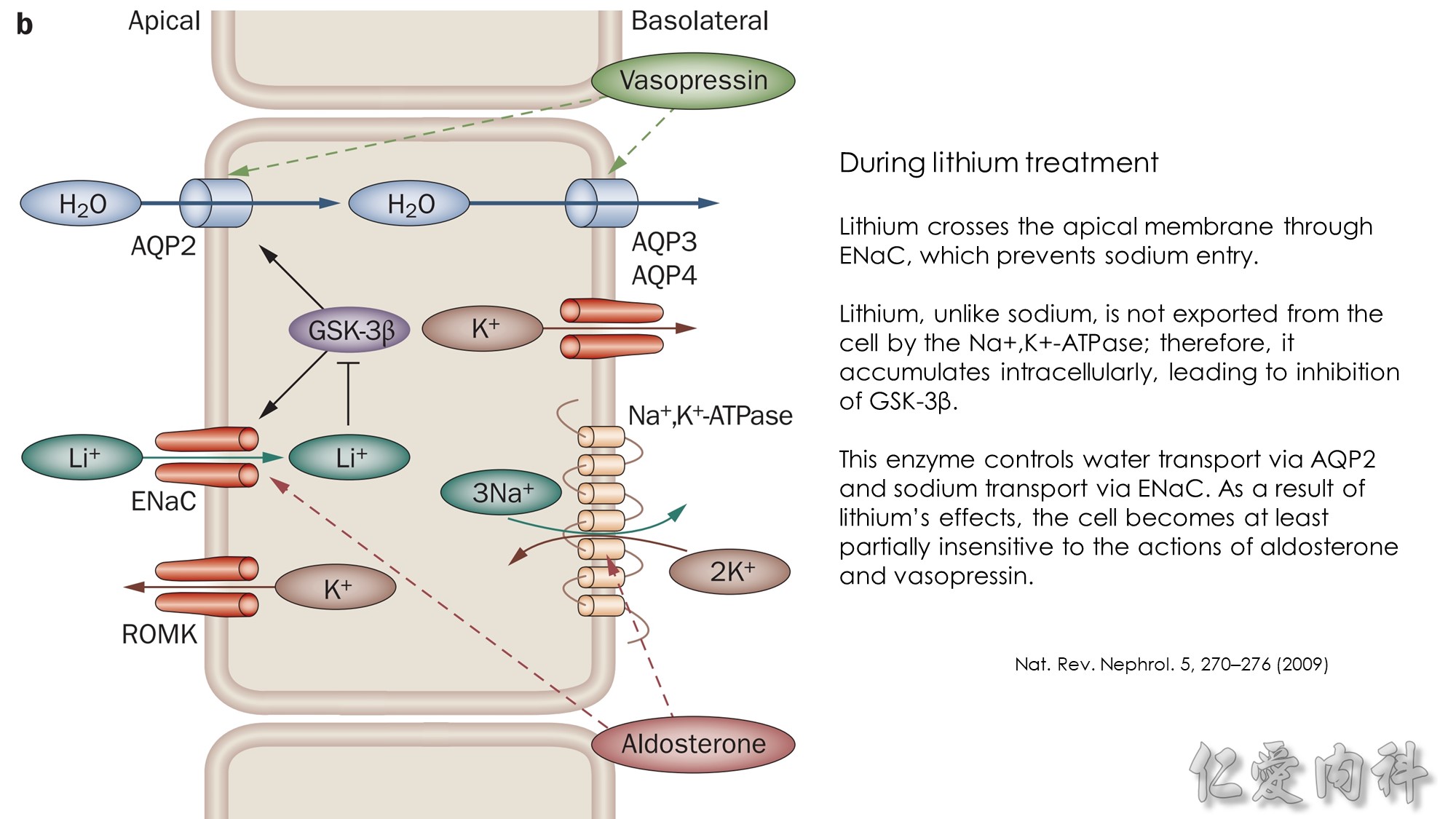
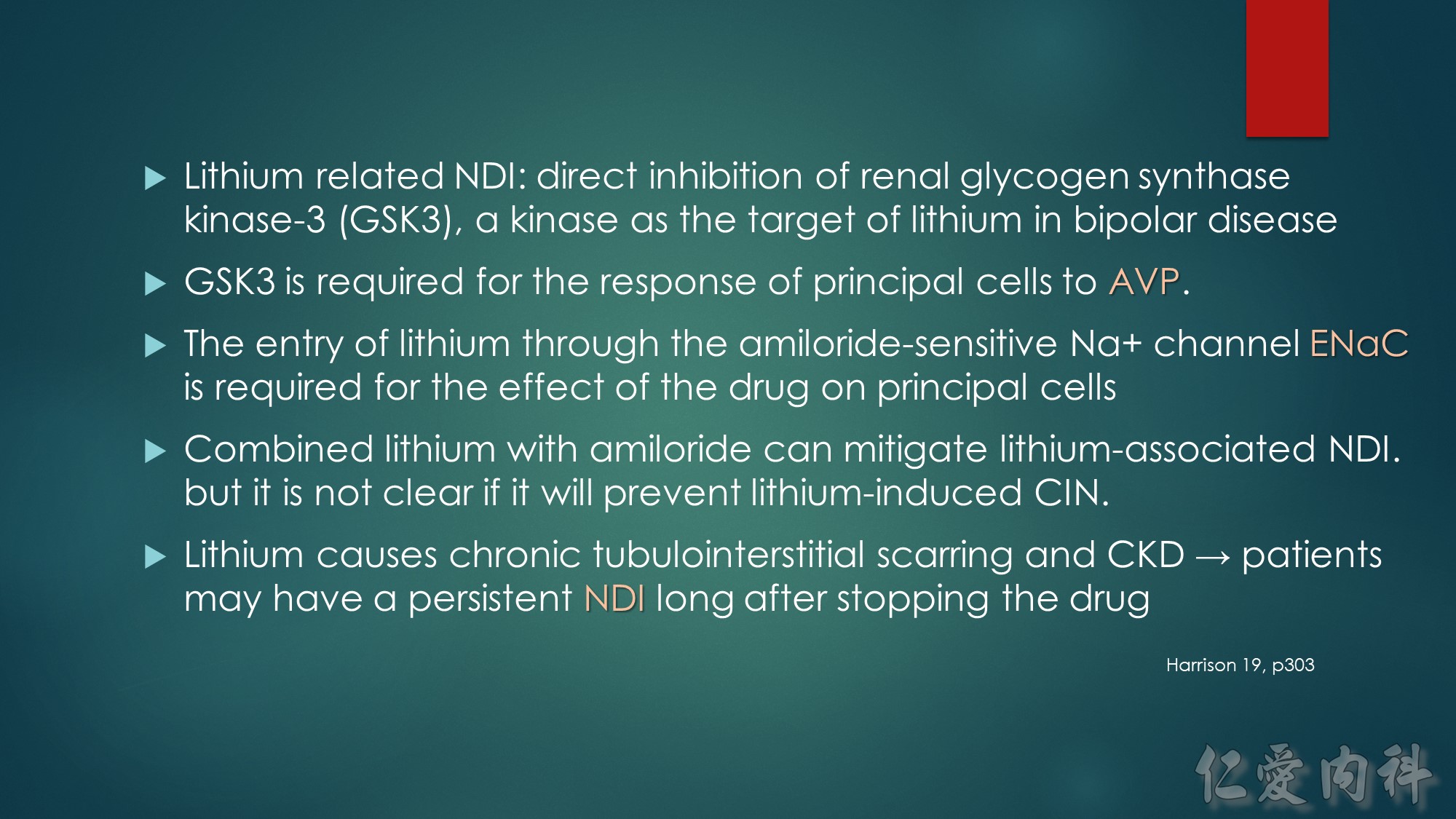
Lithium由Apical端ENaC進入細胞,但無法從Na-K-ATPase出細胞,因此在細胞內累積,累積的lithium會抑制GSK-3beta的作用,進一步抑制AQP2、ENaC的作用,無法留住水→Nephrogenic DI
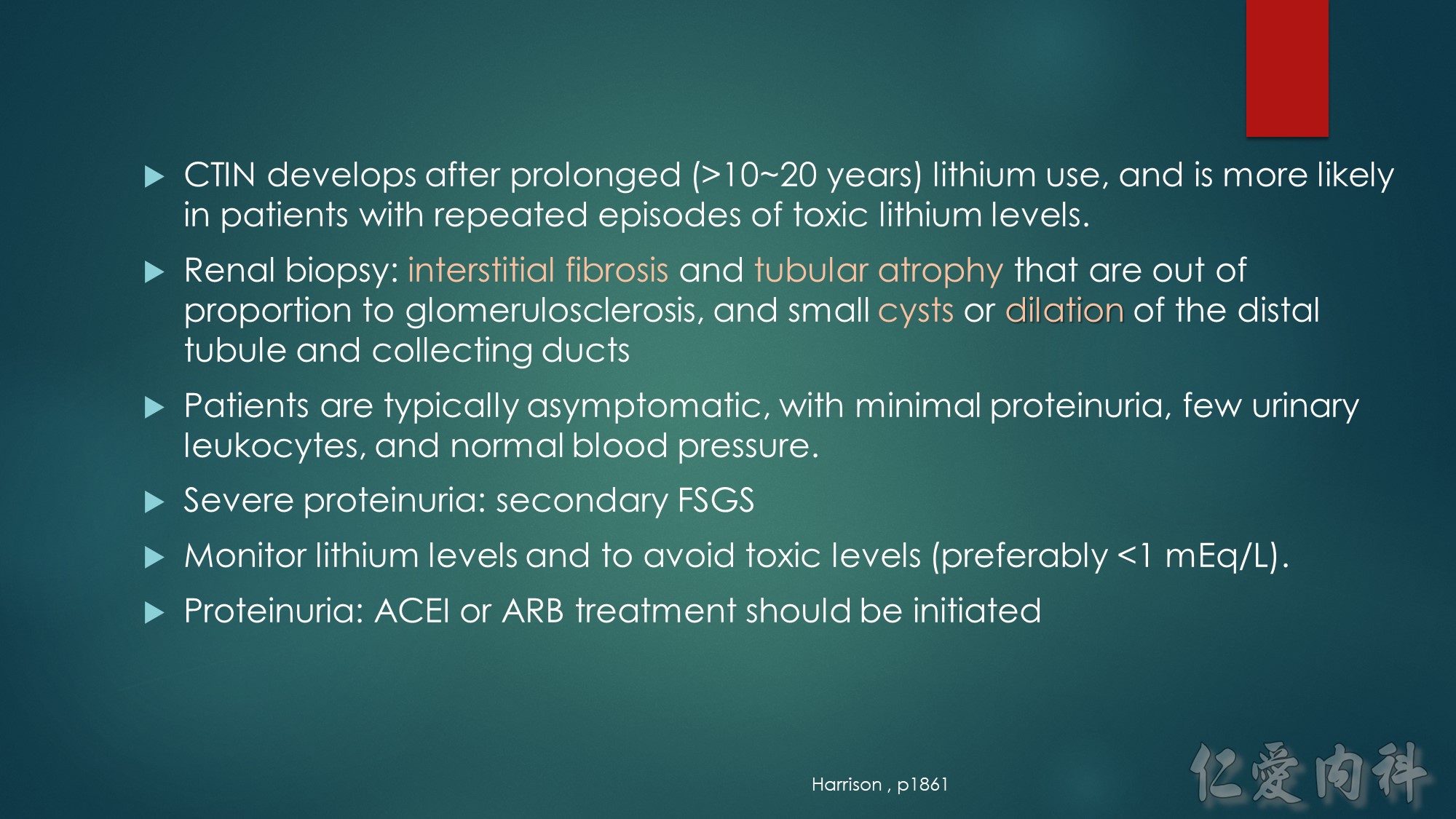
* Lithium約要吃到10-20年以上才會有上述的破壞產生,做renal biopsy會看到interstitial fibrosis、tubular atrophy、small cyst or dilation of distal tubule and collecting ducts.
* 臨床上通常沒什麼症狀,一點點proteinuria、WBC且血壓正常
- 使用lithium要monitor濃度,應小於1 mEq/L
- 若有蛋白尿,應考慮使用ACEI、ARB。
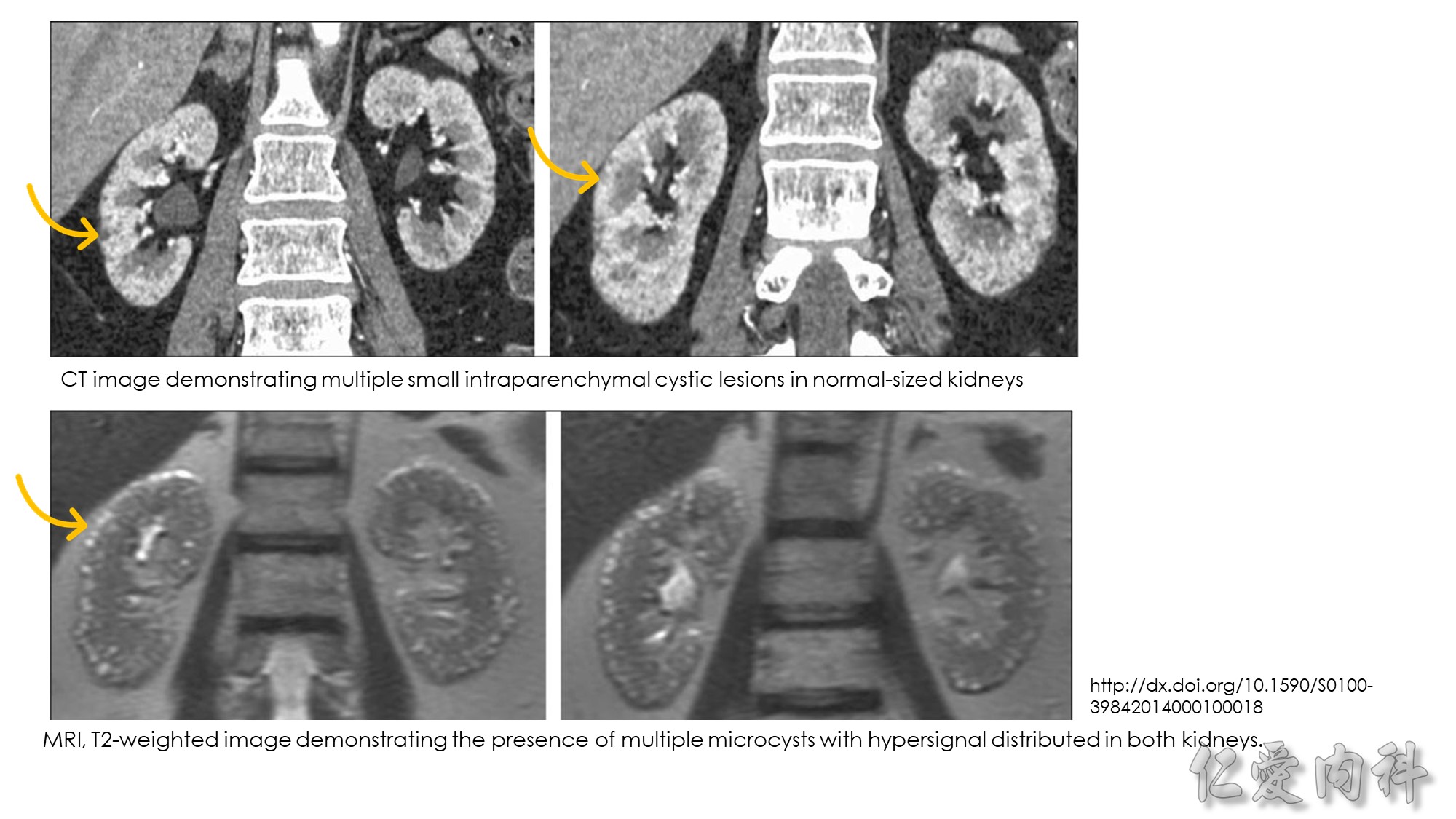
CT上看見小小黑點==> cyst
MRI T2 weighted則是亮白小點點,含水==> cyst
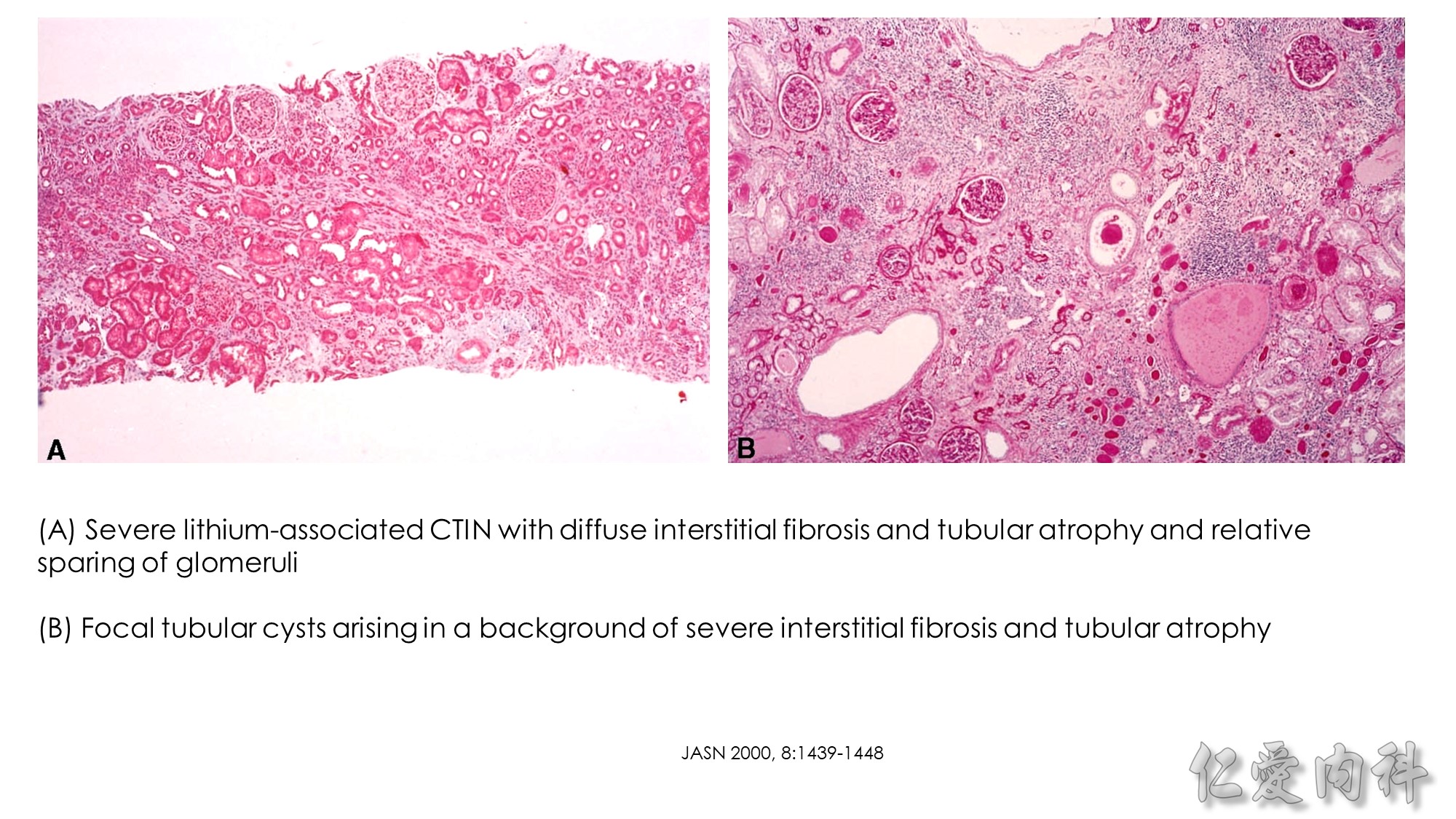
Lithium associated CTIN原則上腎絲球不會被involve,是以腎小管的受損為主,腎小管之間距離會拉大,為chronic interstitial nephritis。
CTI的各種可能cause
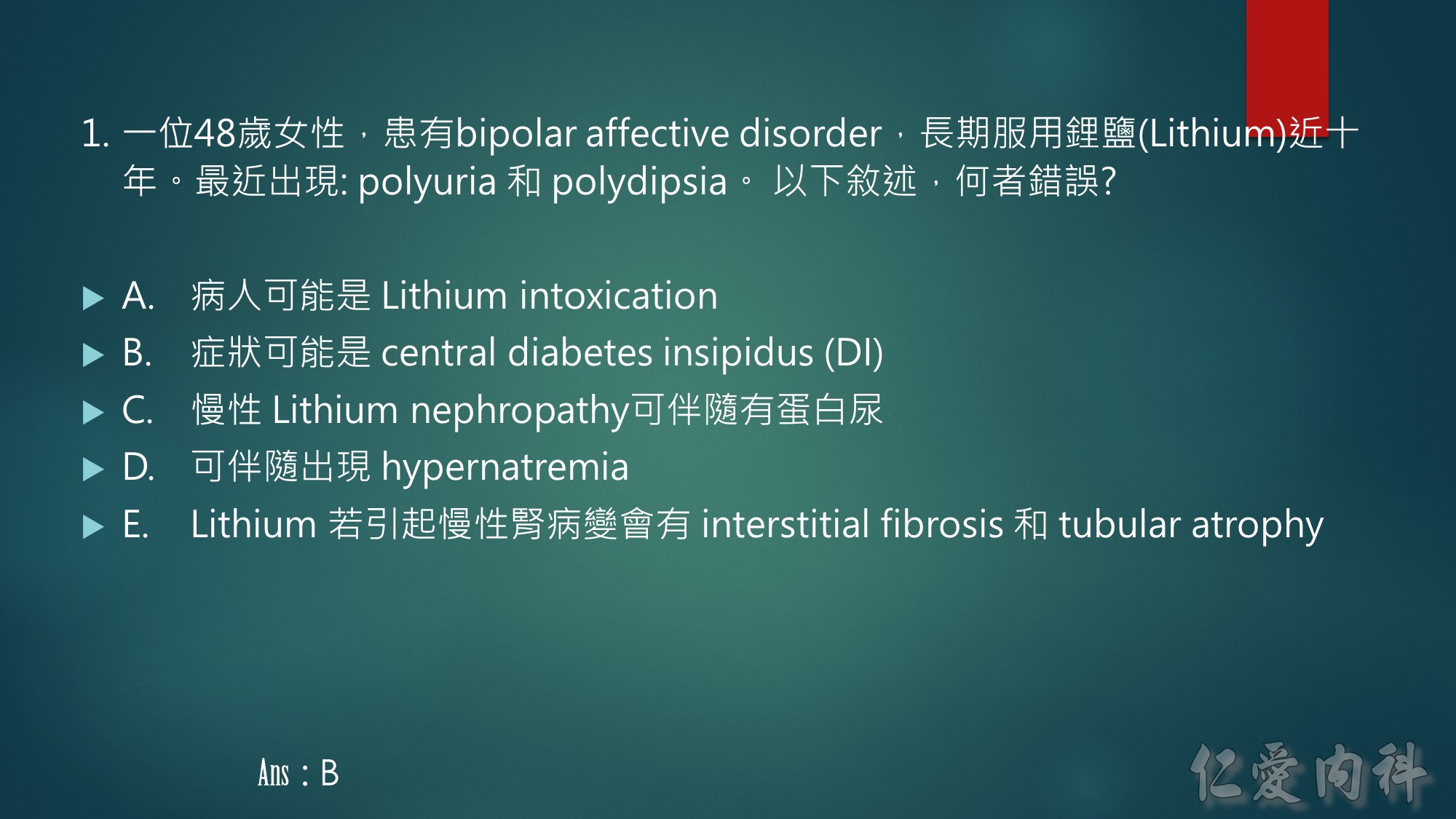
為nephrogenic DI
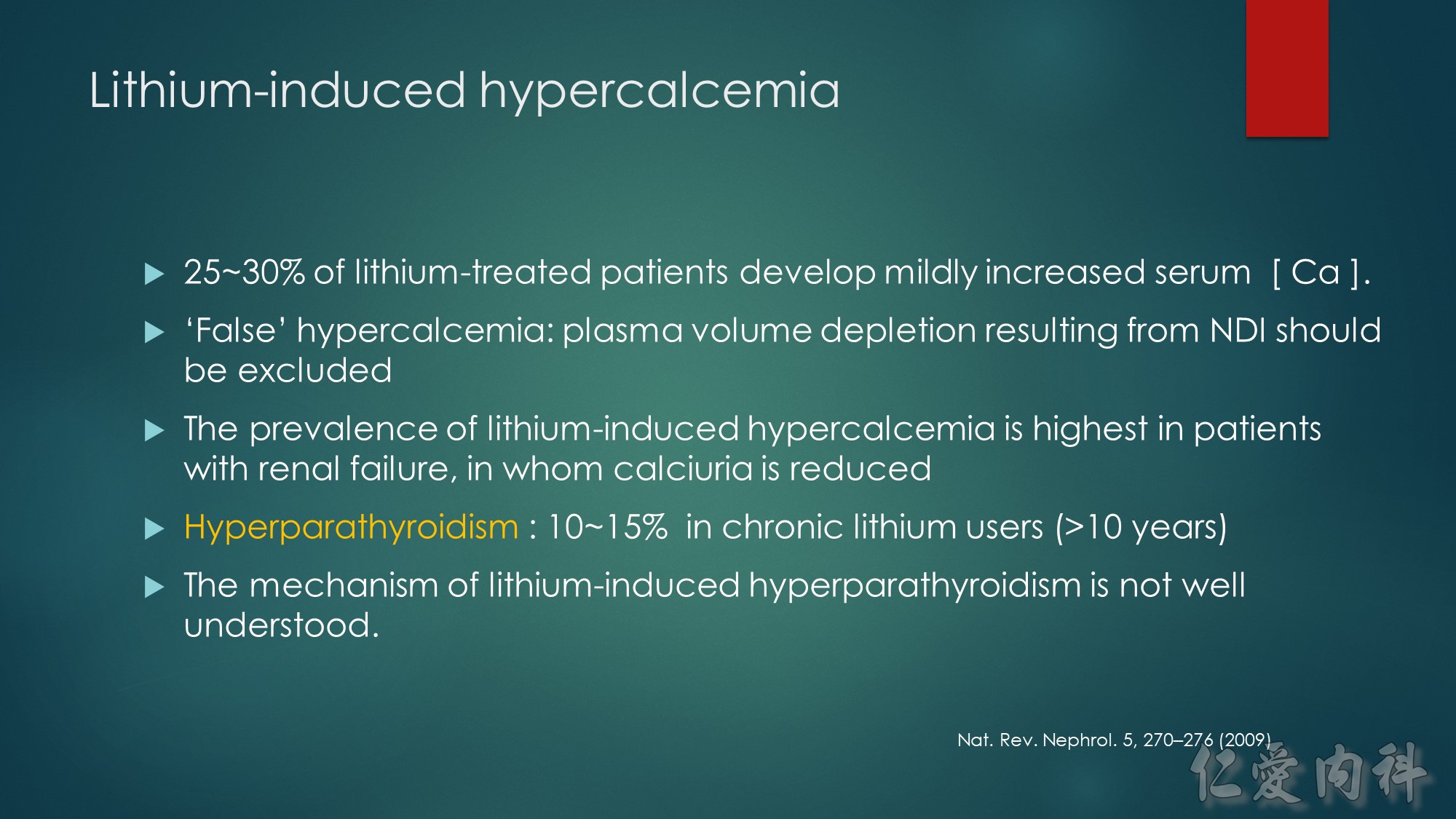
Lithium亦可能造成高血鈣
1.因水流失之後。Pseudo的鈣上升
2.lithium中毒之後不明etiology的hypertparathyroidism

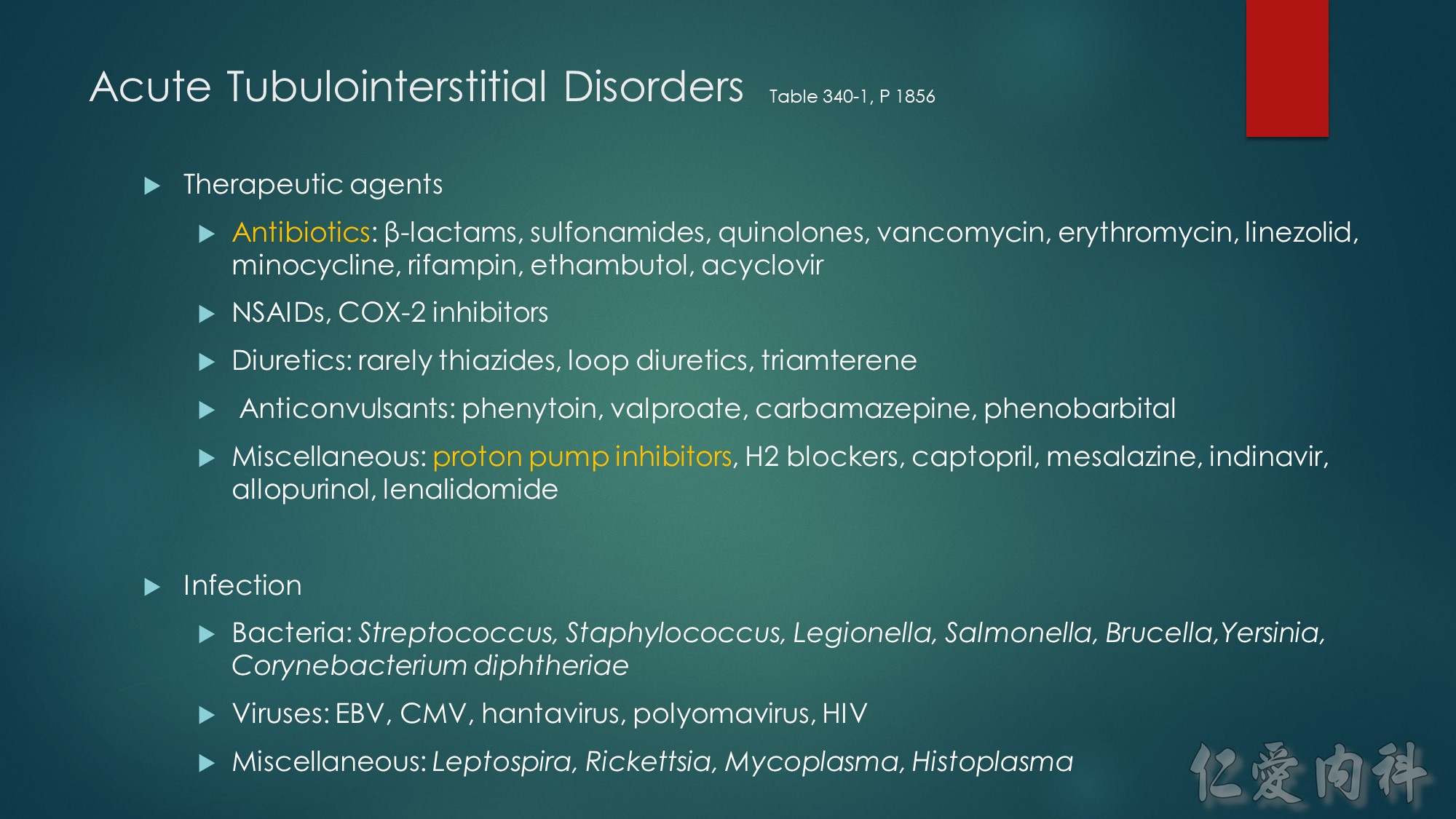
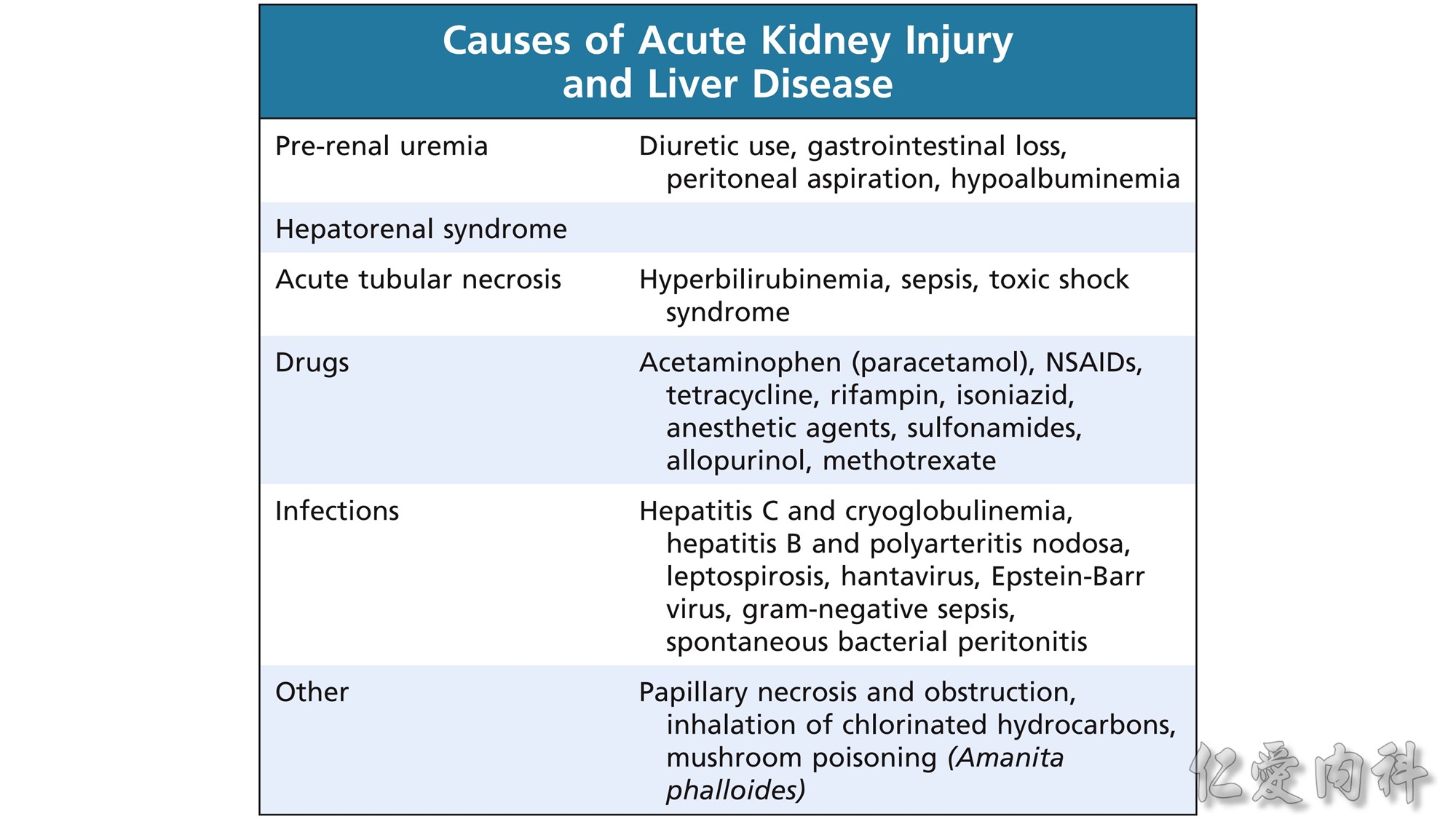
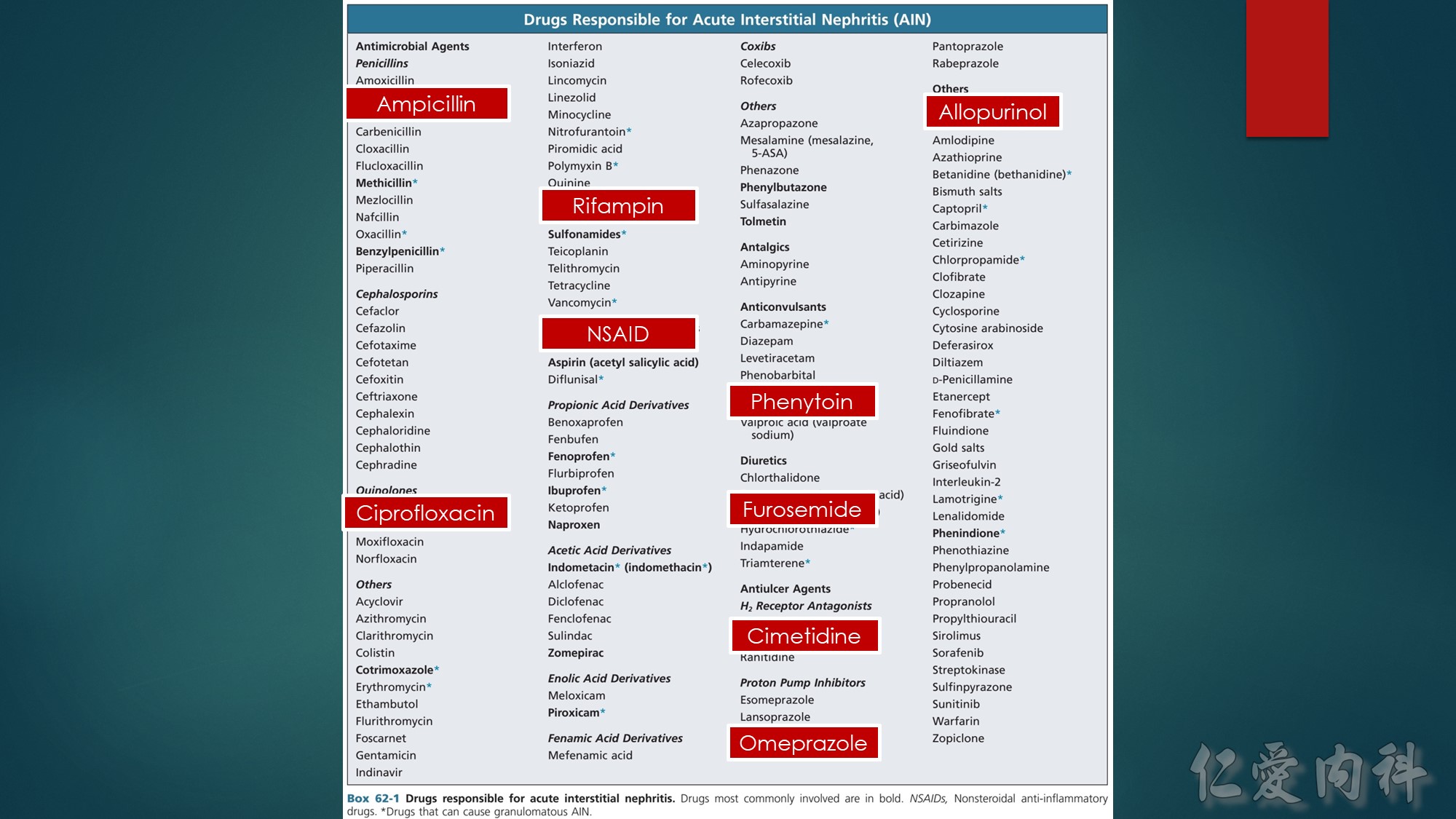
ATIN cause
1.藥物:最常見是抗生素、另外一個不常注意但越來越多case的是PPI造成ATIN。NSAID通常combine minimal change disease
2.infection
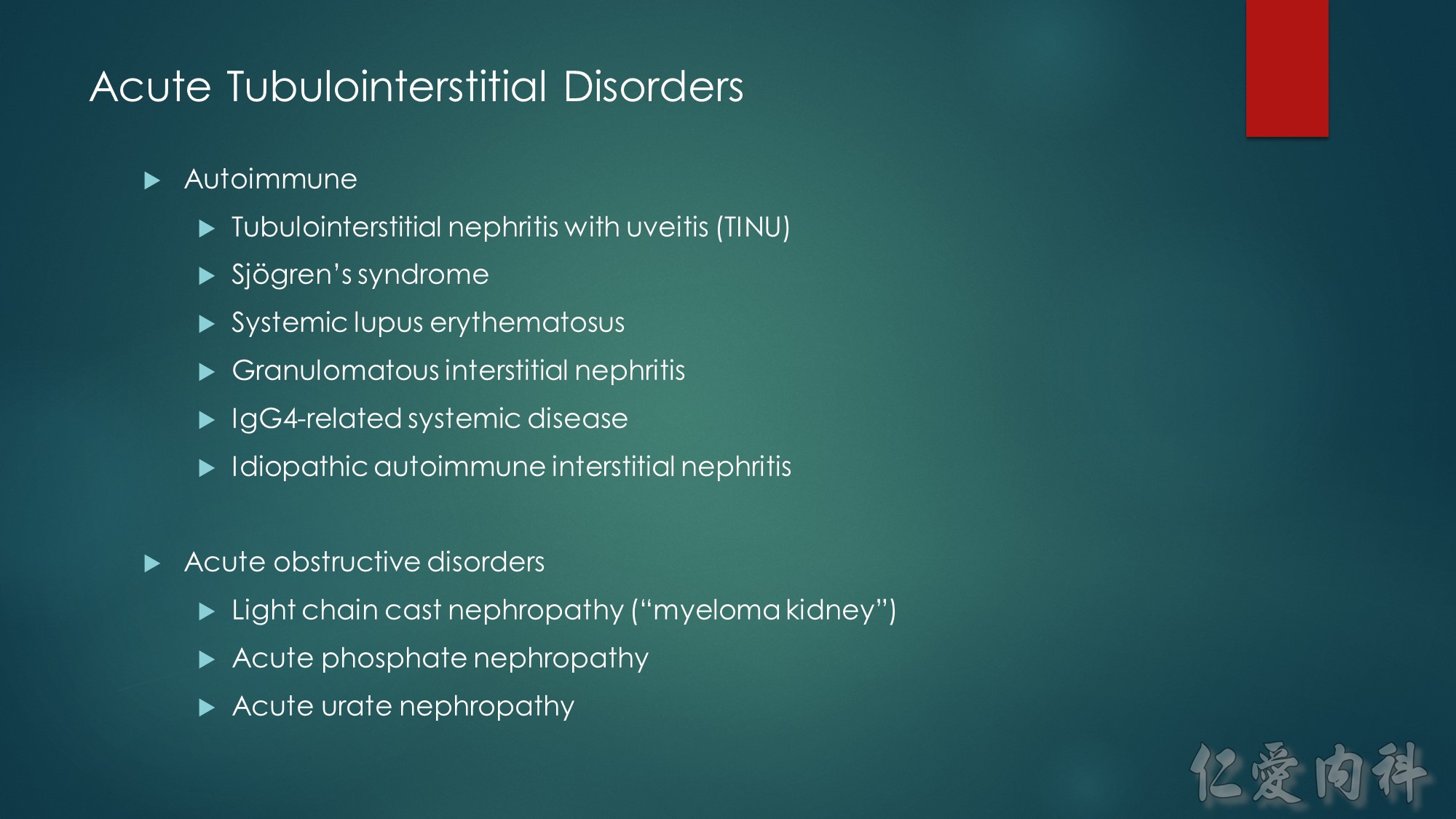
ATIN cause
- autoimmune disorder
- obstructive disorder: MM、尿酸
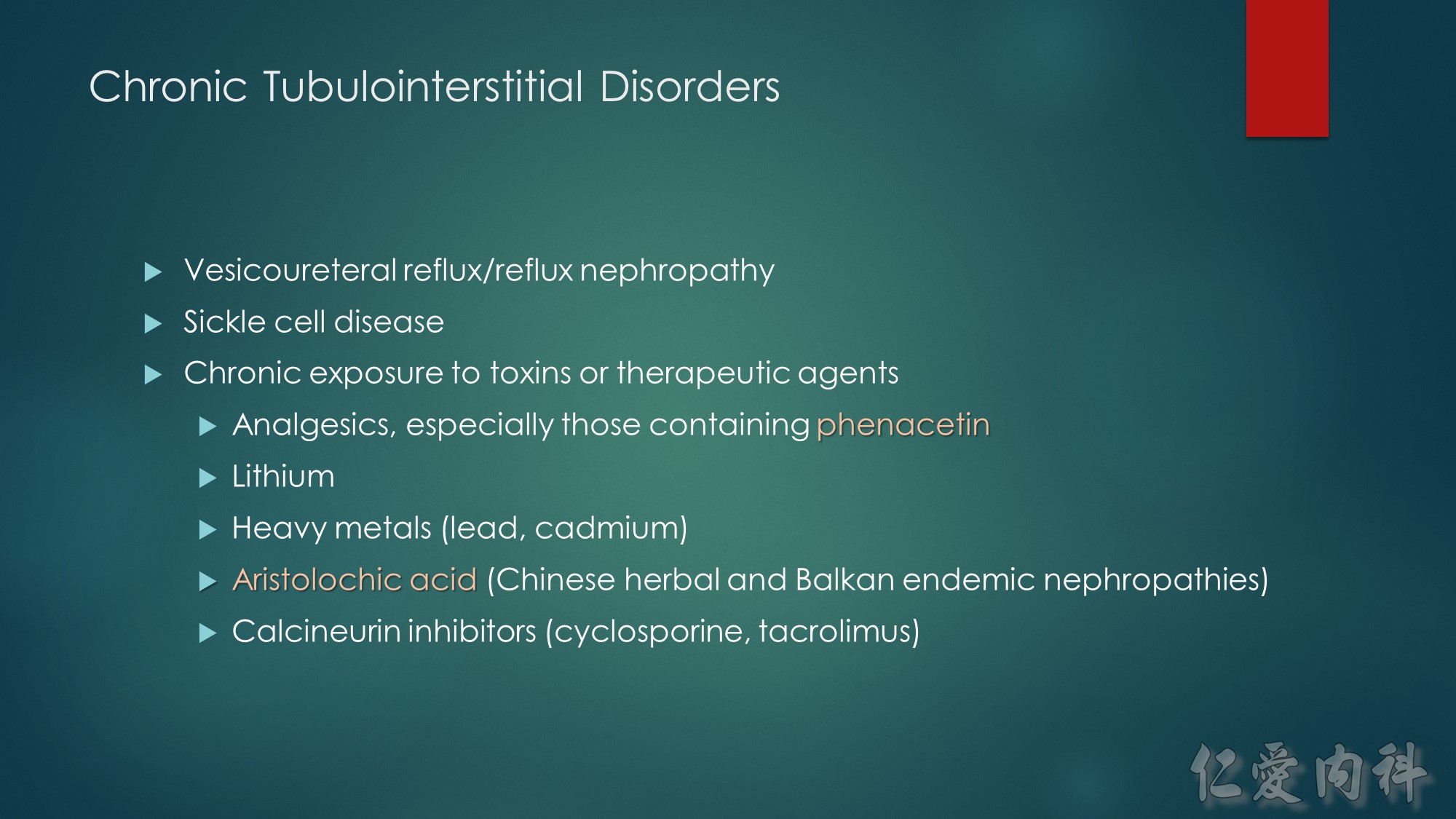
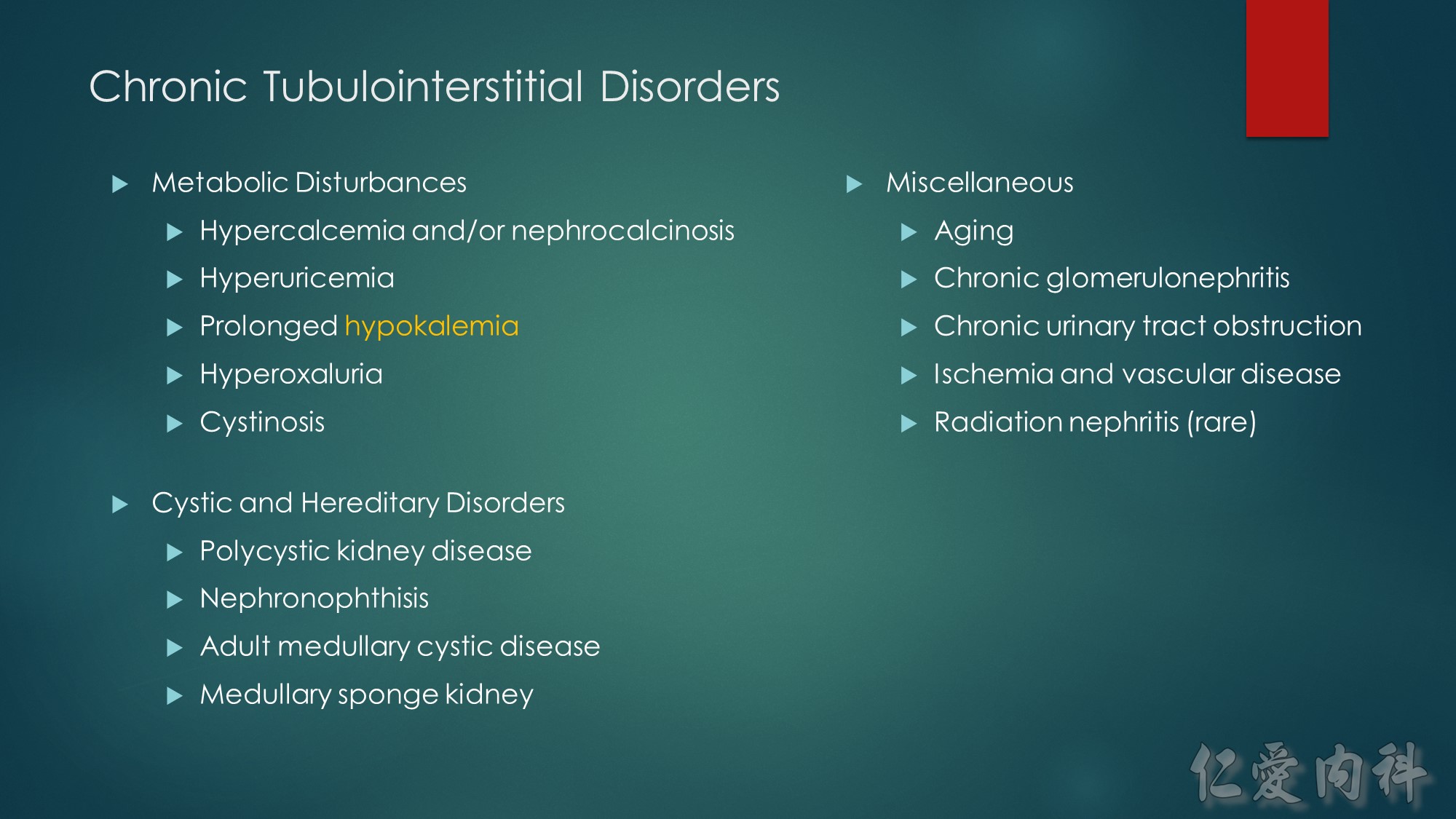
低血鉀、慢性腎絲球腎炎、
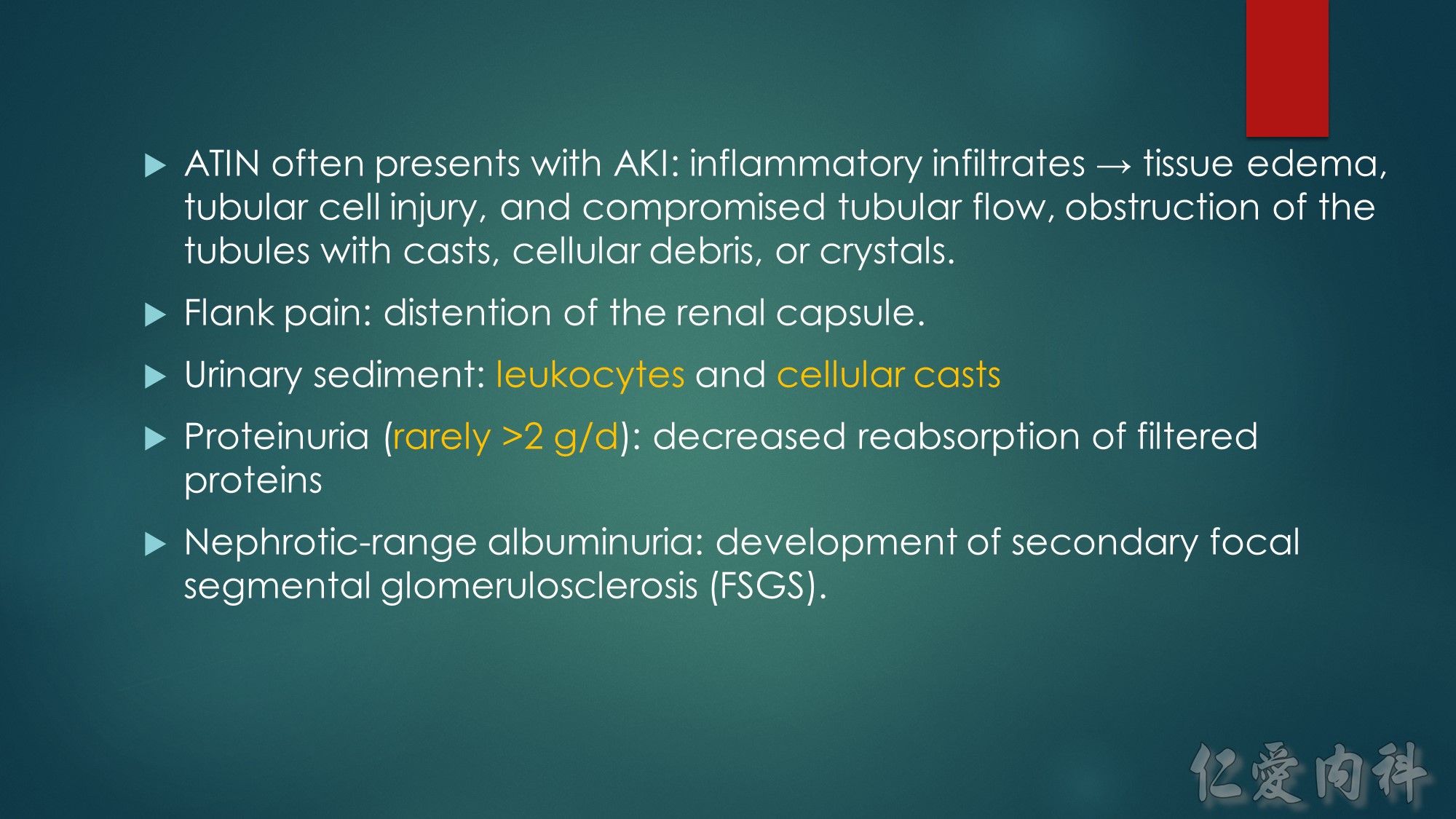
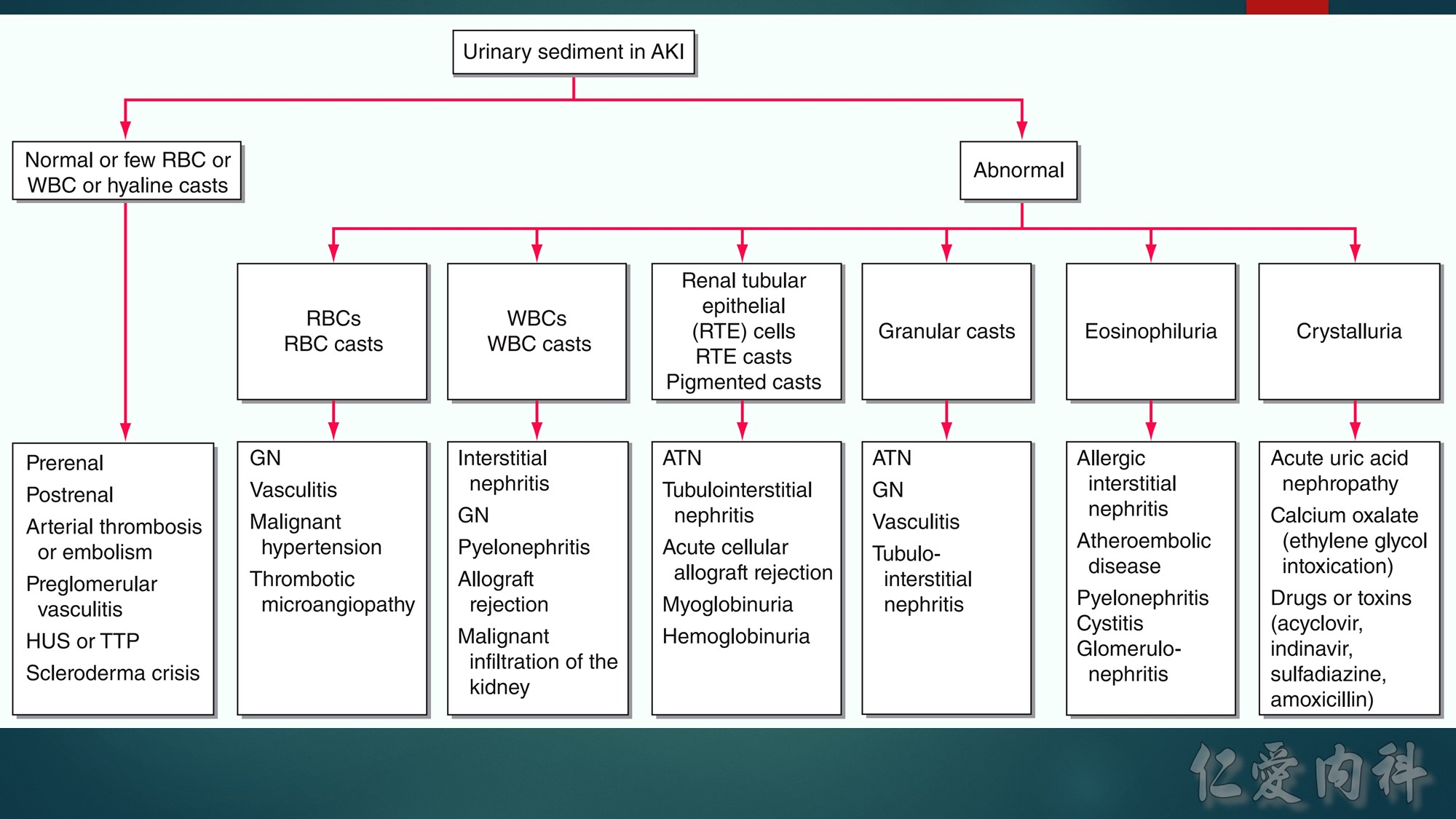
* AKI時,因發炎細胞浸潤、tissue edema造成tubular obstruction、腫脹、拉扯gerota fascia-==> 腰痛
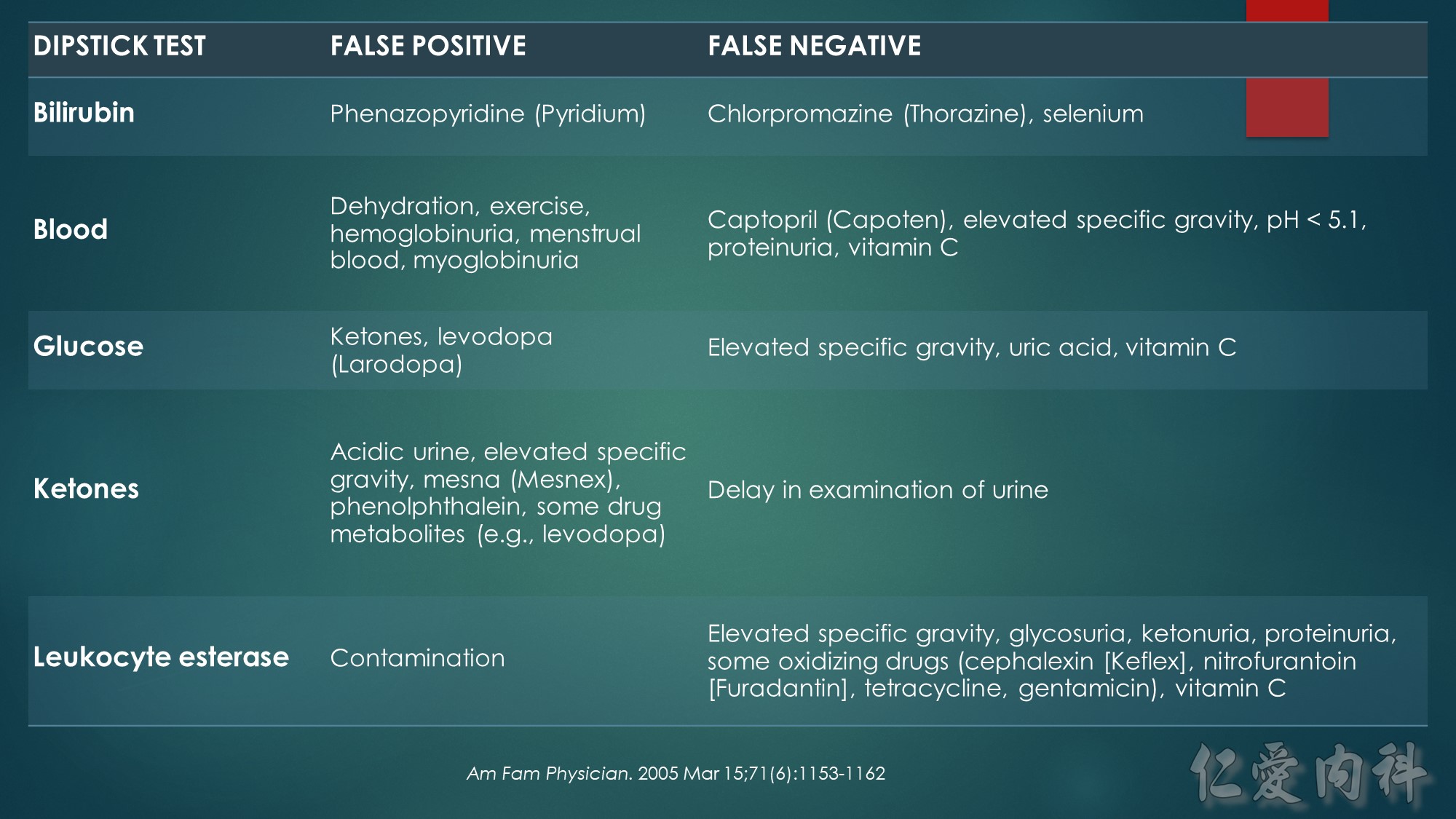
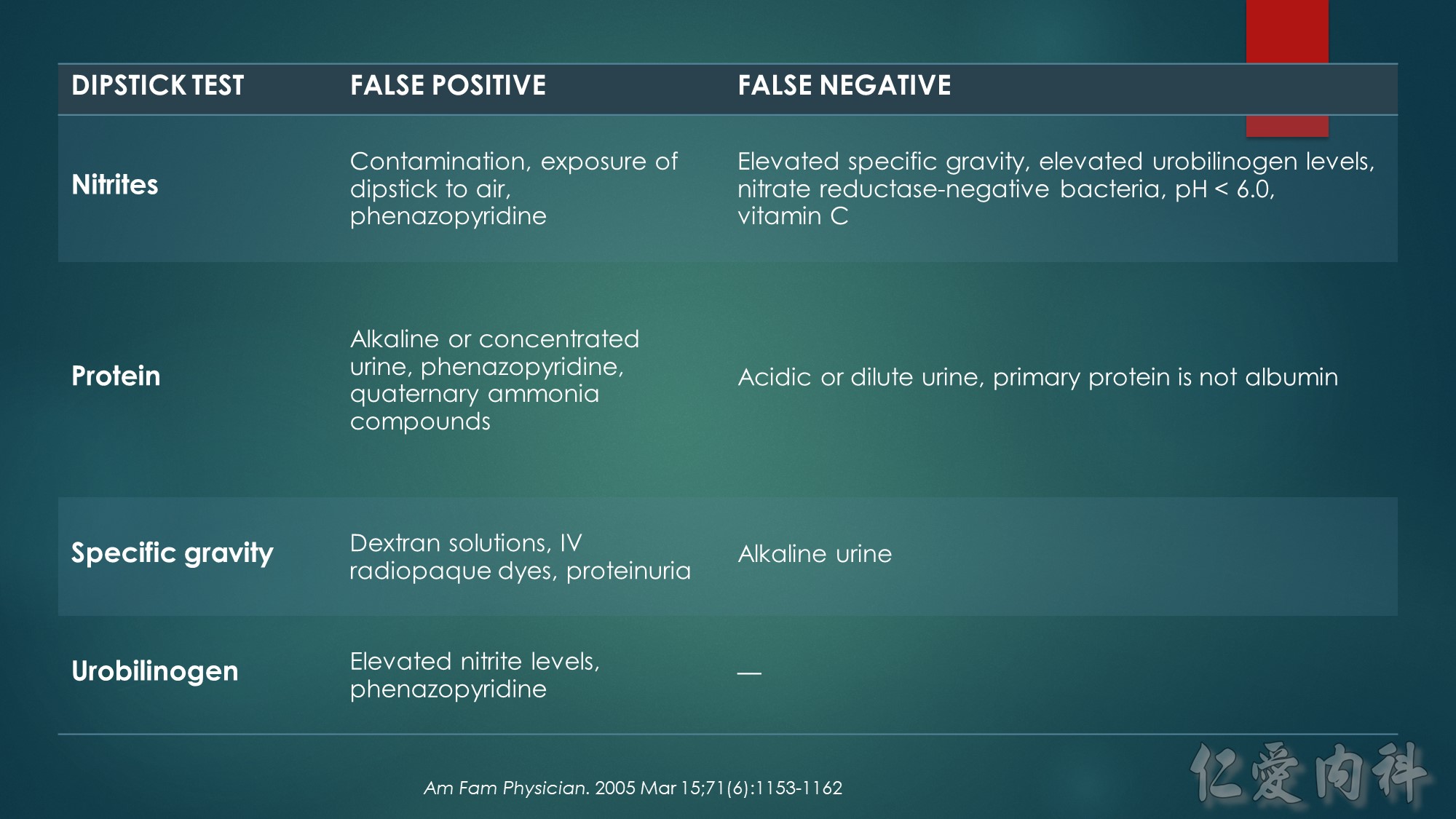
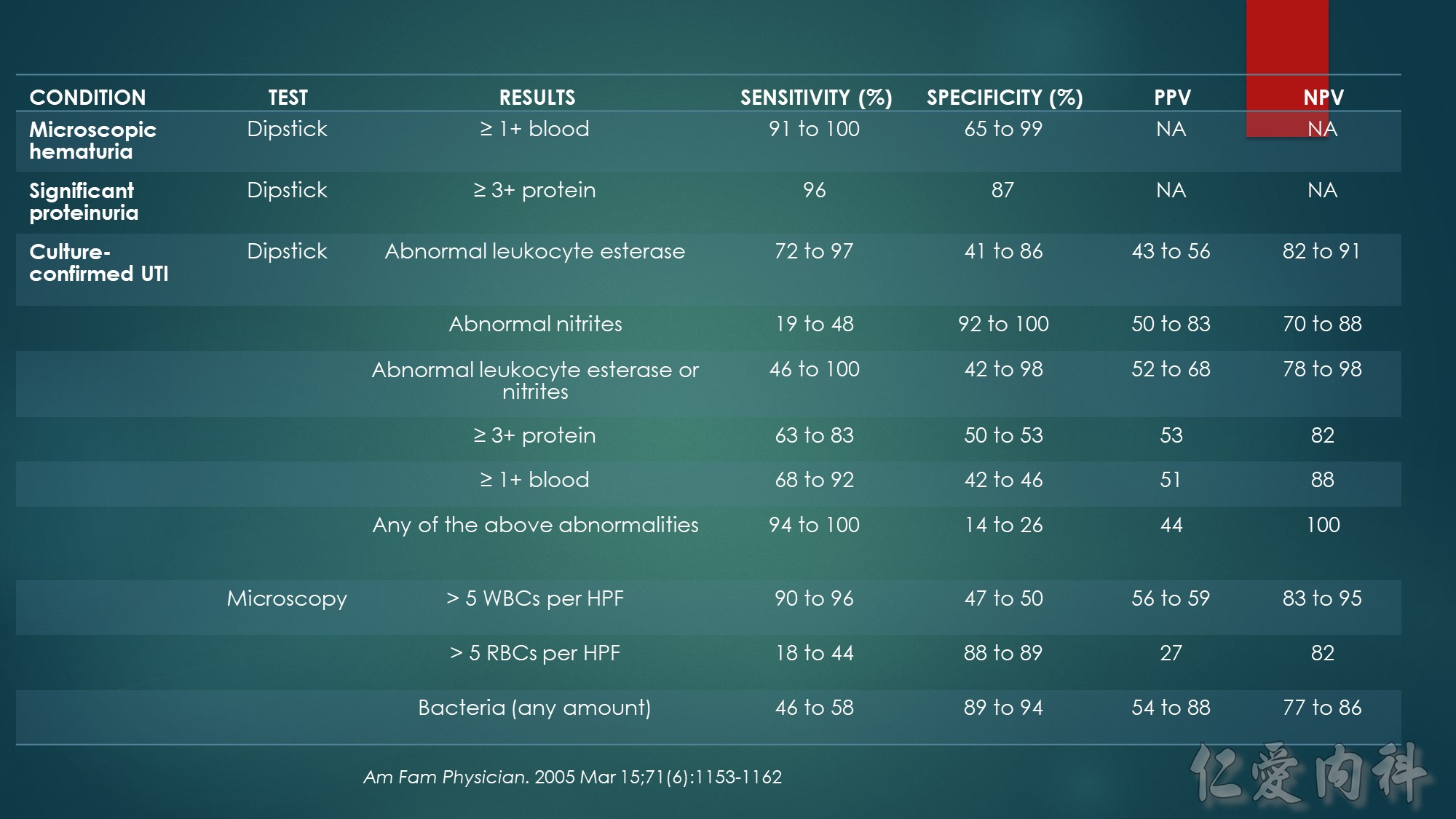
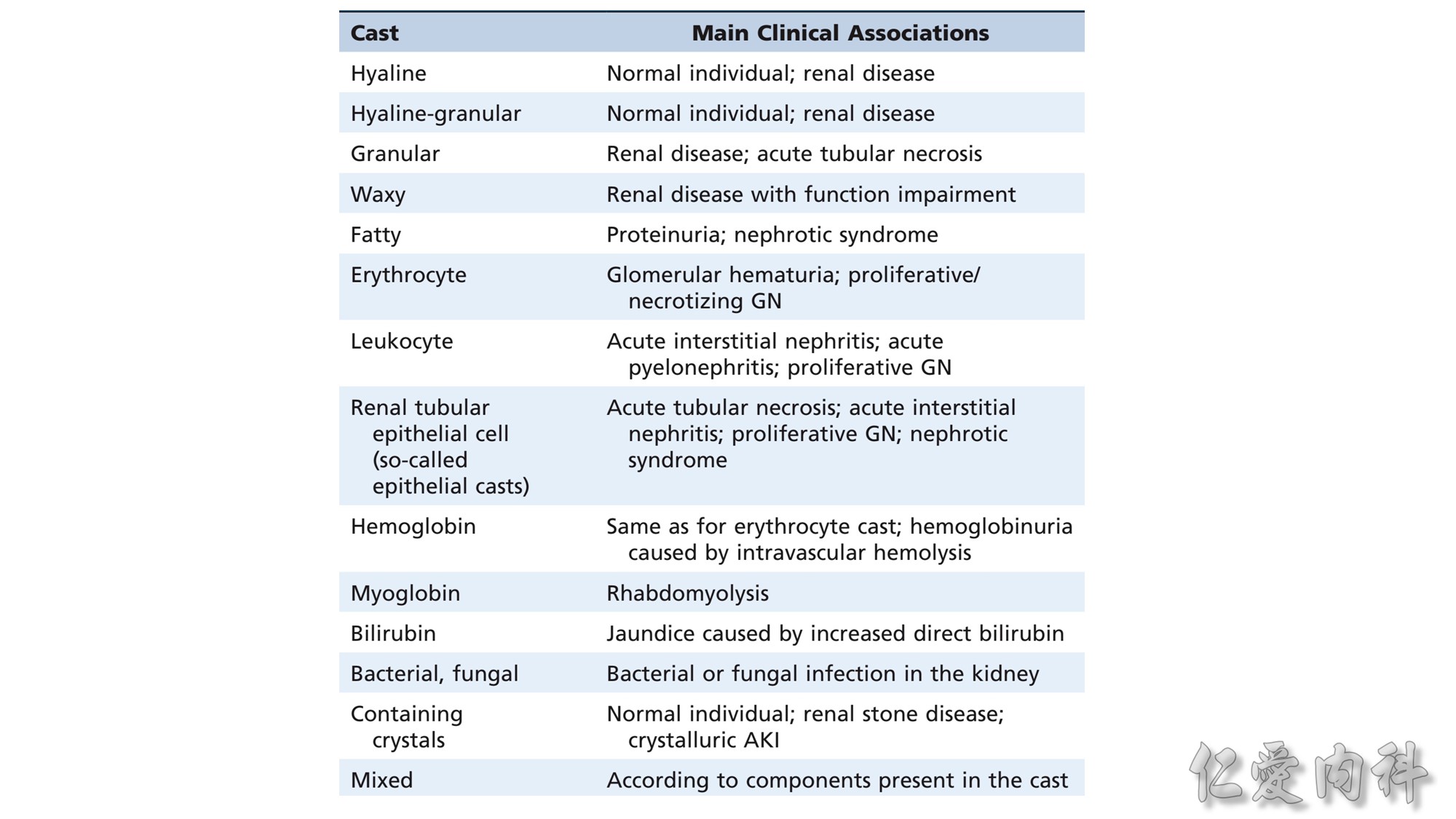
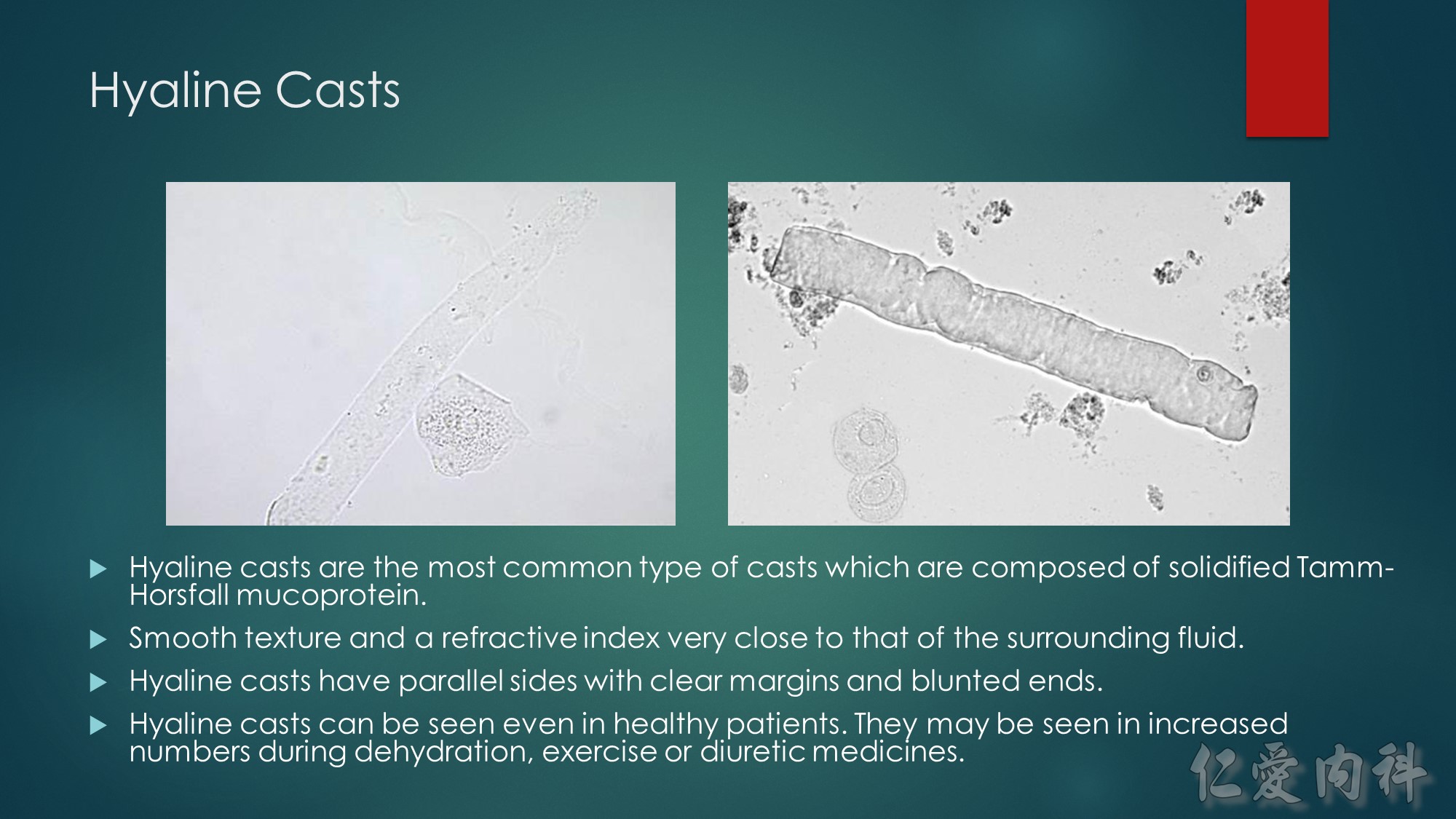
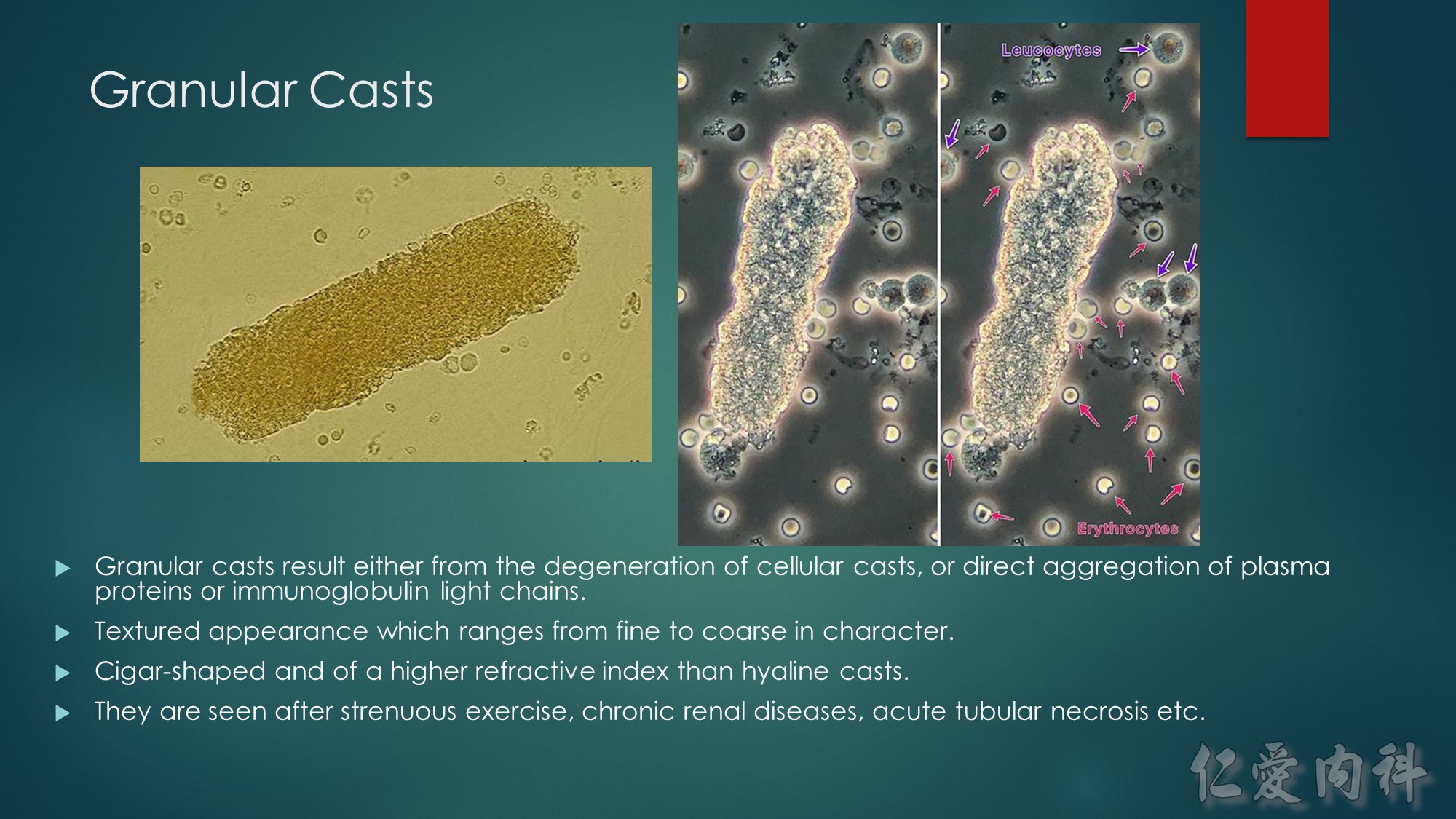
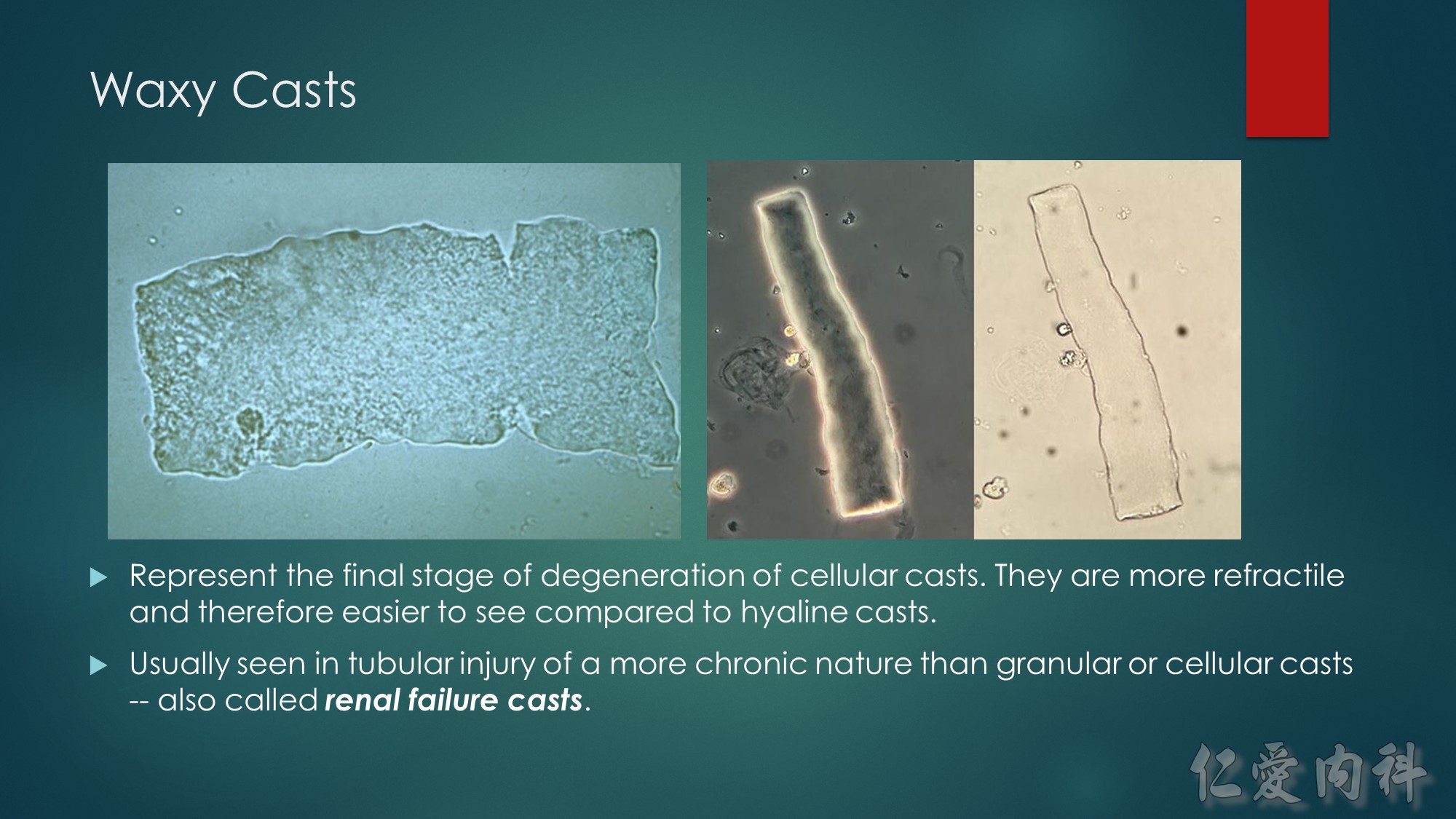
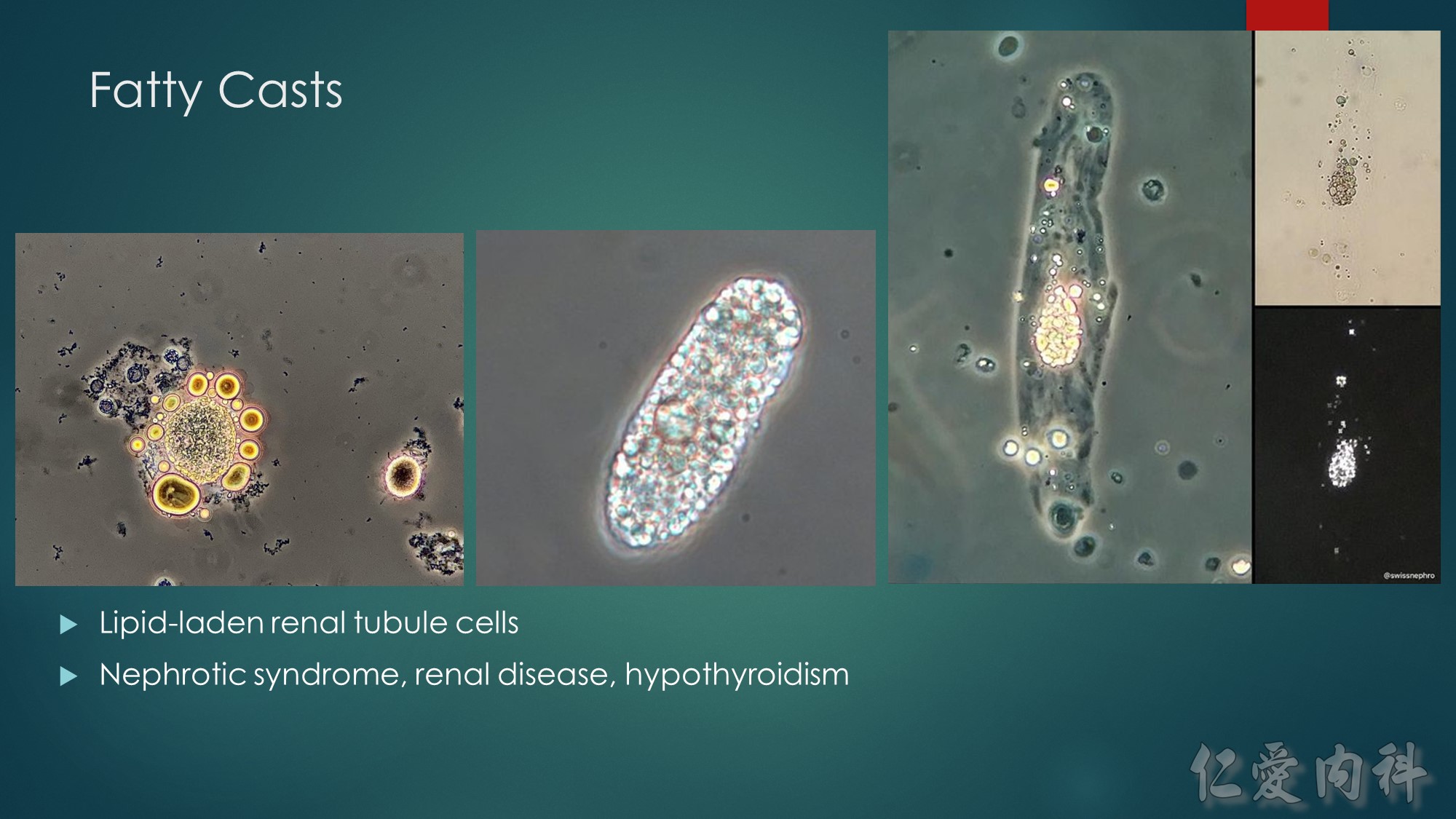
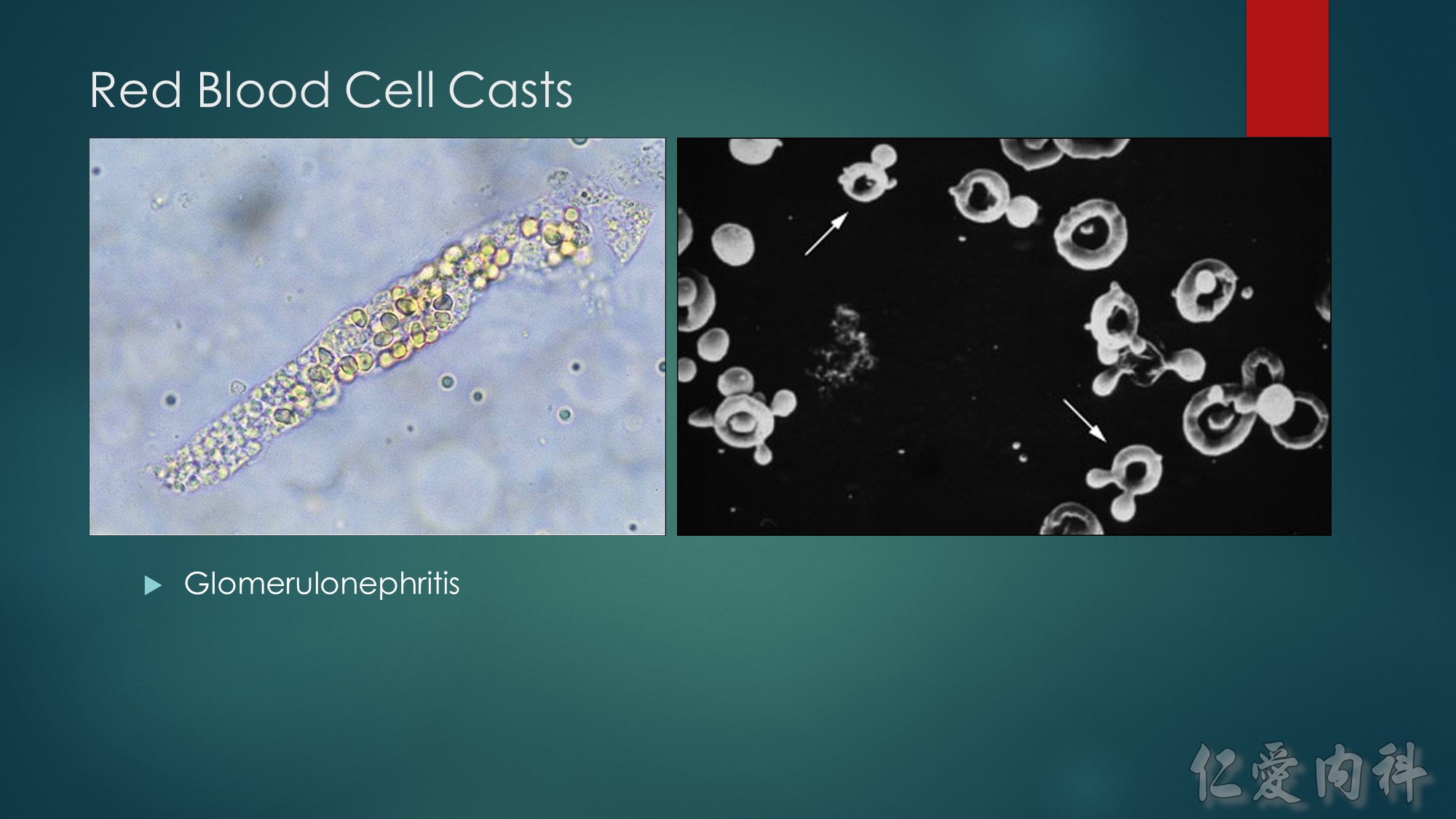
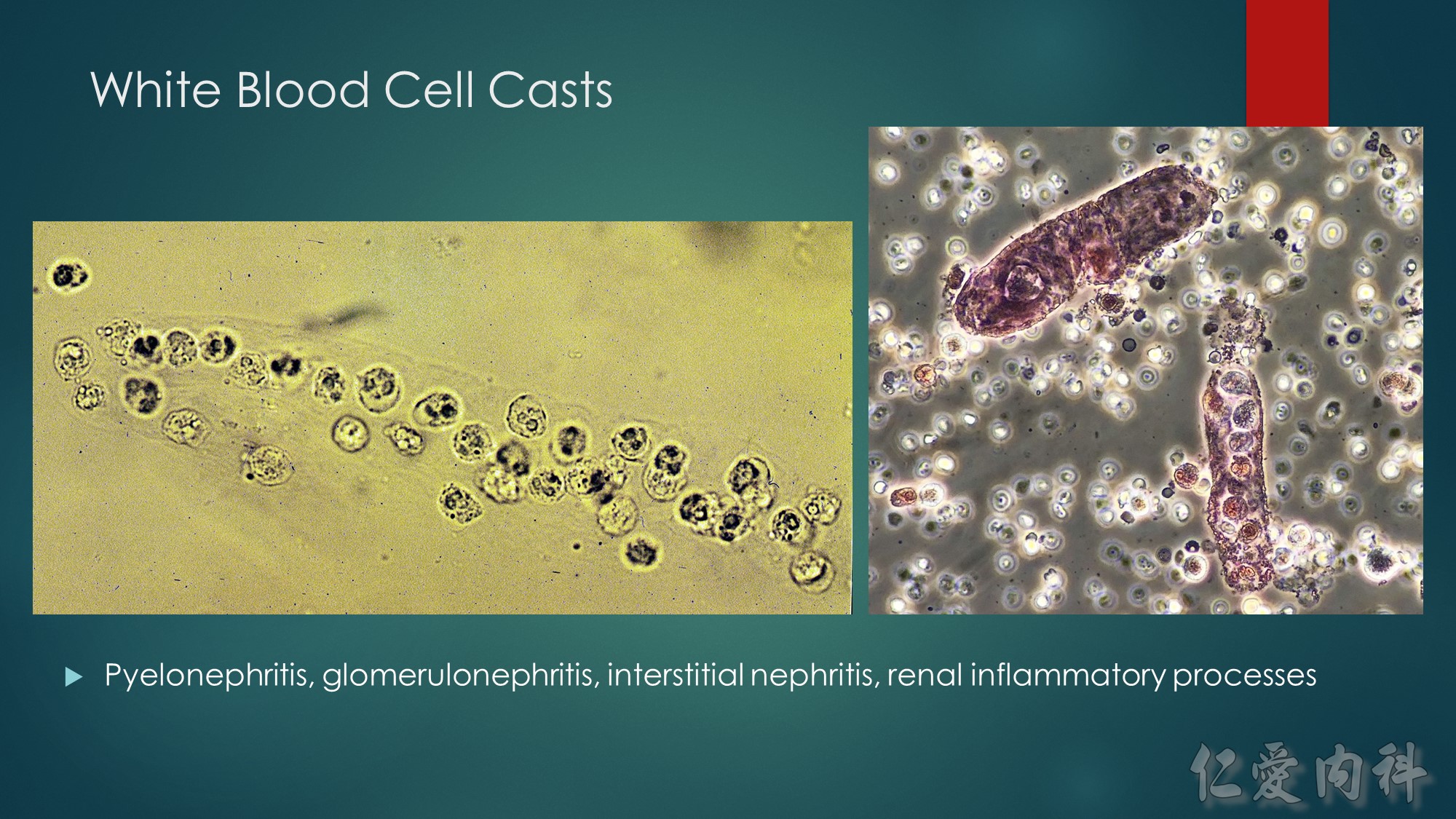
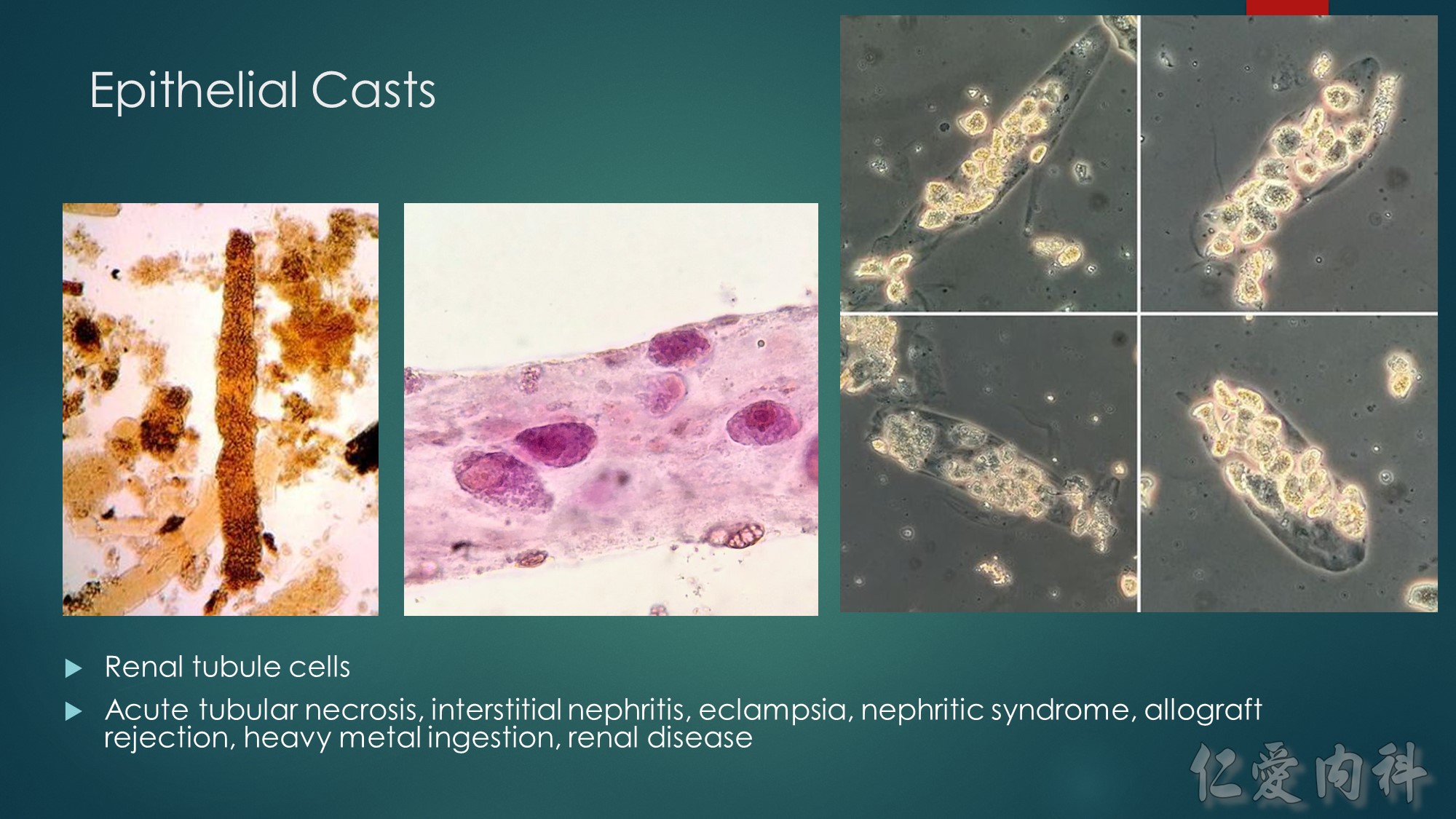
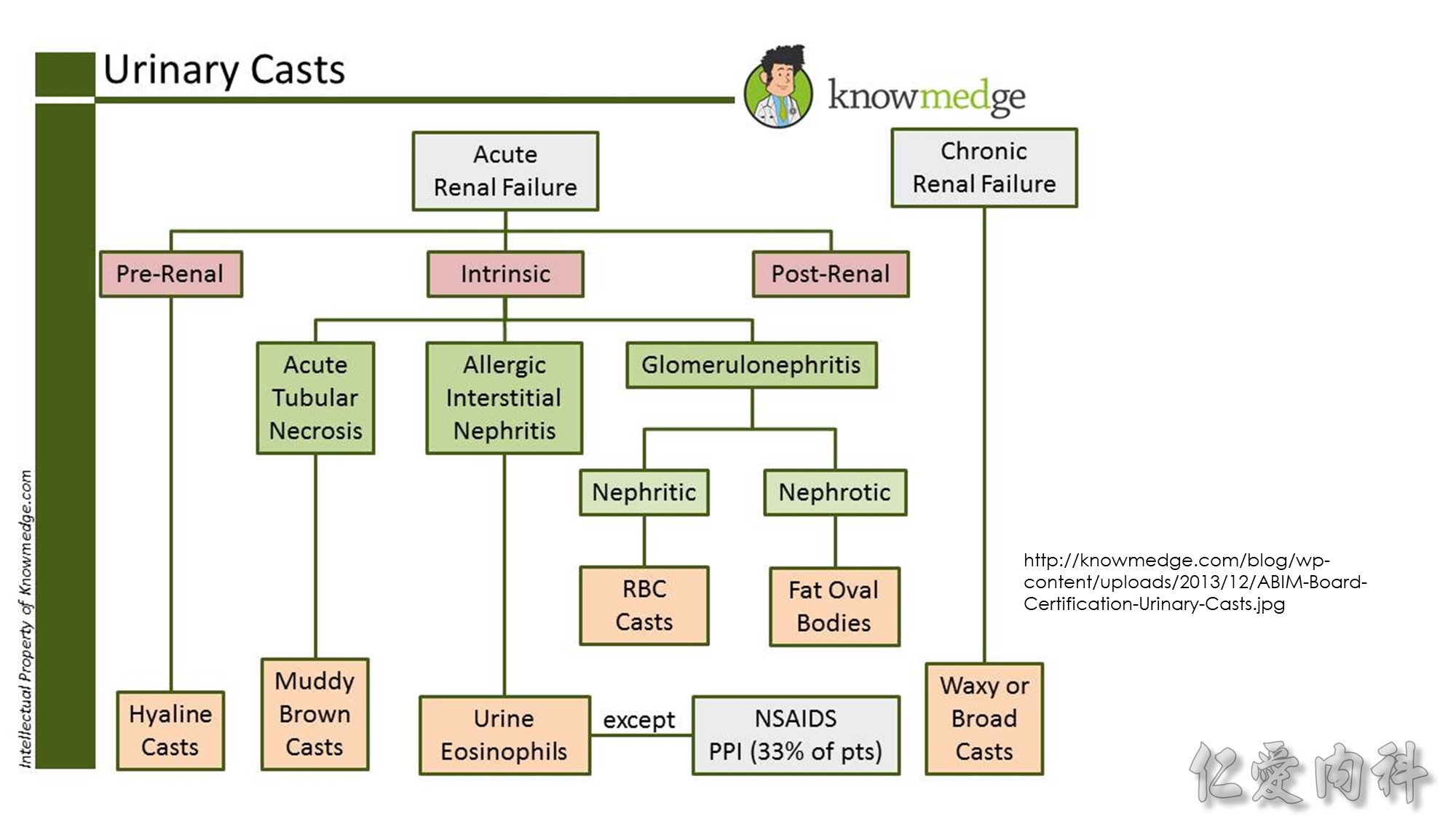
U/A出現leukocyte、tubular cell damage造成cast形成
* Proteinuria的部分,腎絲球腎炎的蛋白質漏出會比較多、腎小管腎炎只是不能回收蛋白質而已,所以腎小管腎炎的蛋白尿會較輕微(subnephrotic range<3 g/d)。
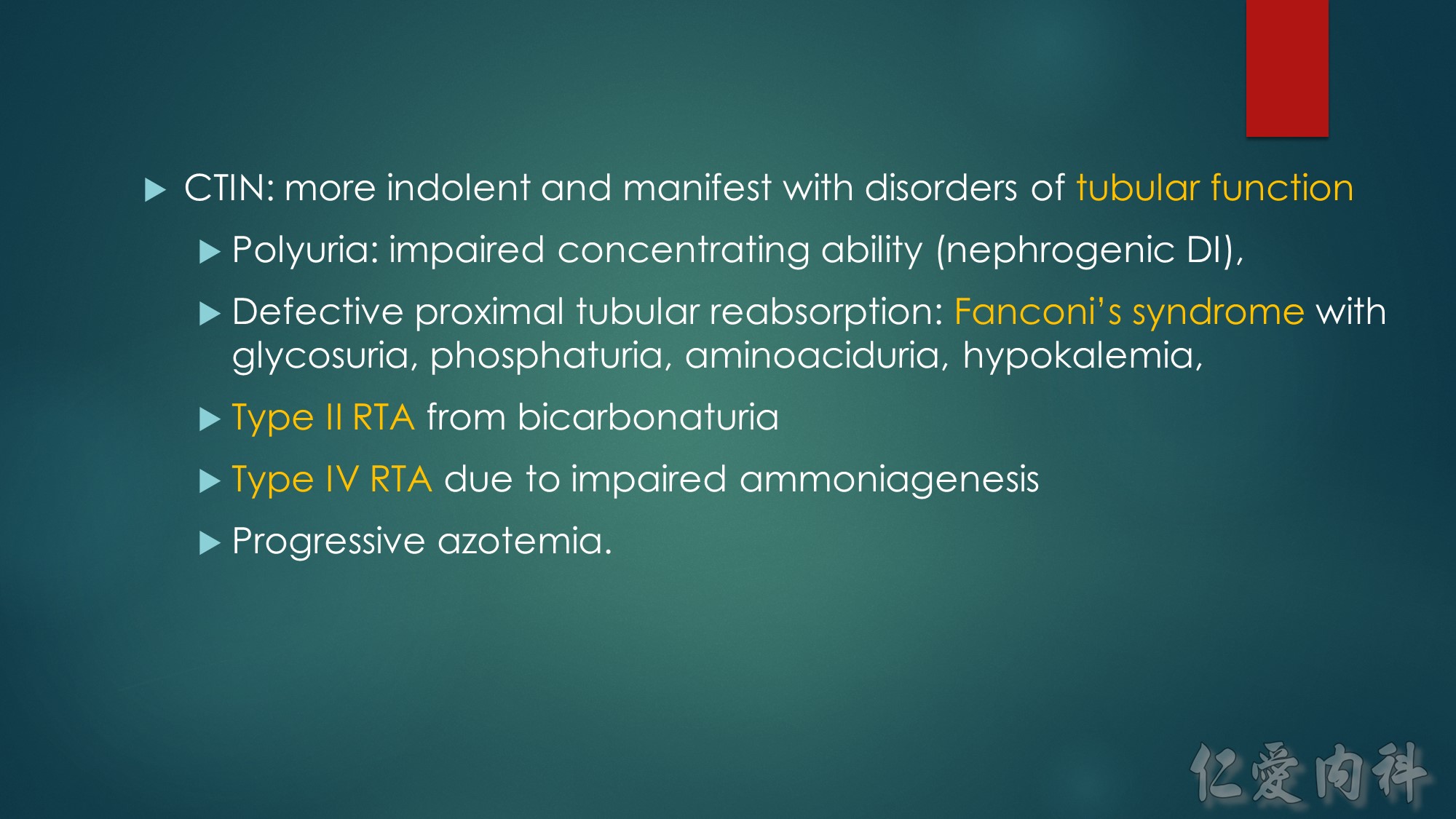
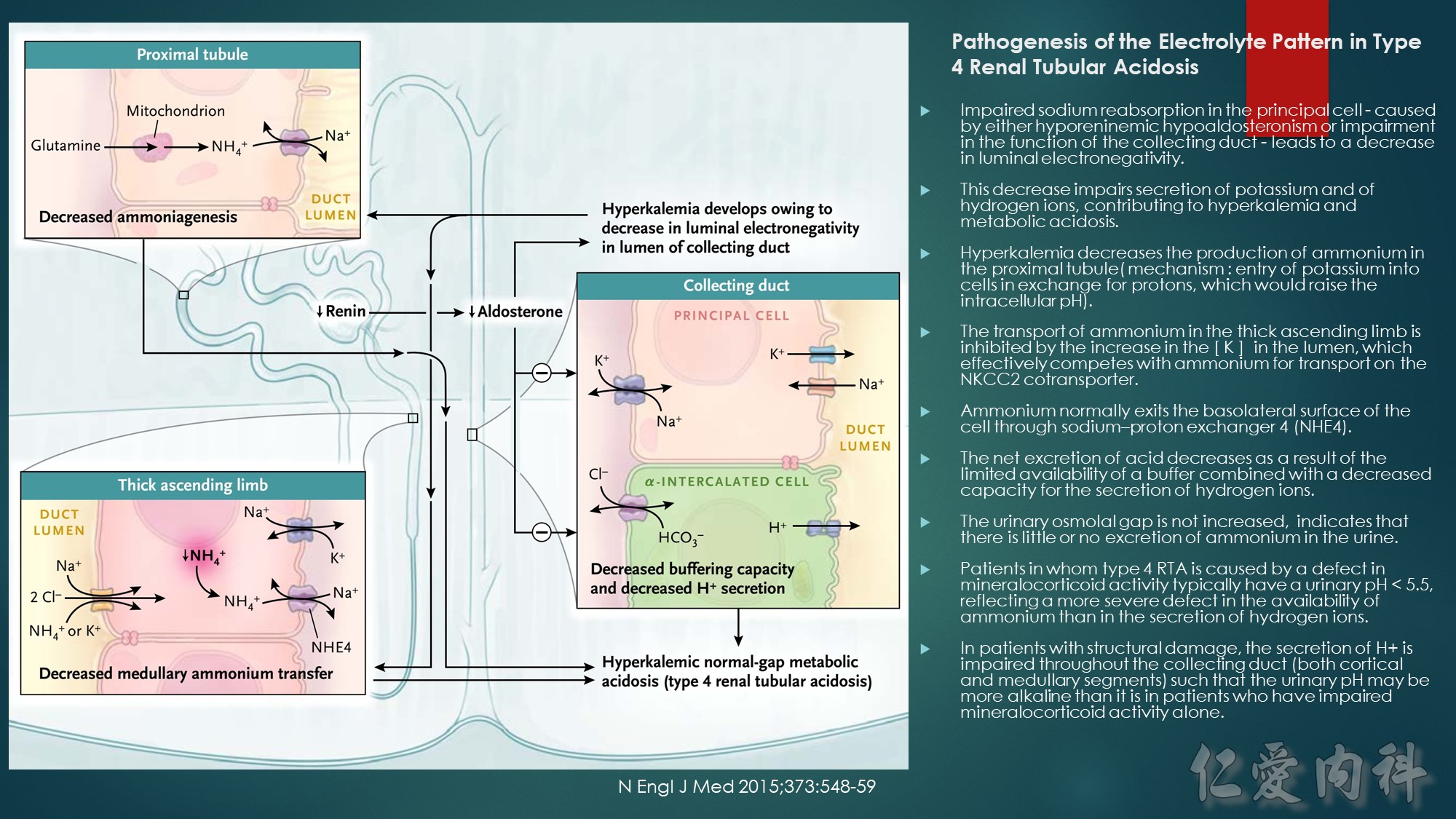
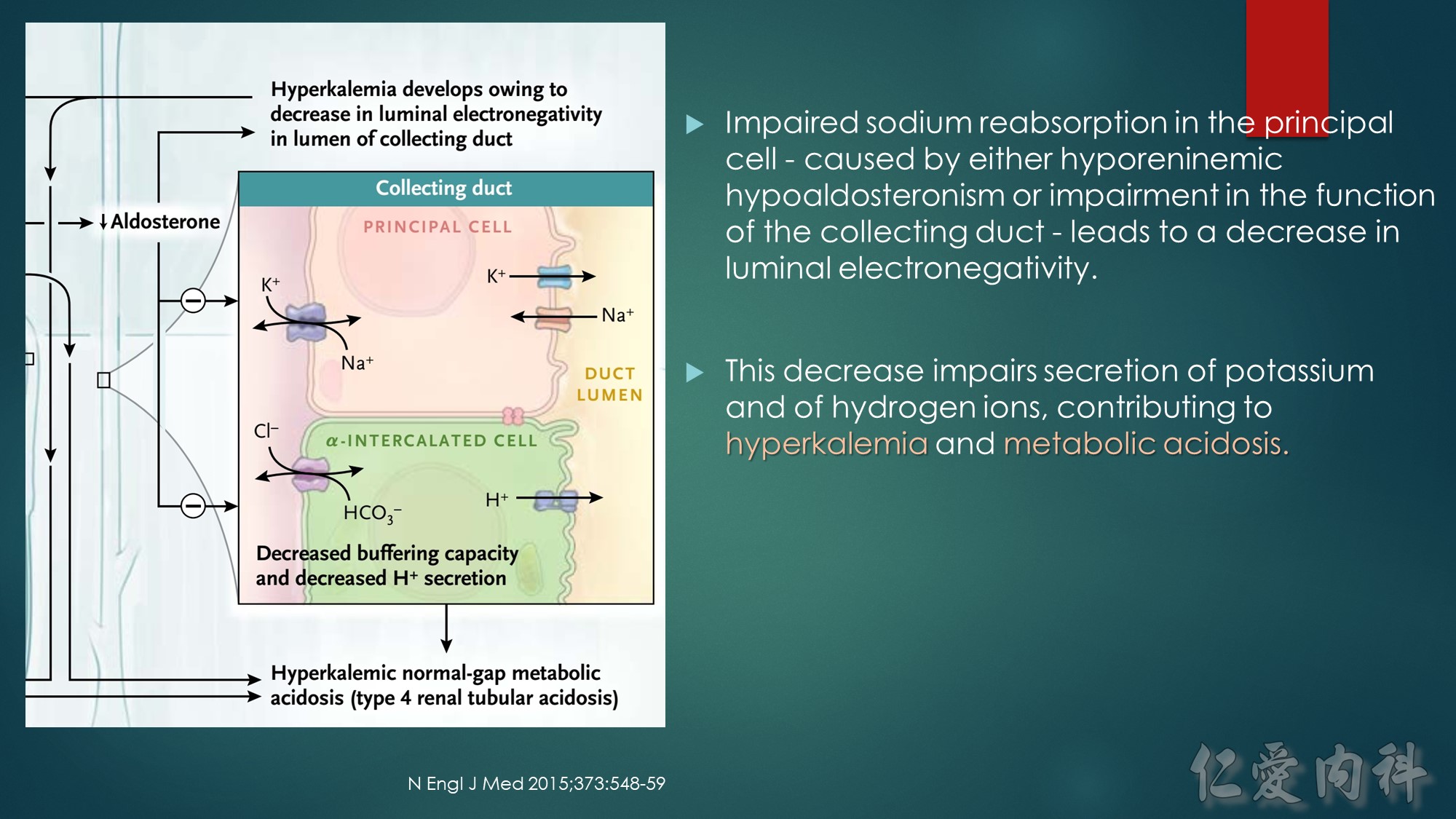
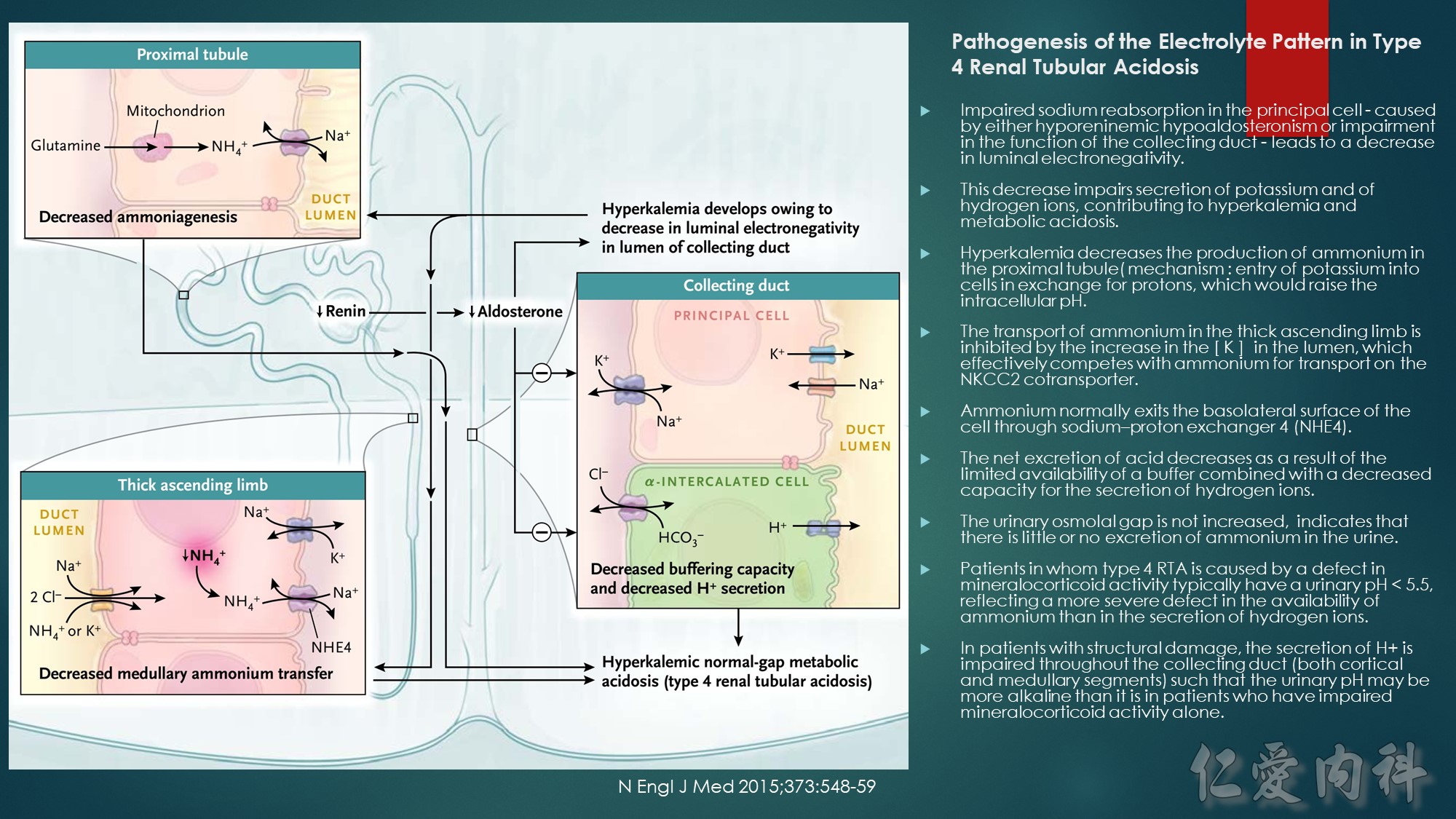
DM p’t 通常renin、aldosterone 都低。
– aldosterone低,Na吸不進來、K排不出去、H也排不出去→高血鉀、代謝酸
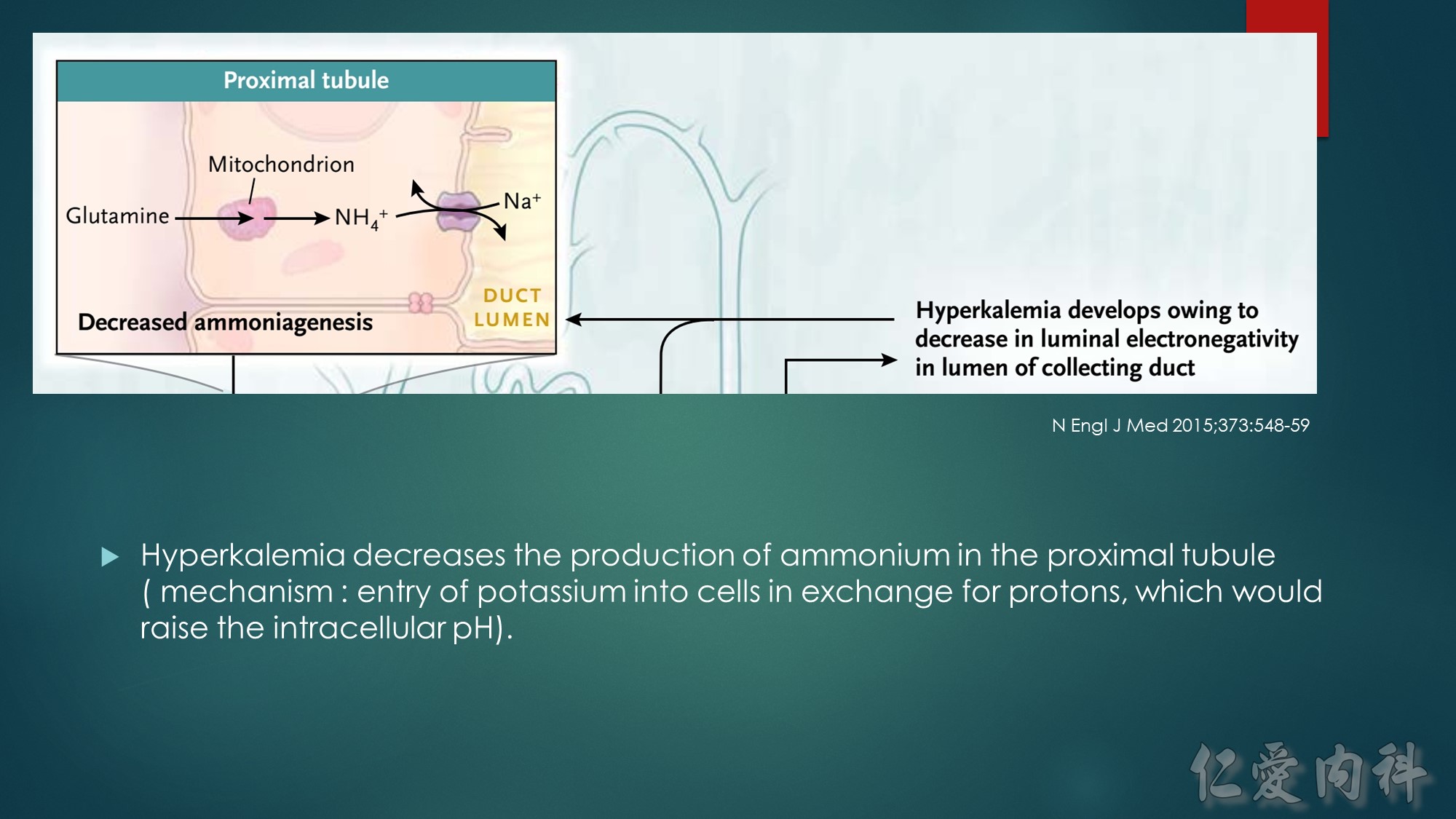
高血鉀==> 鉀進入細胞內會把H擠出細胞,造成胞內alkalosis,alkalosis的環境會抑制glutamine變成NH4(ammoniagenesis)。
NH4做為一個buffer,可與H結合排出,因此impaired ammoniagenesis會進一步造成代謝酸。
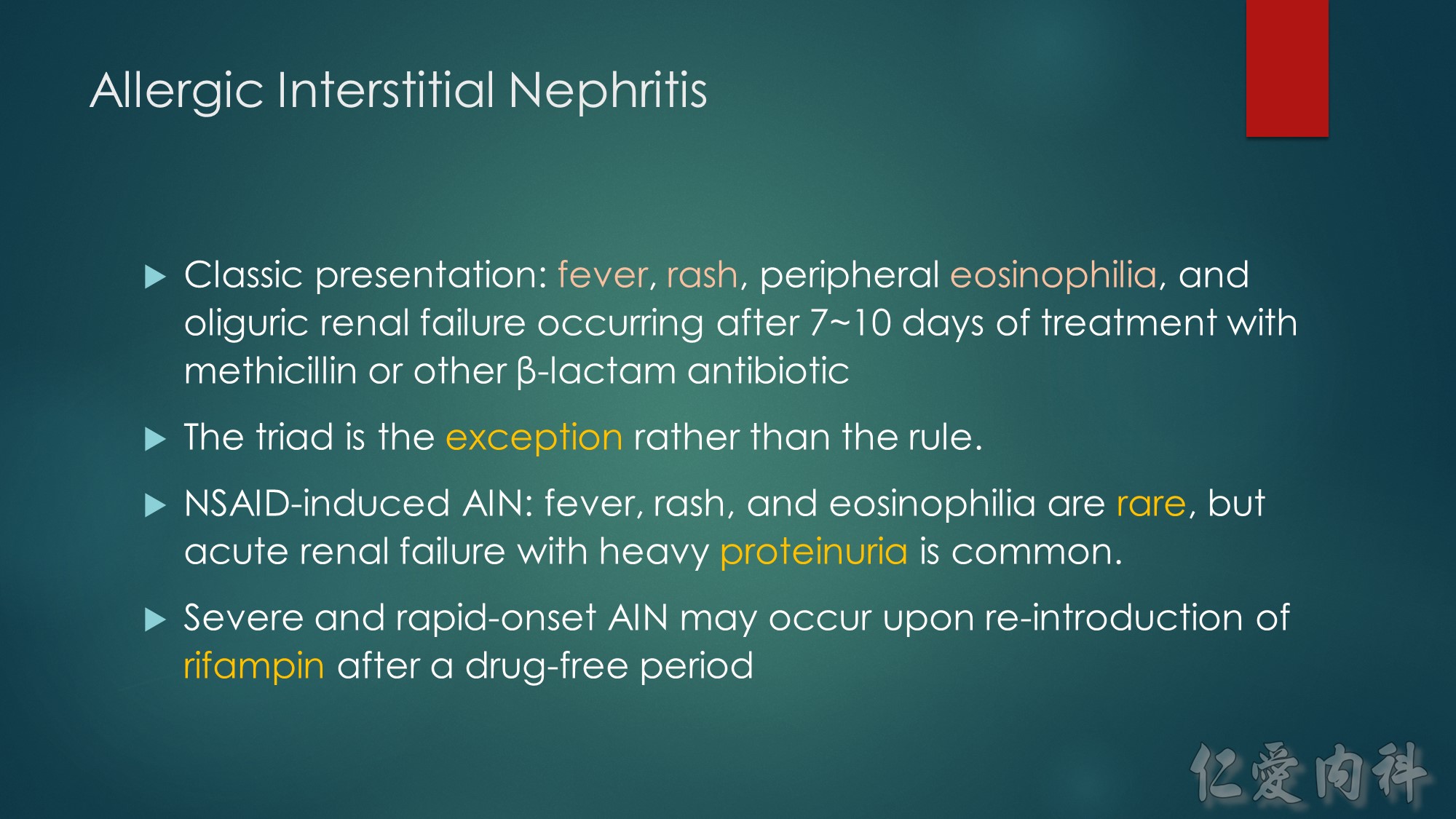
過去的AIN比較常看到符合triad,現在的AIN則罕見符合triad。
NSAID induced AIN少見符合 triad,但proteinuria則常見。
Rifampin若吃了停藥後再吃,體內易產生anti-rifampin Ab,攻擊腎臟,造成AIN。
教科書說:
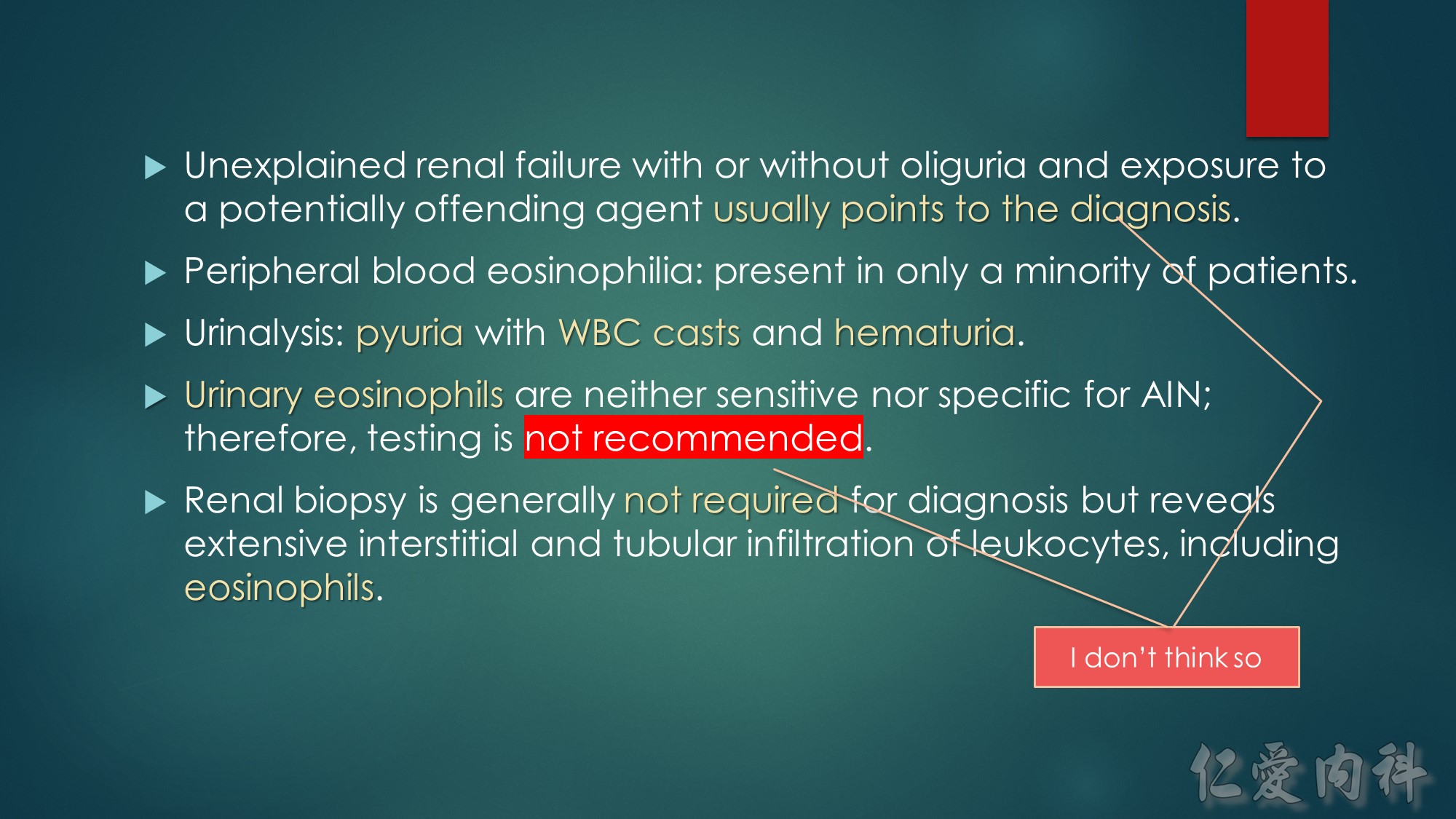
1.腎功能不好但找不到原因時,若能找到暴露於某個可能的affending agent時,通常那就是導致腎功能不好的原因。(授課徐主任覺得未必如此,事情沒那麼簡單!)
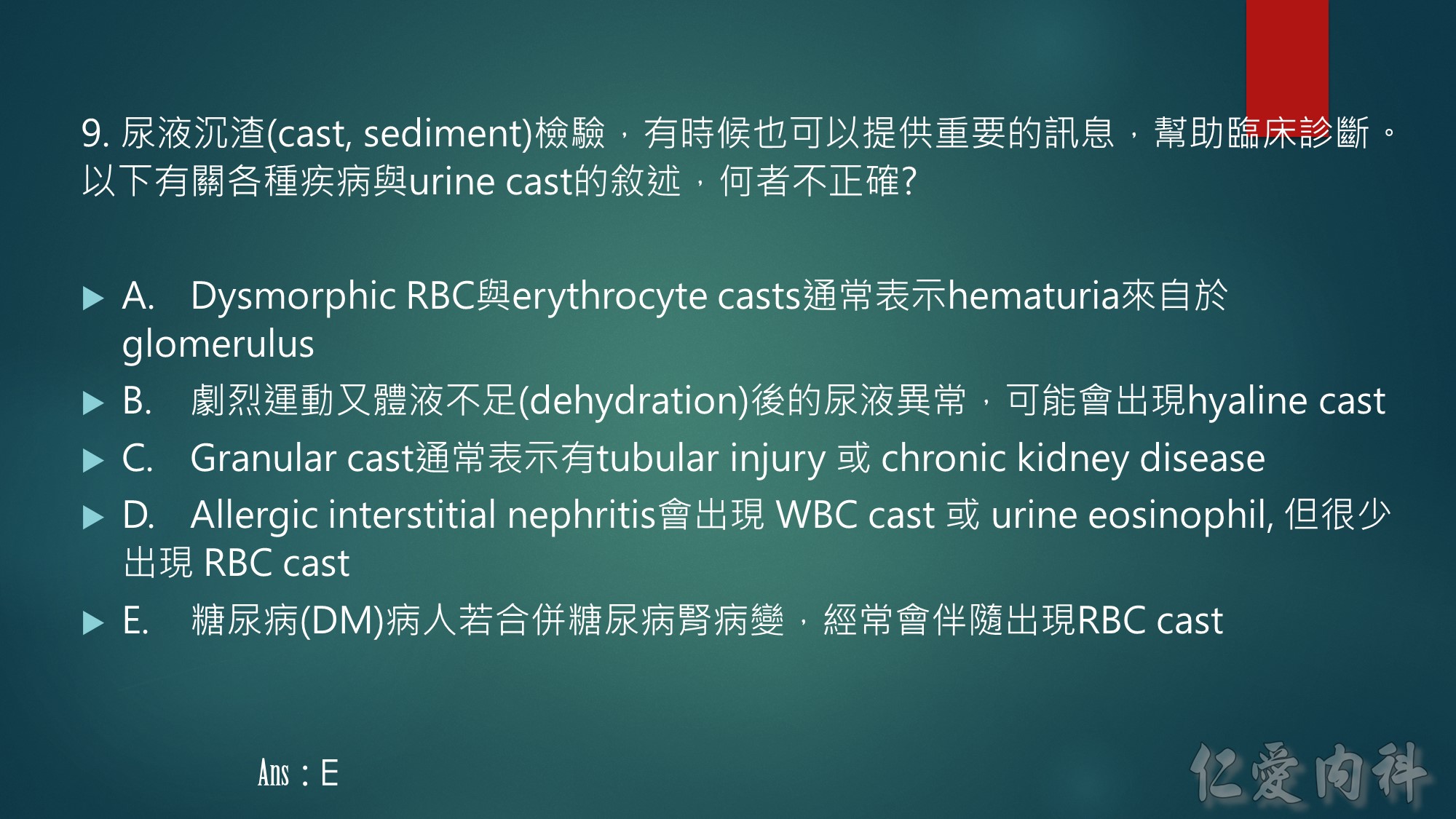
2.U/A: 有pyuria, WBC cast, hematuria。但有eosinophil是否就指向AIN?? NO! eosinophil是not specific to AIN的。
3.不須切片即能診斷。(徐主任不認為如此)
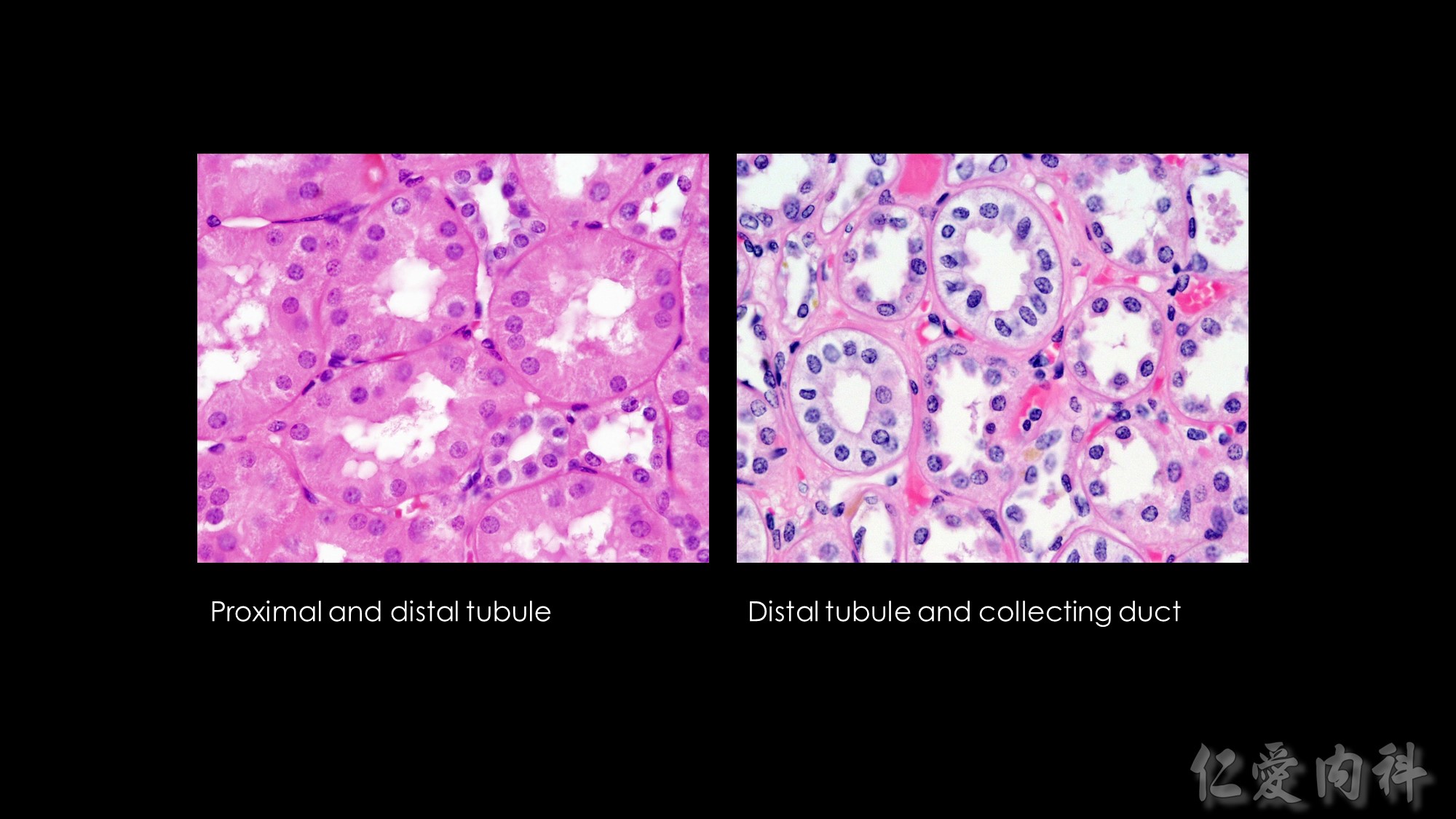
Tubule Histology
Proximal Convoluted Tubules (PCT)
brush border
star-shaped
larger outside diameter
Distal Convoluted Tubules (DCT)
clean lumen surface
apical nuclei
Collecting Tubules (CT)
larger lumen than DCT (about size of PCT)
cuboidal cells and smaller than DCT
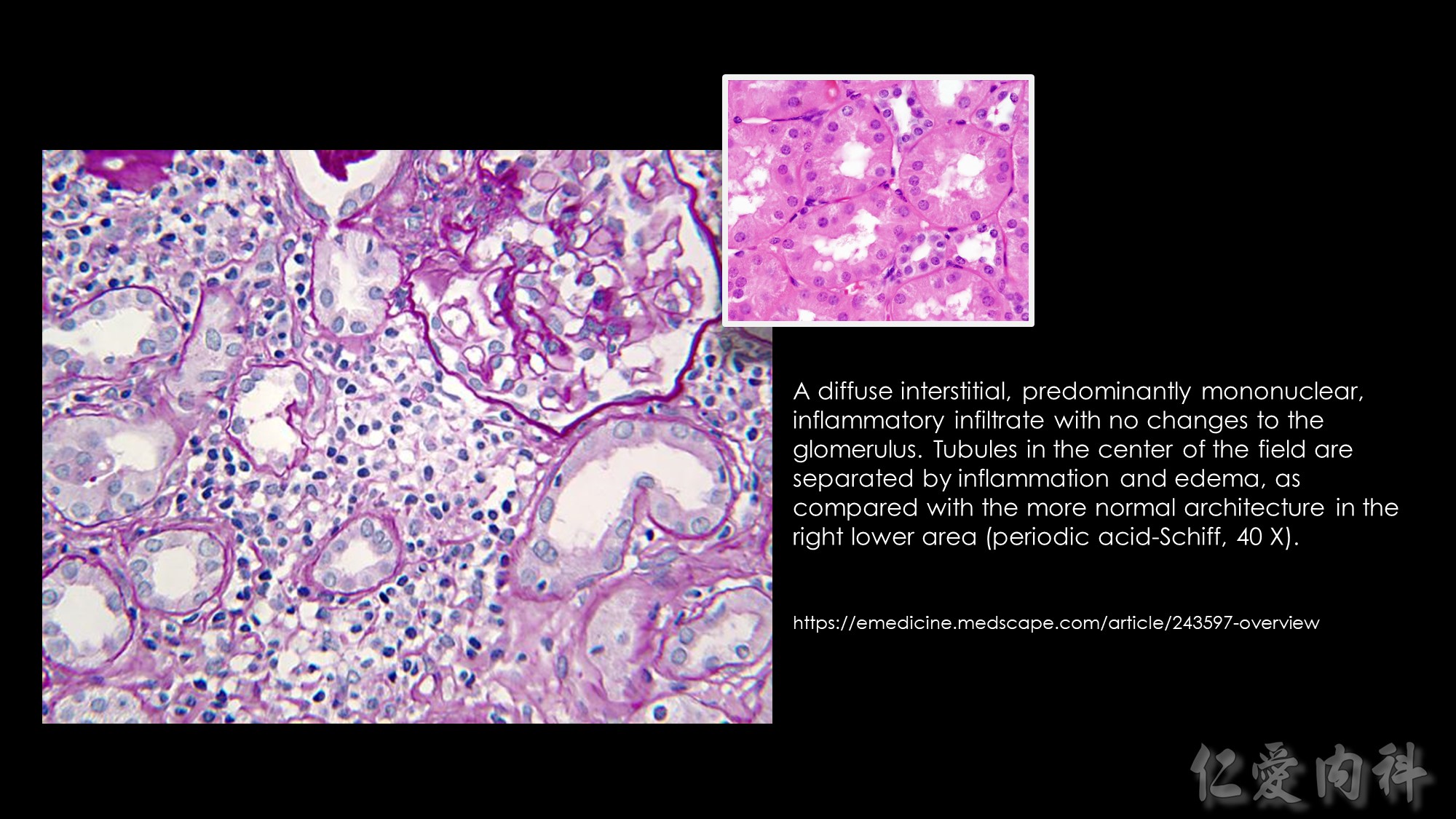
Tubule之間距離遠,chronic infiltration
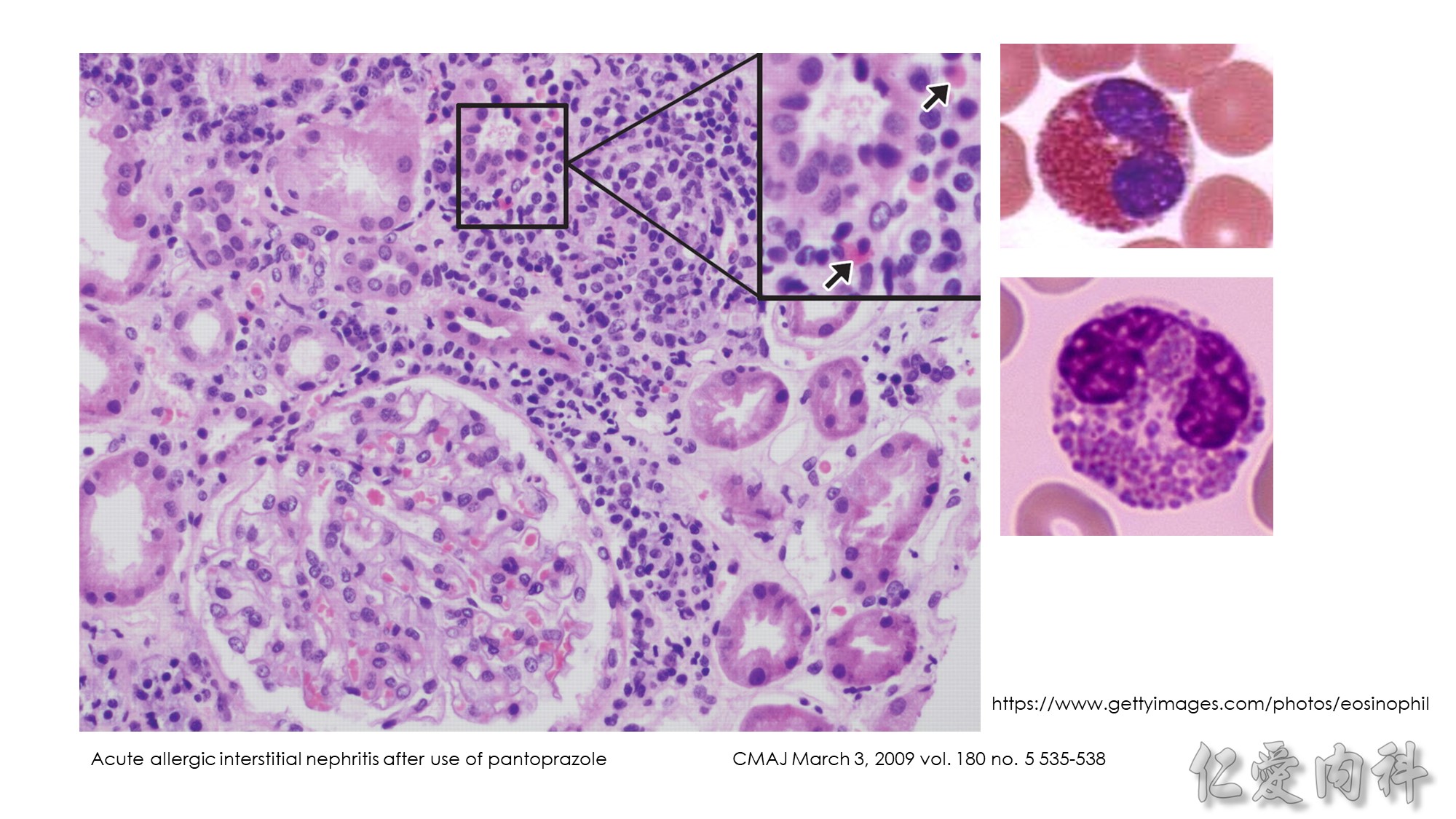
右上圖為eosinophil(看起來像戴太陽眼鏡曬太陽,臉紅紅XD)
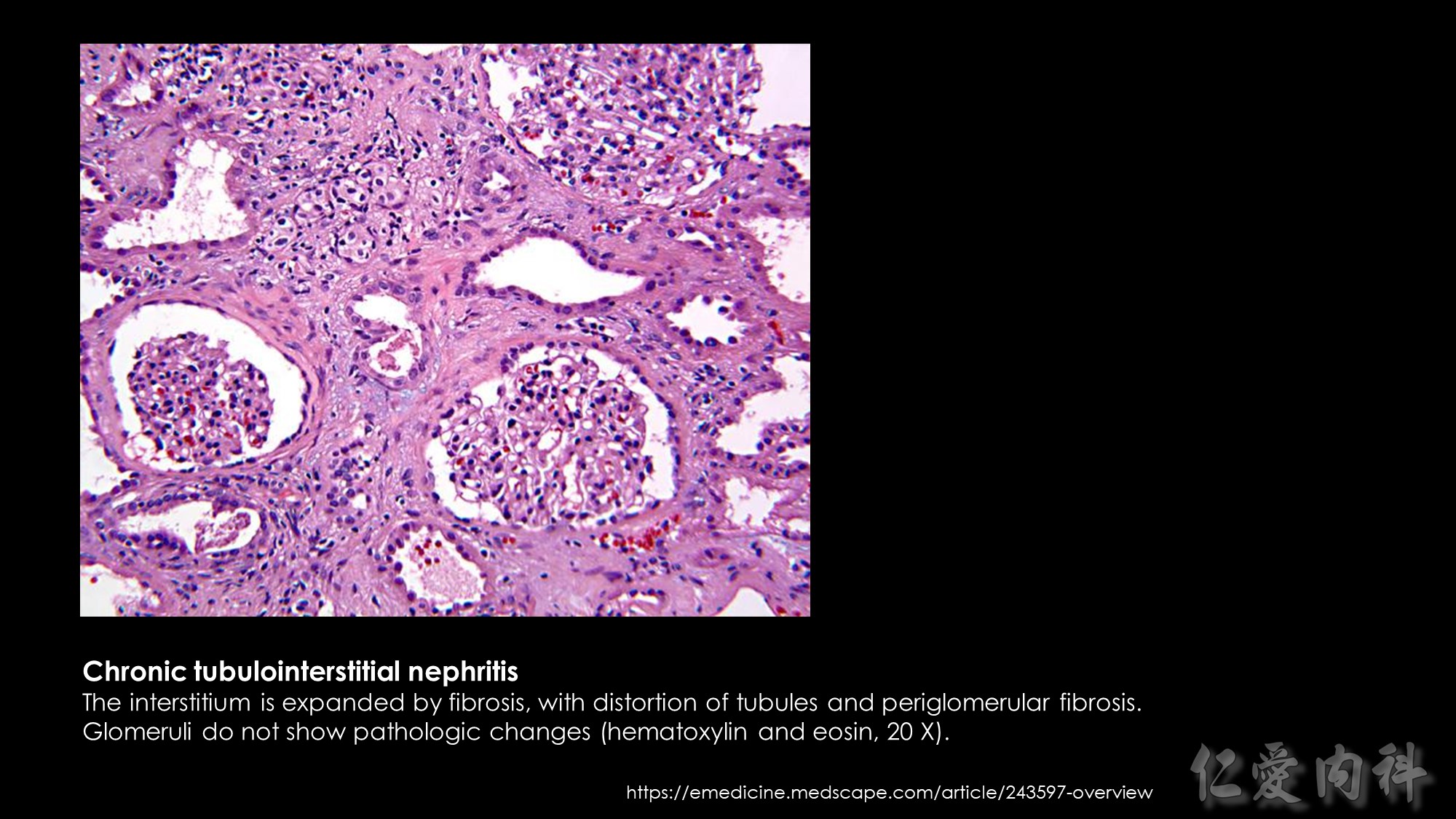
腎絲球之間距離非常遠,CTIN
藥物使用時間長短與腎功能損害的程度、是否需要洗腎,沒有直接的關係。
預測腎功能最好的指標仍是biopsy看有沒有interstitial fibrosis
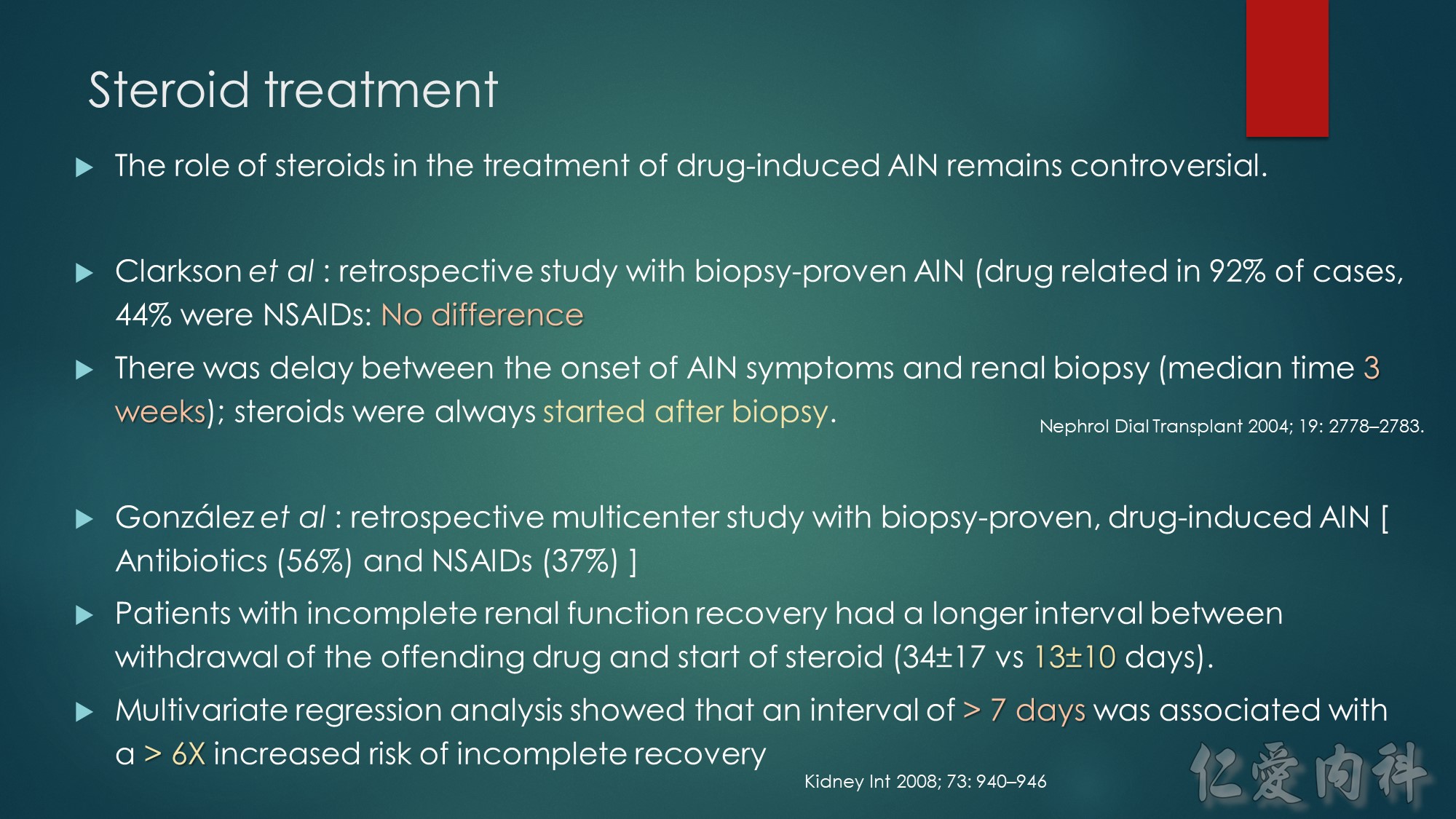
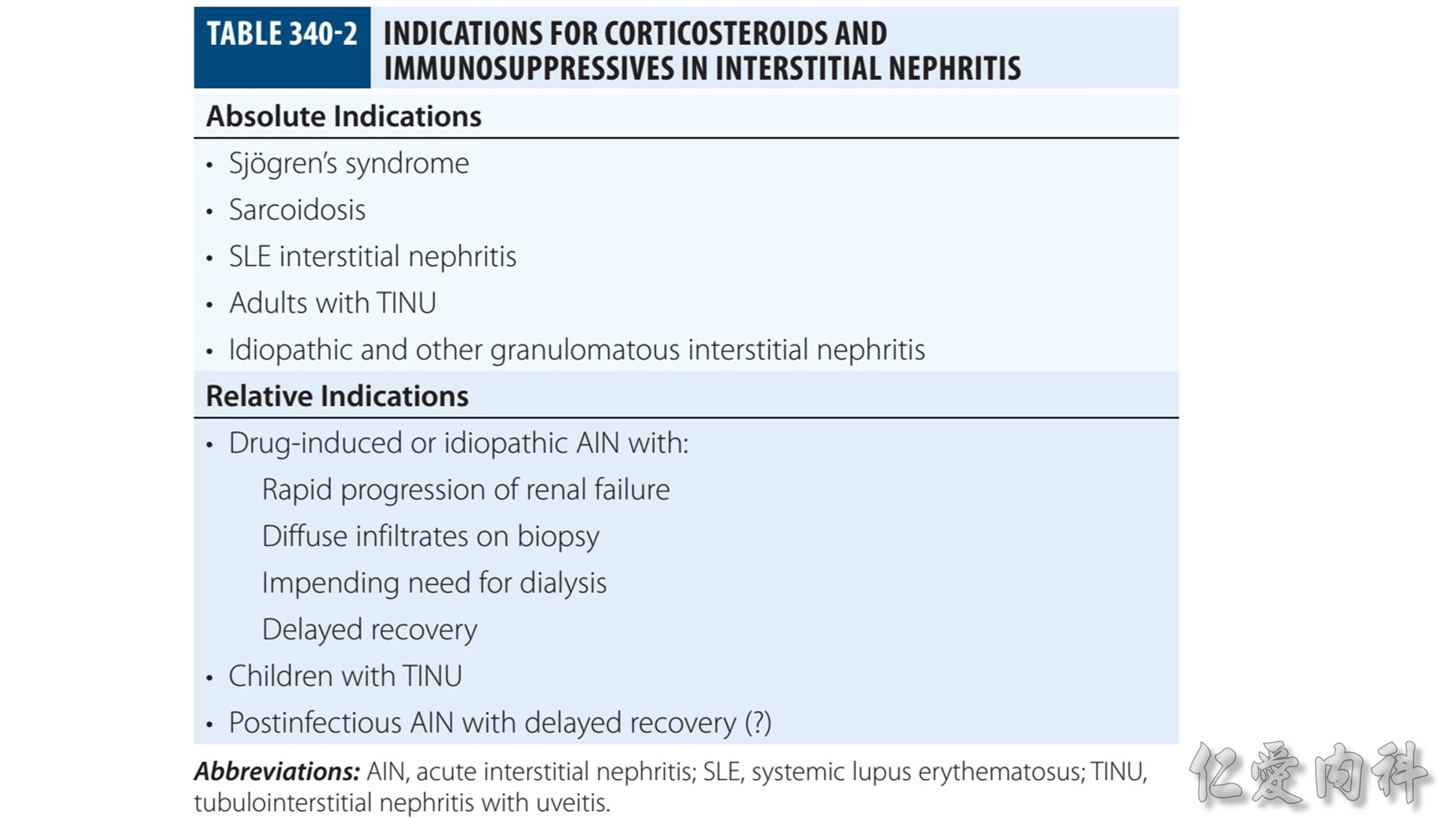
AIN是否給steroid?
一旦懷疑是AIN就應馬上給steroid,目前evidence指出,超過七天才給steroid,其治療無效的risk上升。
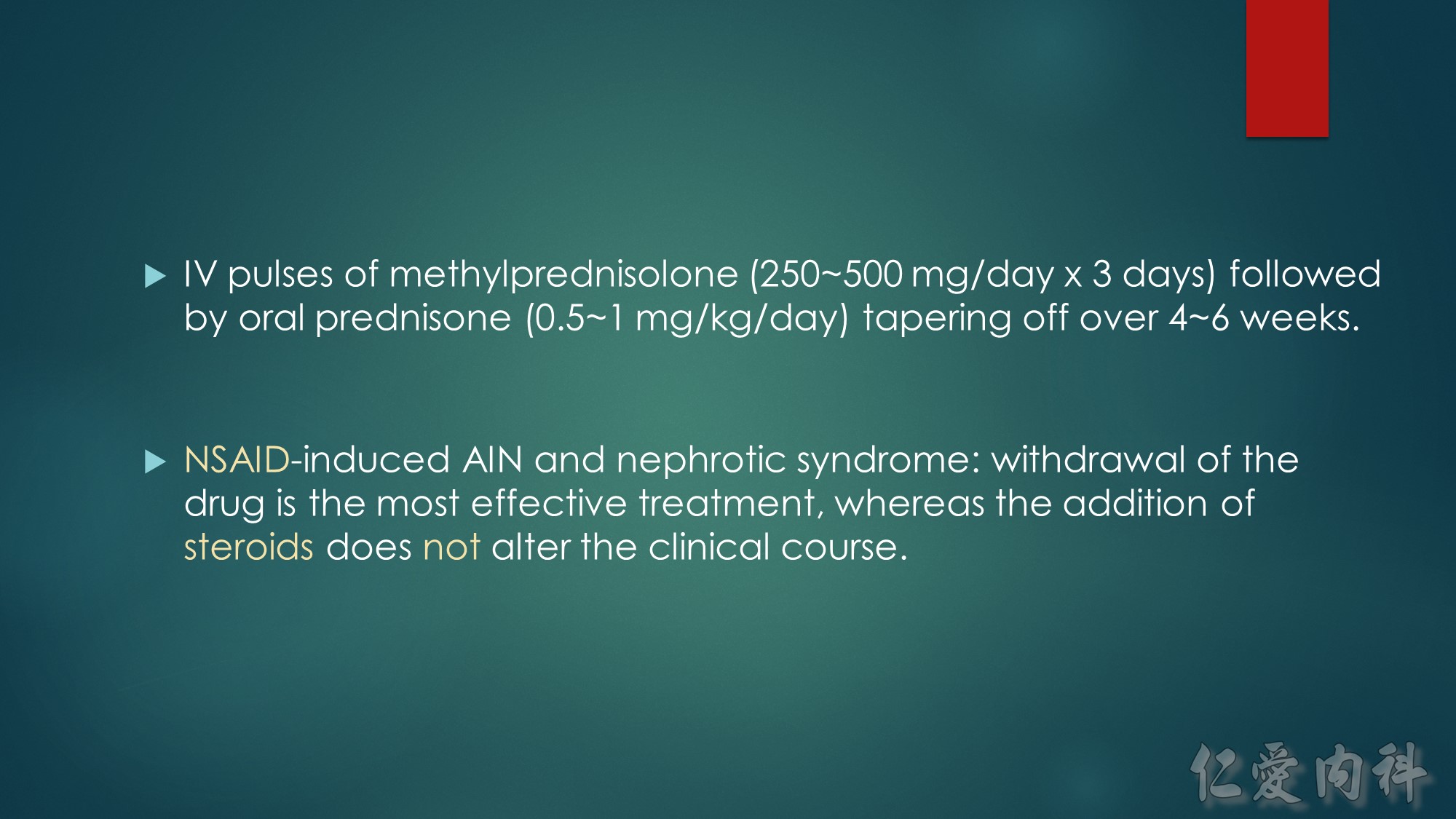
使用pulse steriod治療三天、再換回口服。
若是NSAID造成的AIN,使用steroi就沒有效!
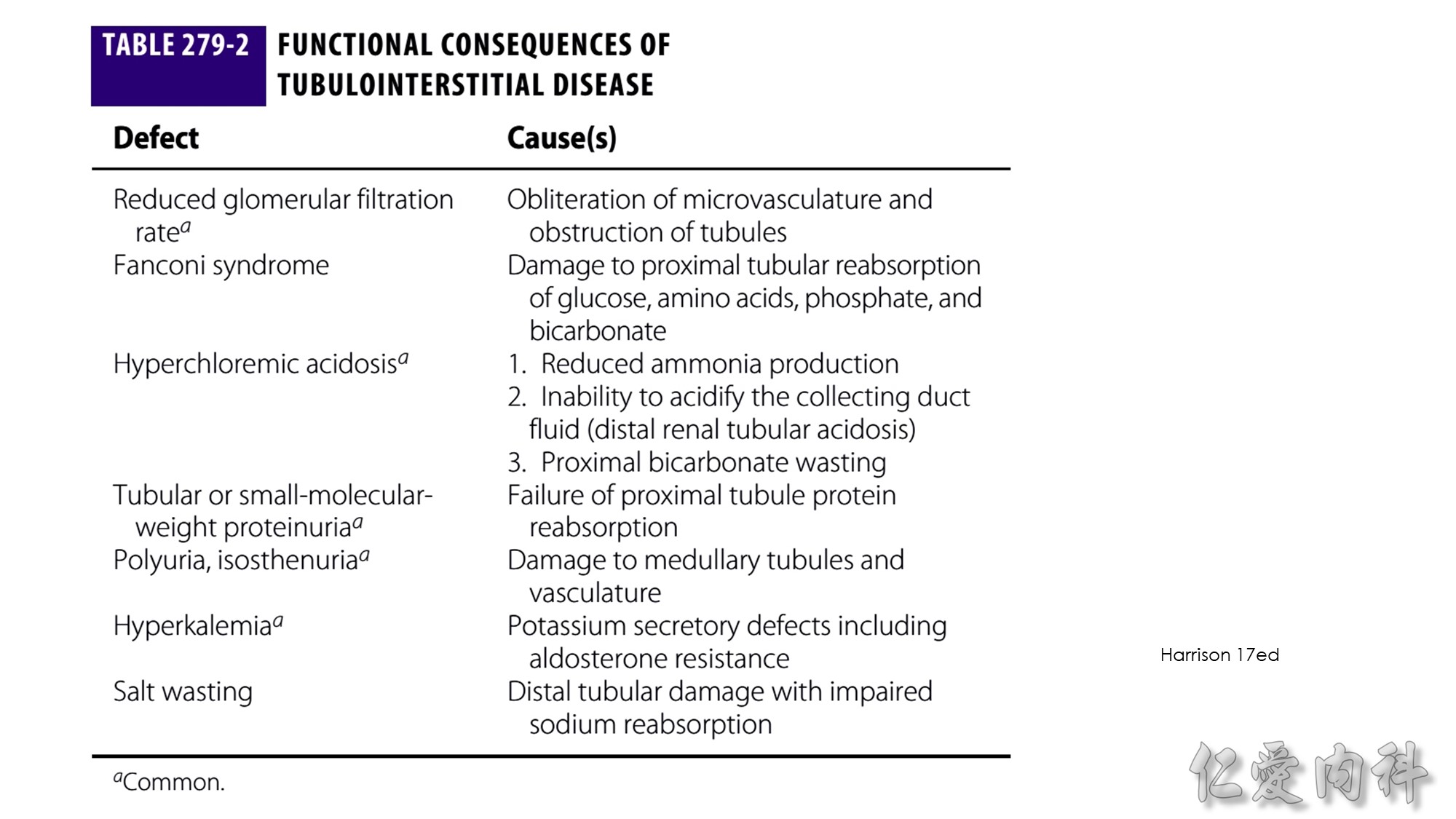
Harrison表格。
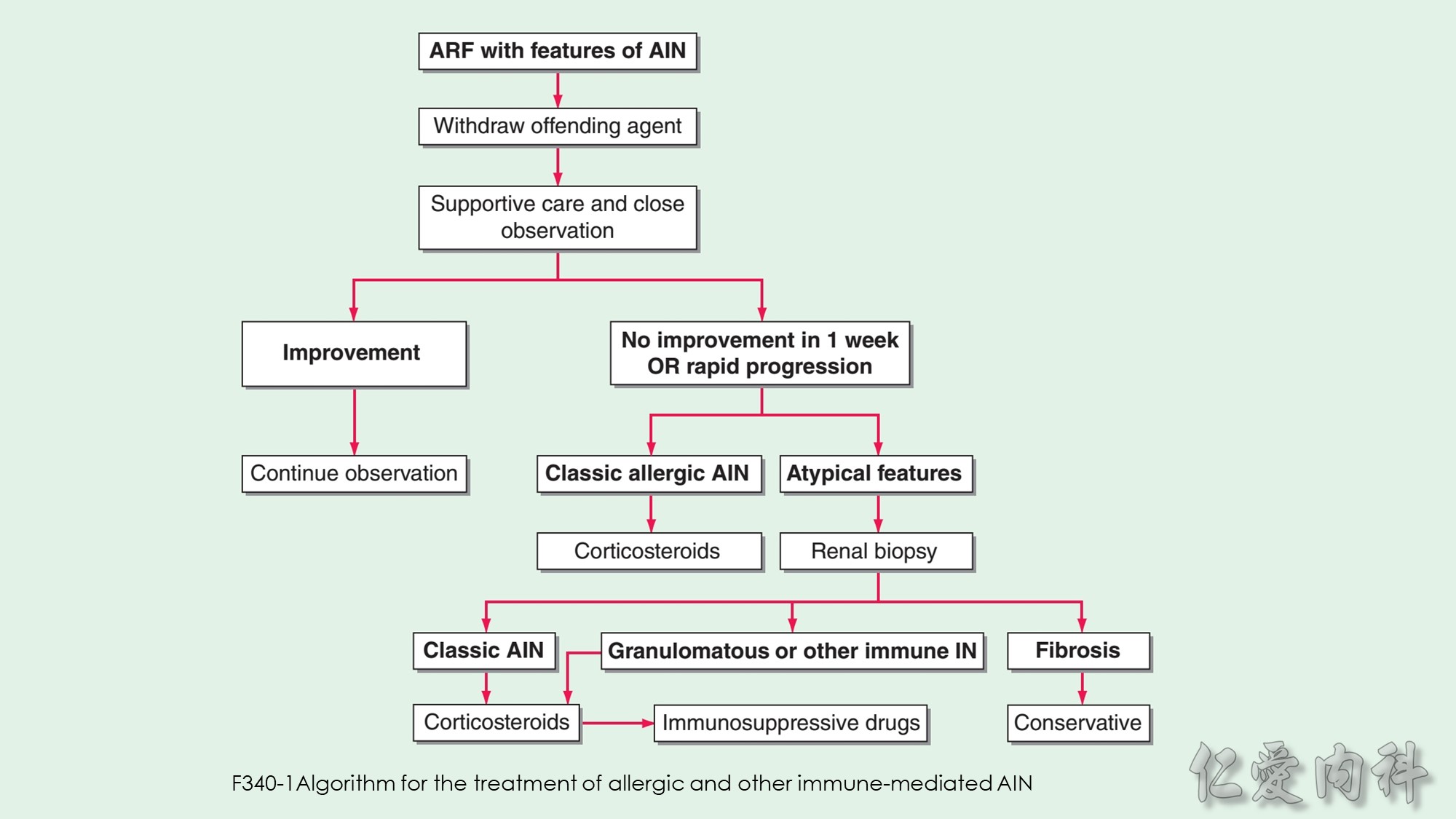
一旦懷疑是AIN,第一步先把affending drug拿掉,觀察一周之後如果沒有改善、甚至是持續惡化,仍懷疑是AIN時就直接使用steroid;不是很確定是AIN的case就坐biopsy,結果出來是AIN依舊是Steroid!!!!
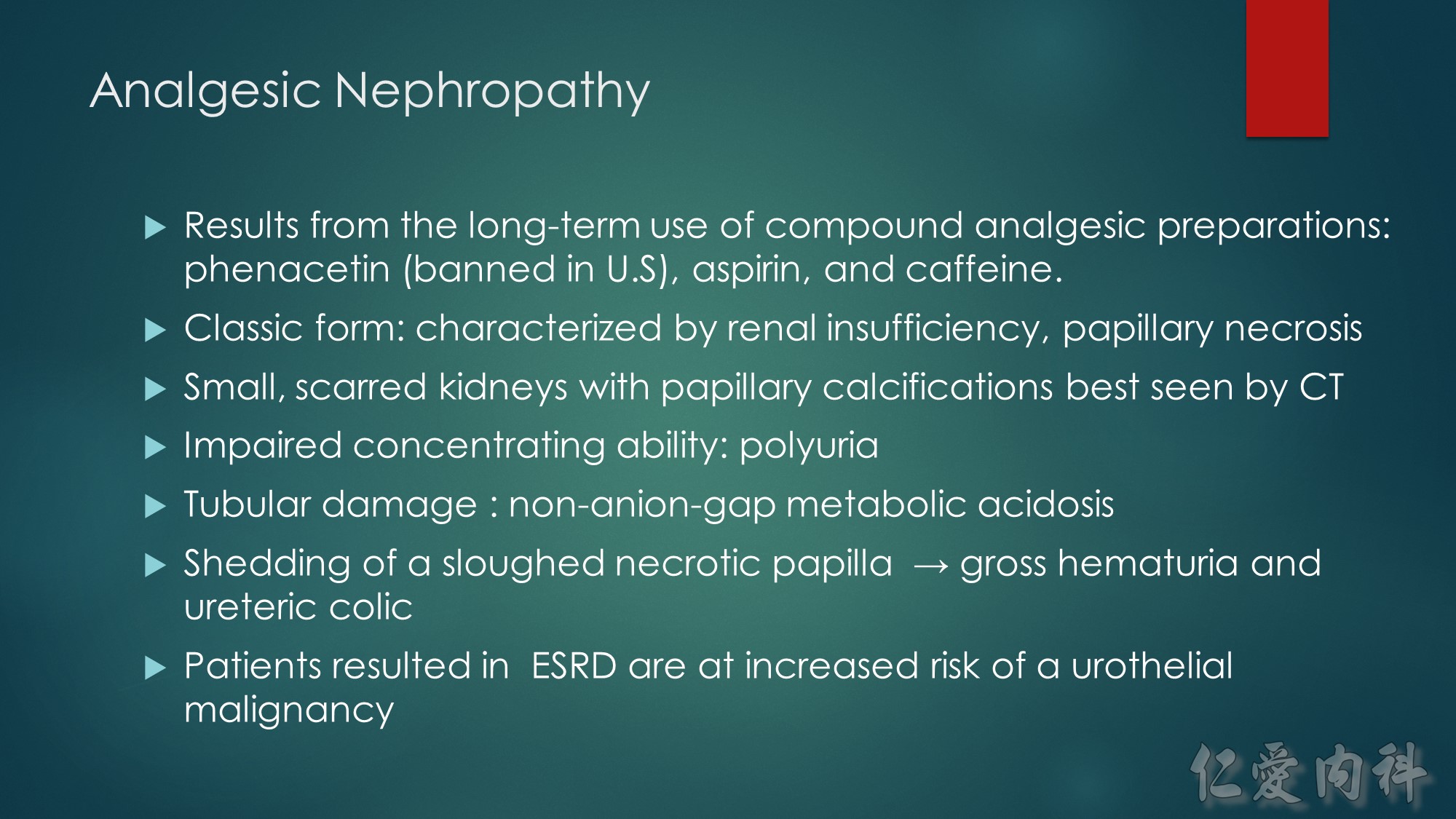
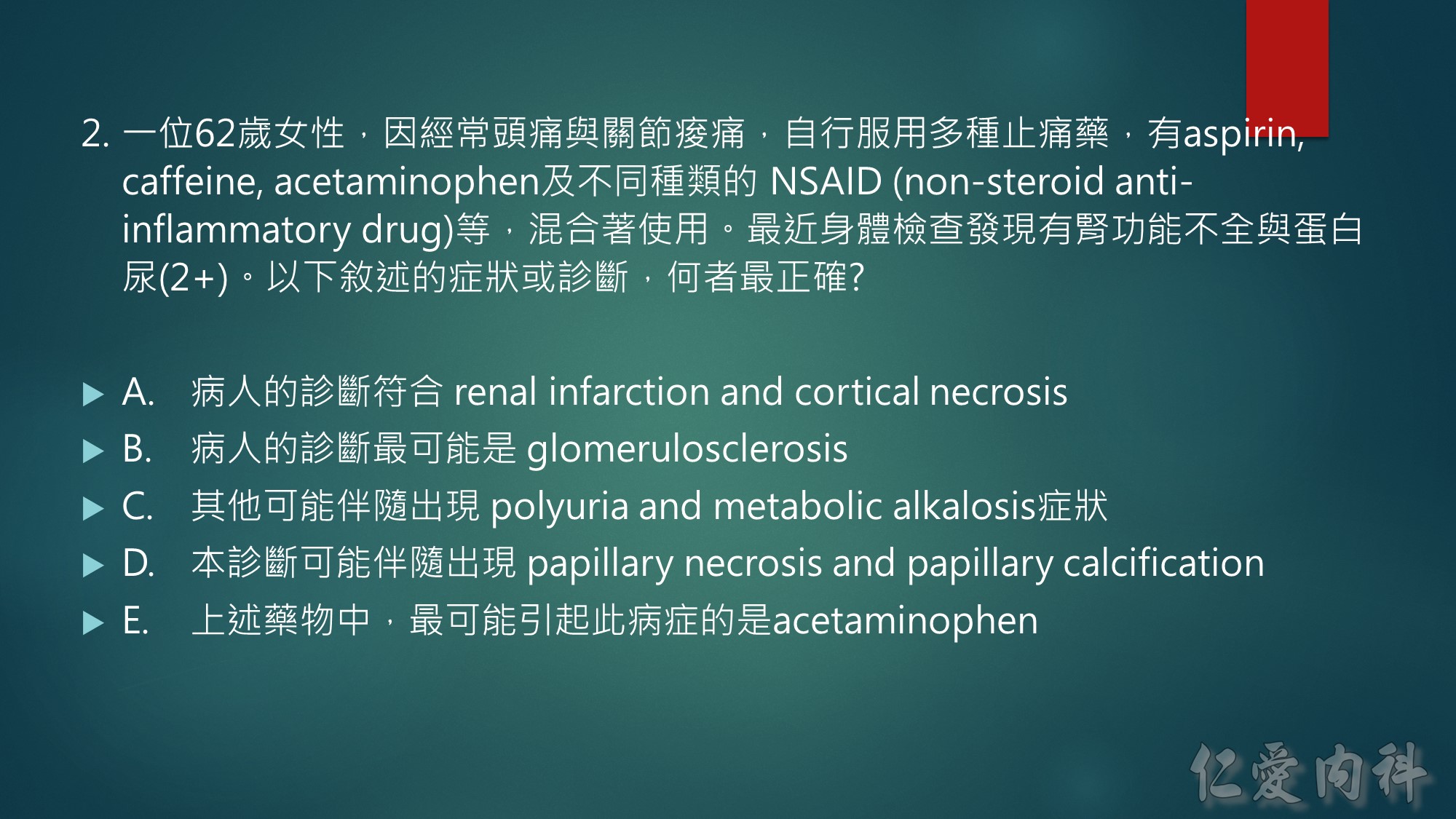
止痛藥造成的nephropathy通常是好幾種止痛藥一起吃。
NSAID造成的nephropathy進一步造成的ESRD,會增加urothelial ca.的risk
馬兜鈴酸也同樣會造成上述的injur的risk of urothelial ca.
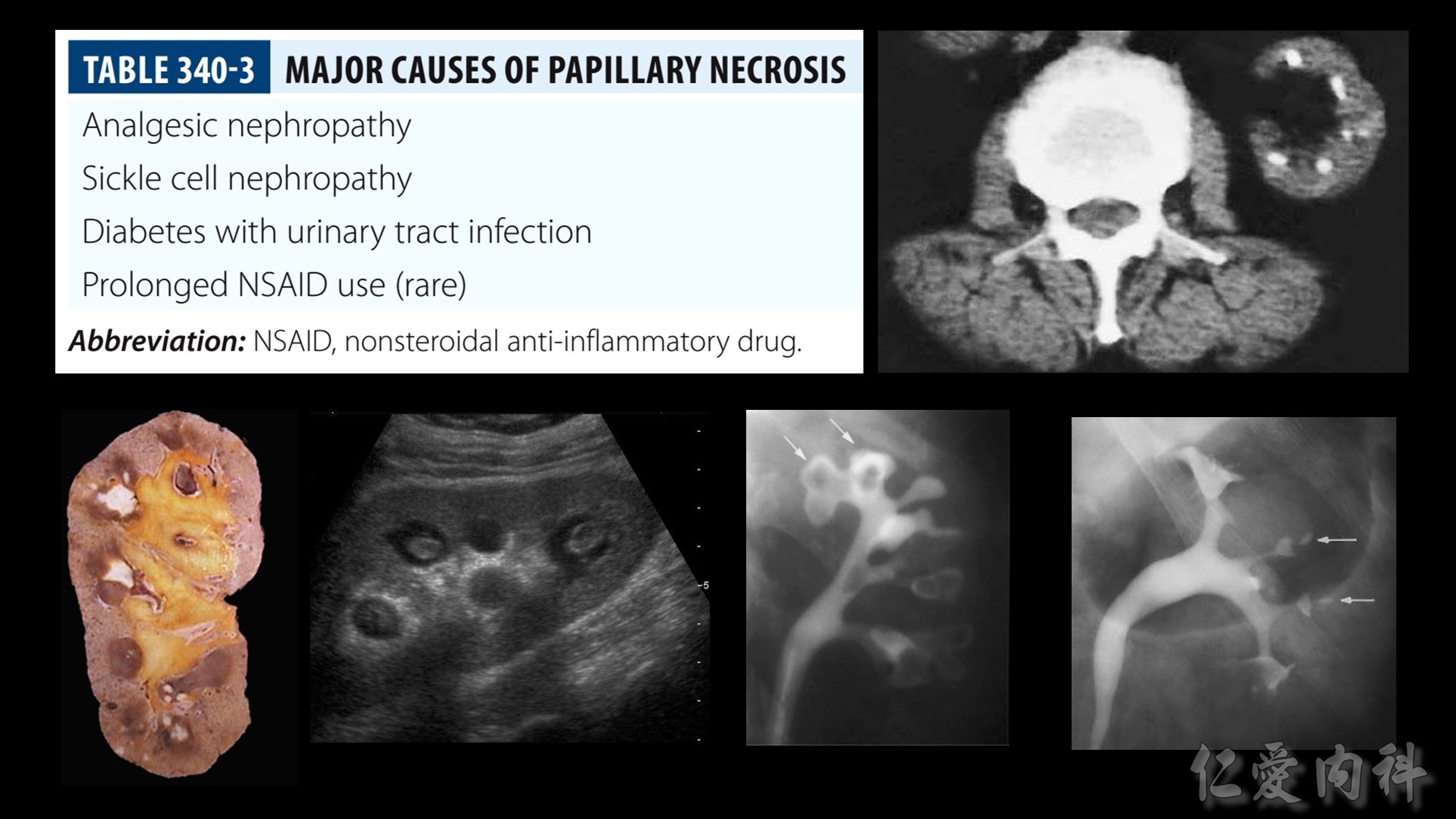
影像可看到小小的腎臟,及papilla calcification
IVP可見一球一球黑黑的,是鈣化失去功能的papilla。
其他可能造成papillary necrosis的情形列於上表。
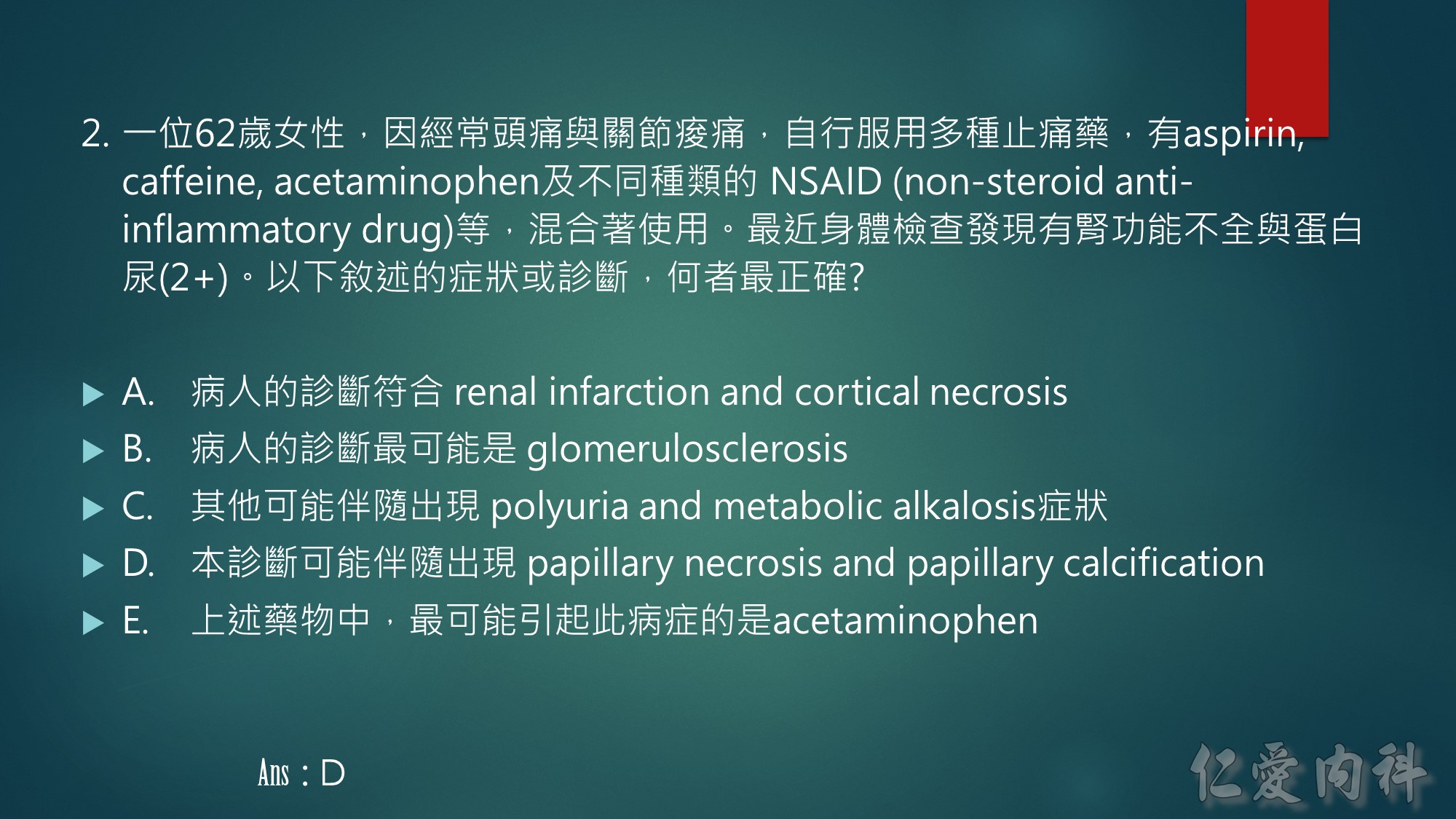
A: renal infarction 通常是acute renal failure,腰痛血尿。非cortical necrosis, 是papillary necrosis
B: not GN
C: metabolic acidosis
E: NSAID
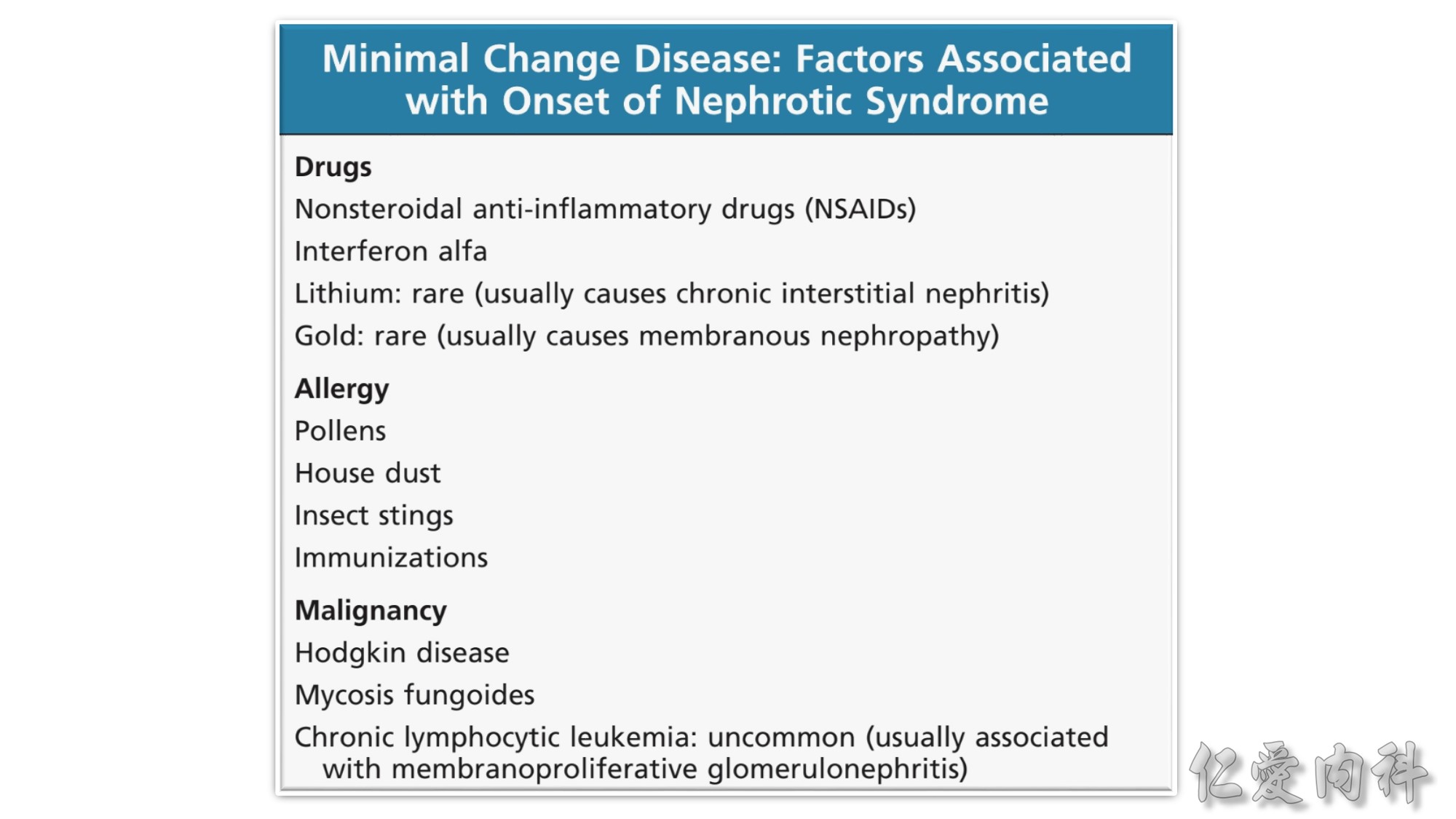
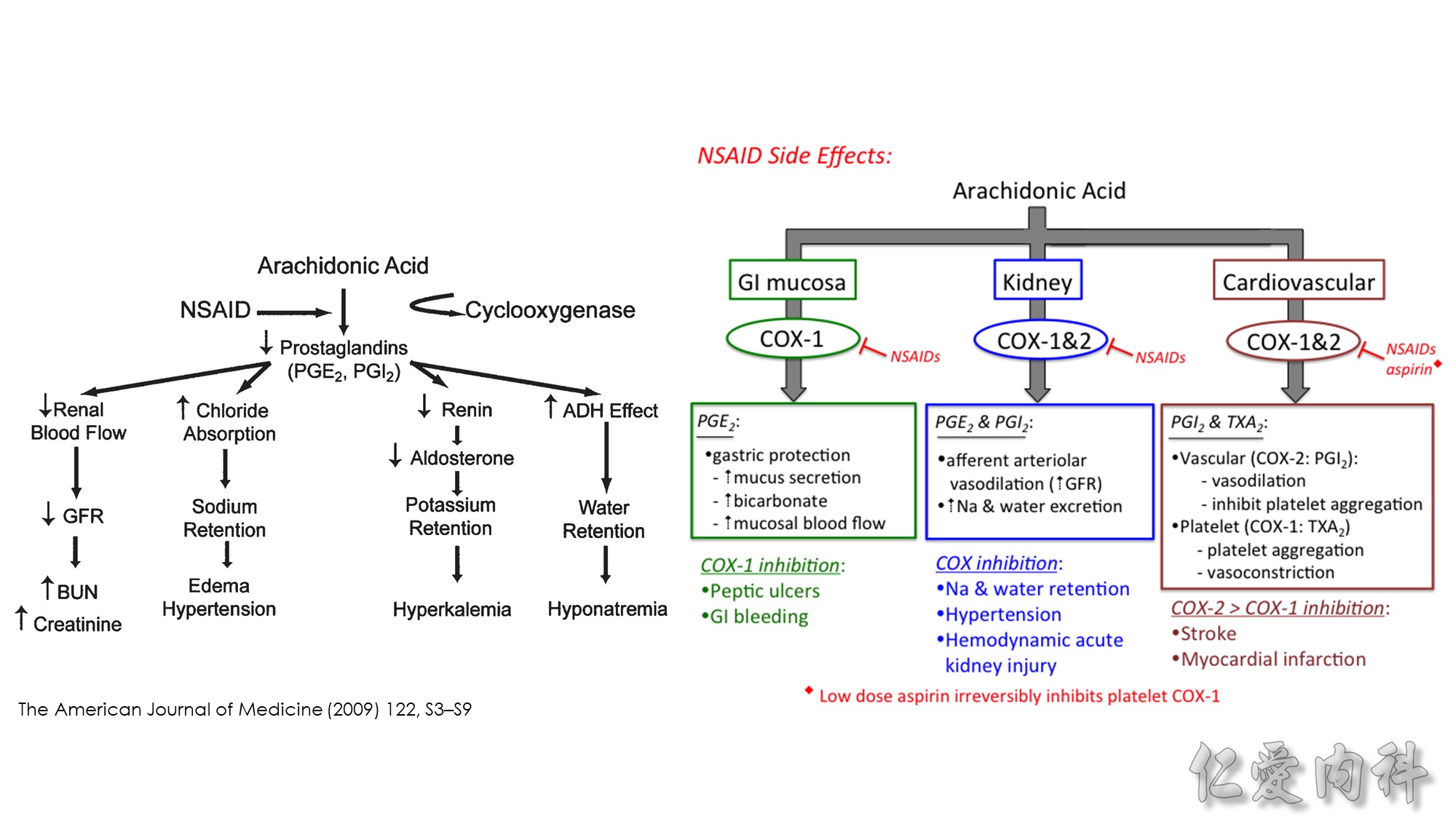
NSAID造成的腎絲球腎炎是minimal change disease
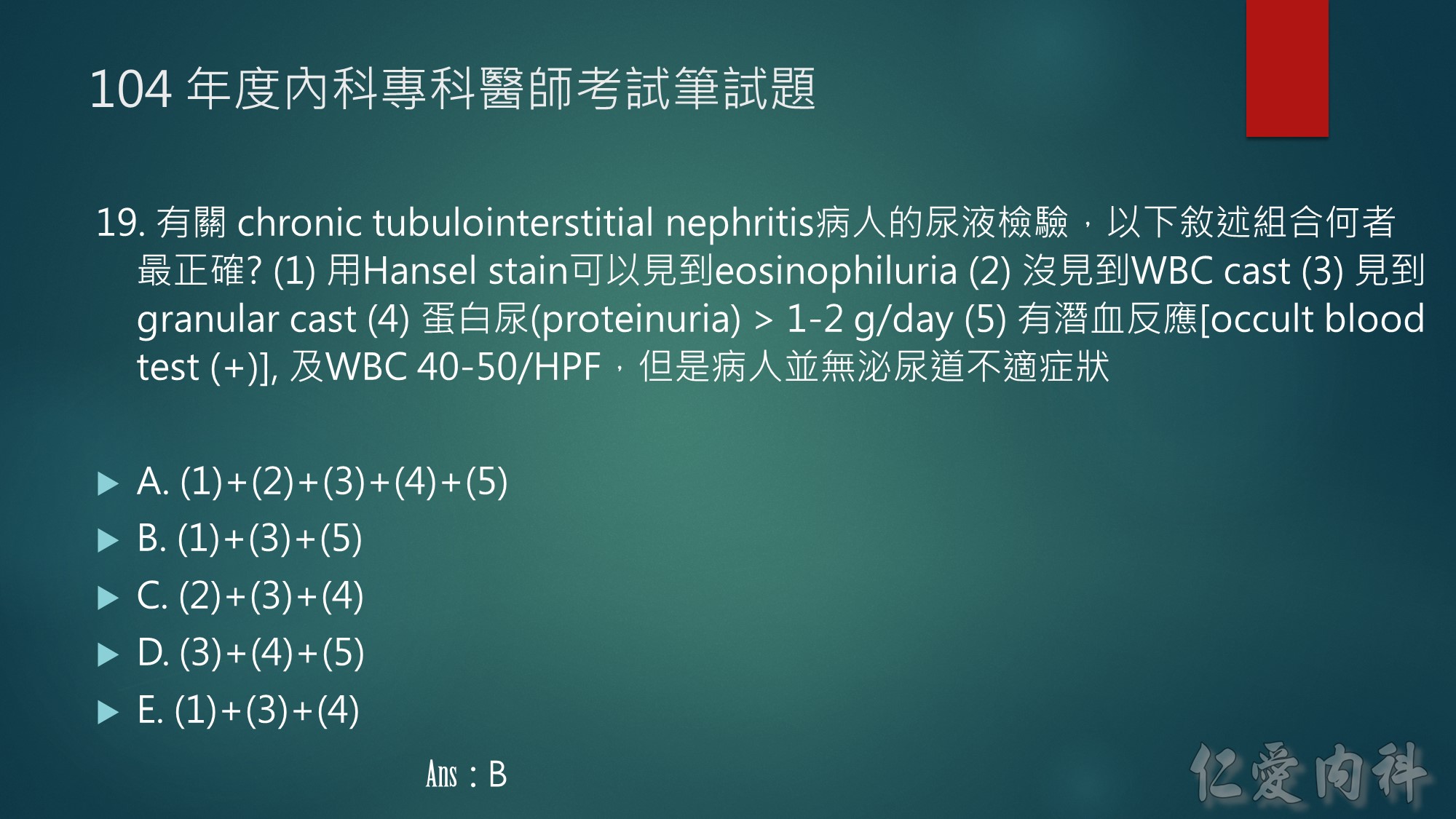
可見WBC cast,proteinuria < 1-2g/day
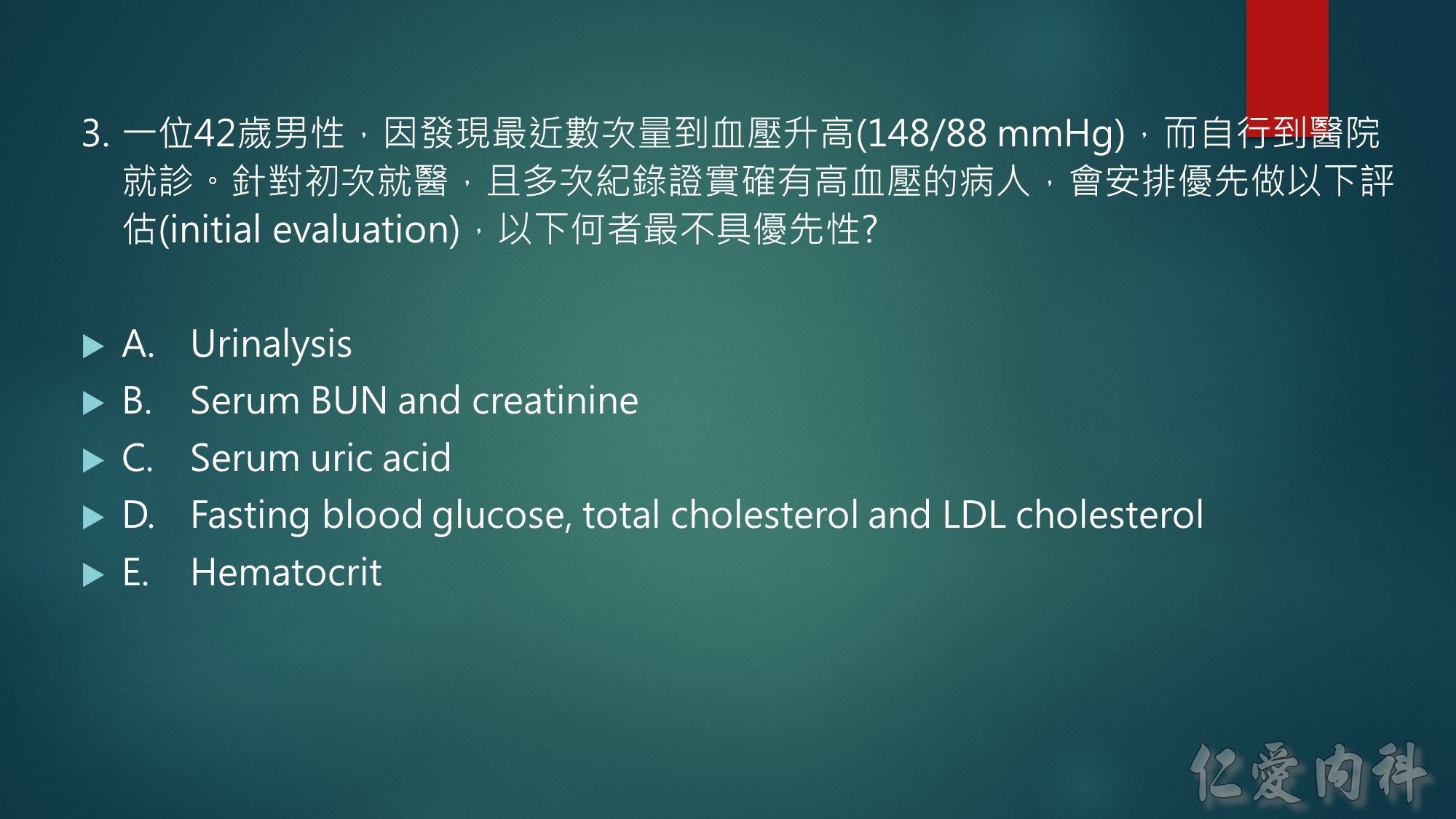
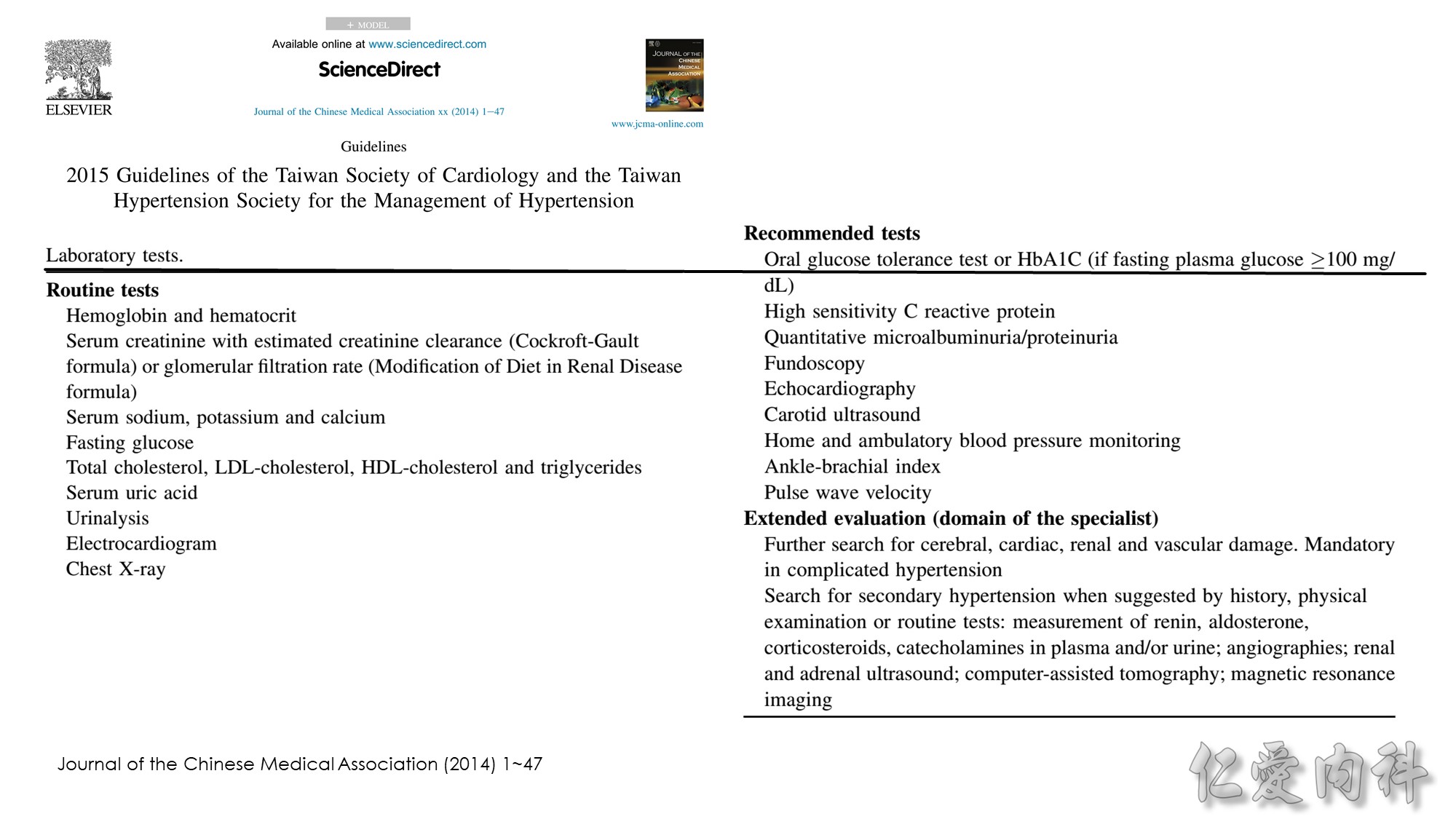
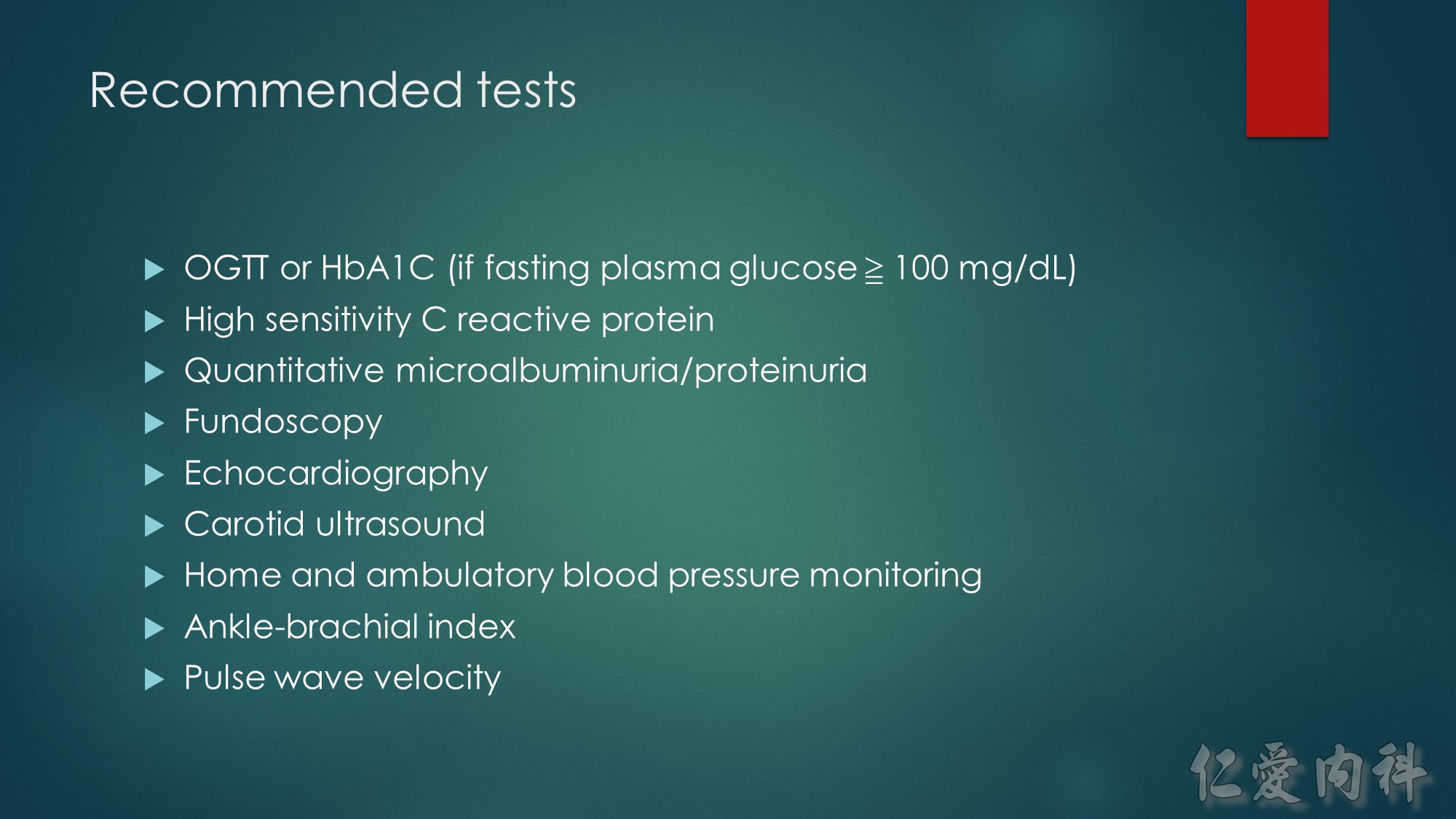
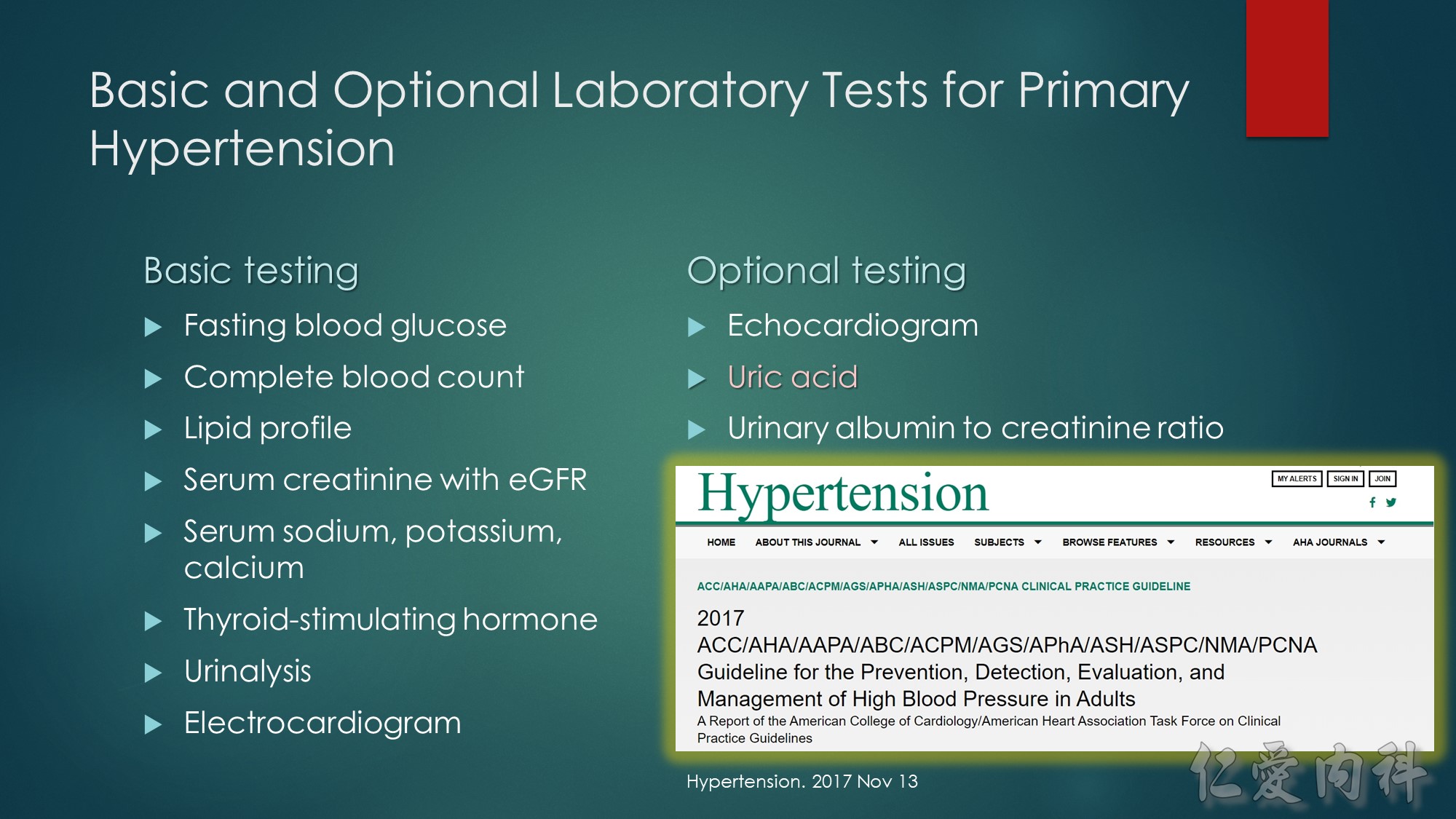
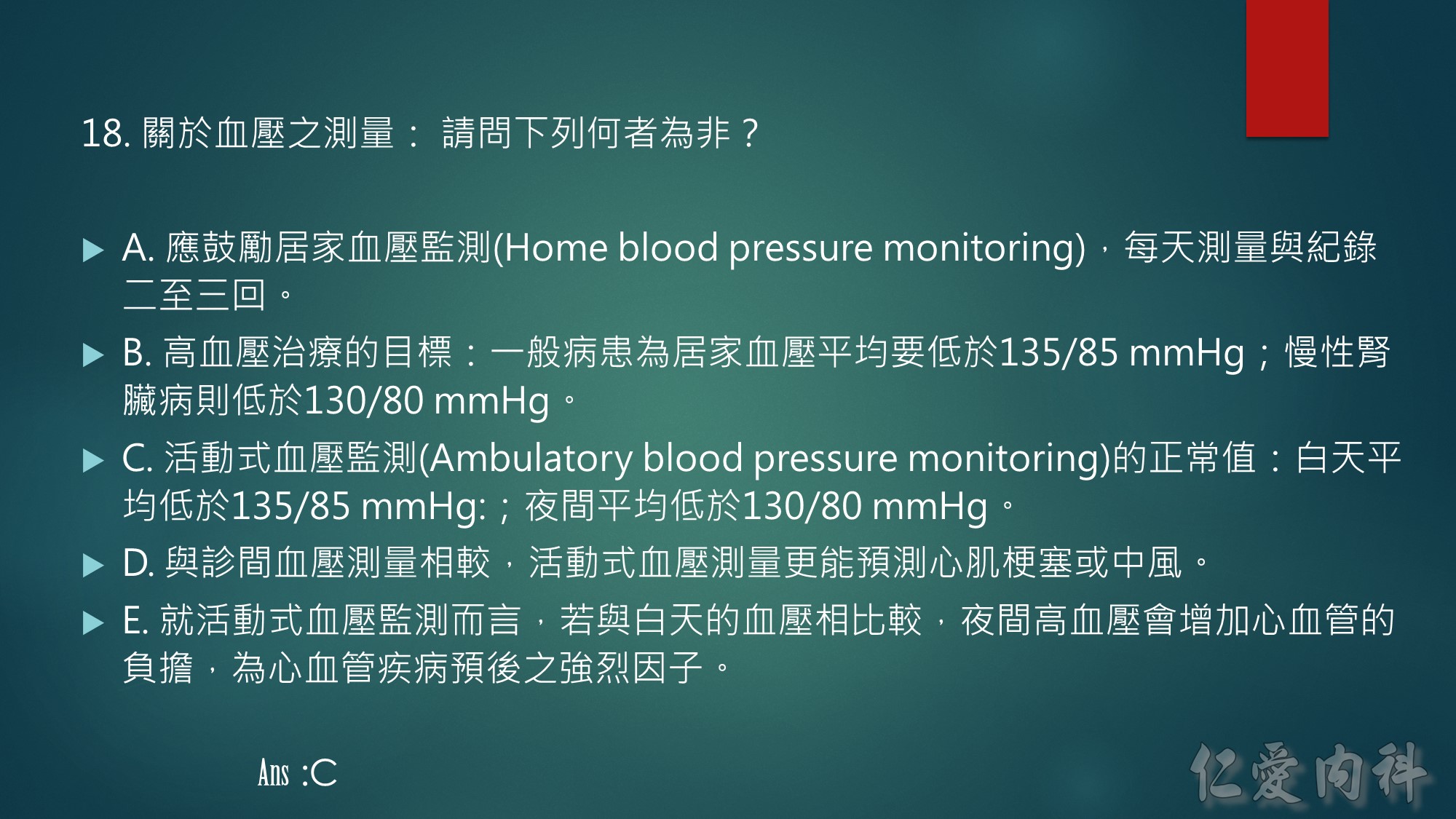
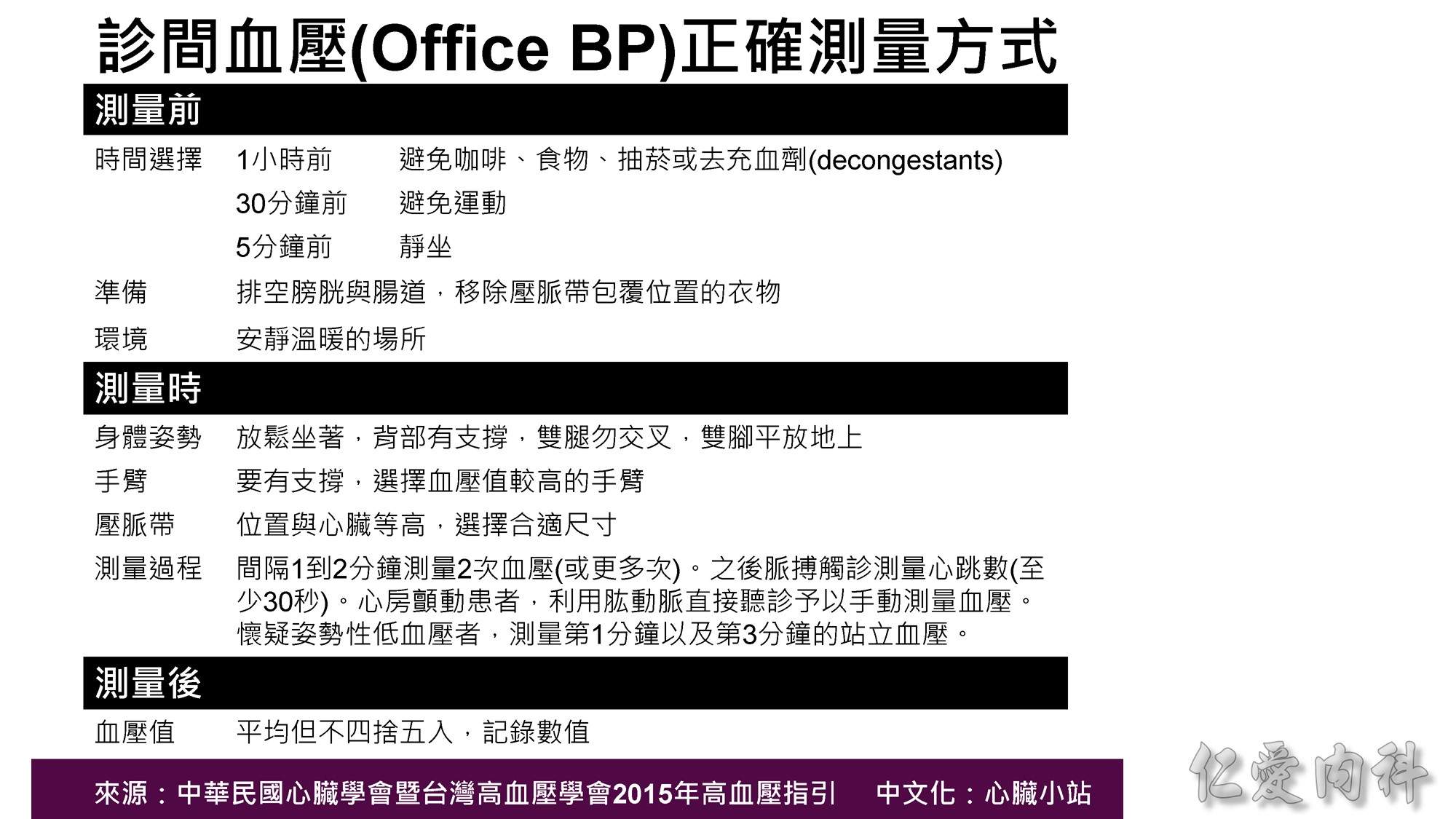
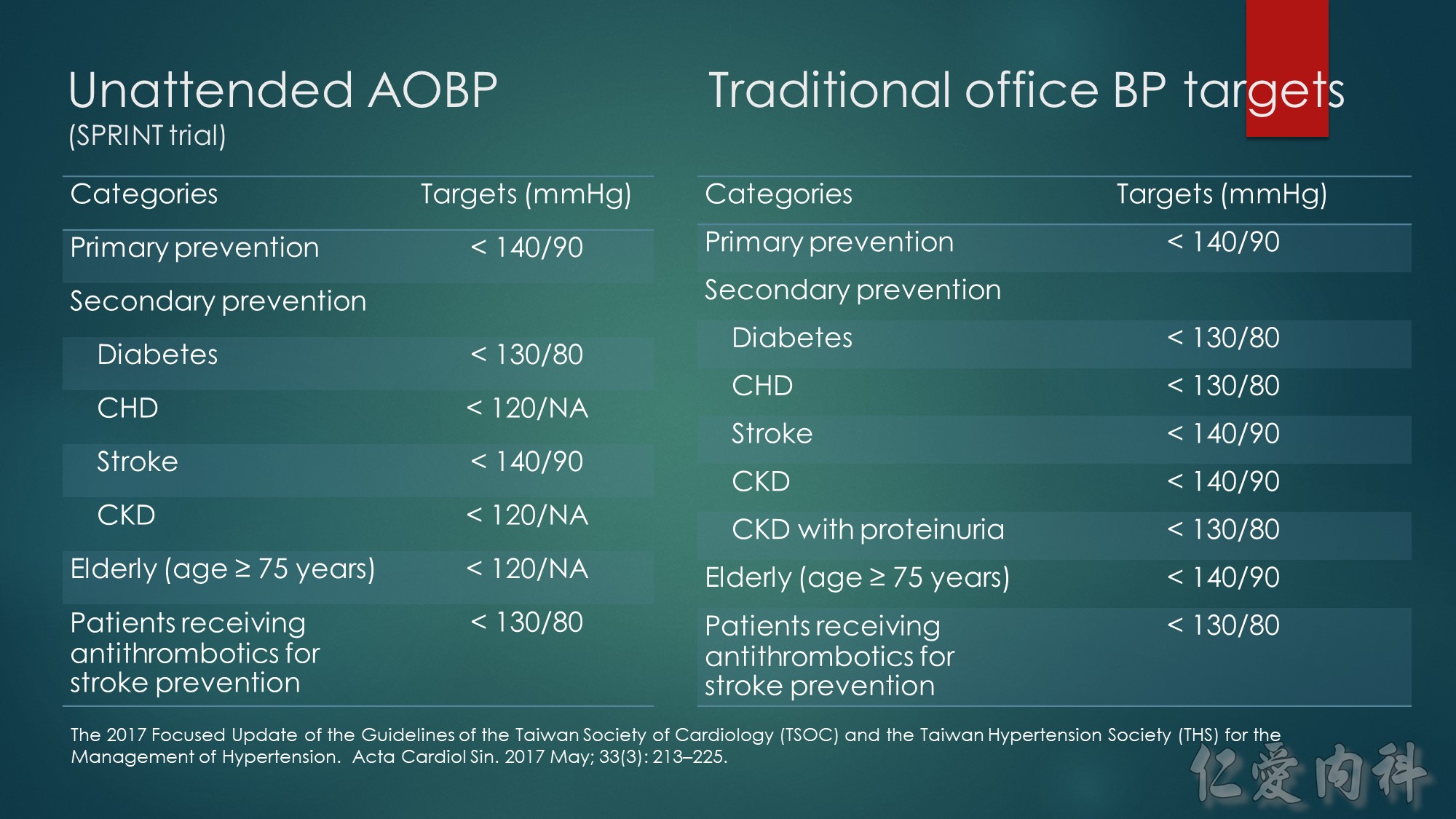
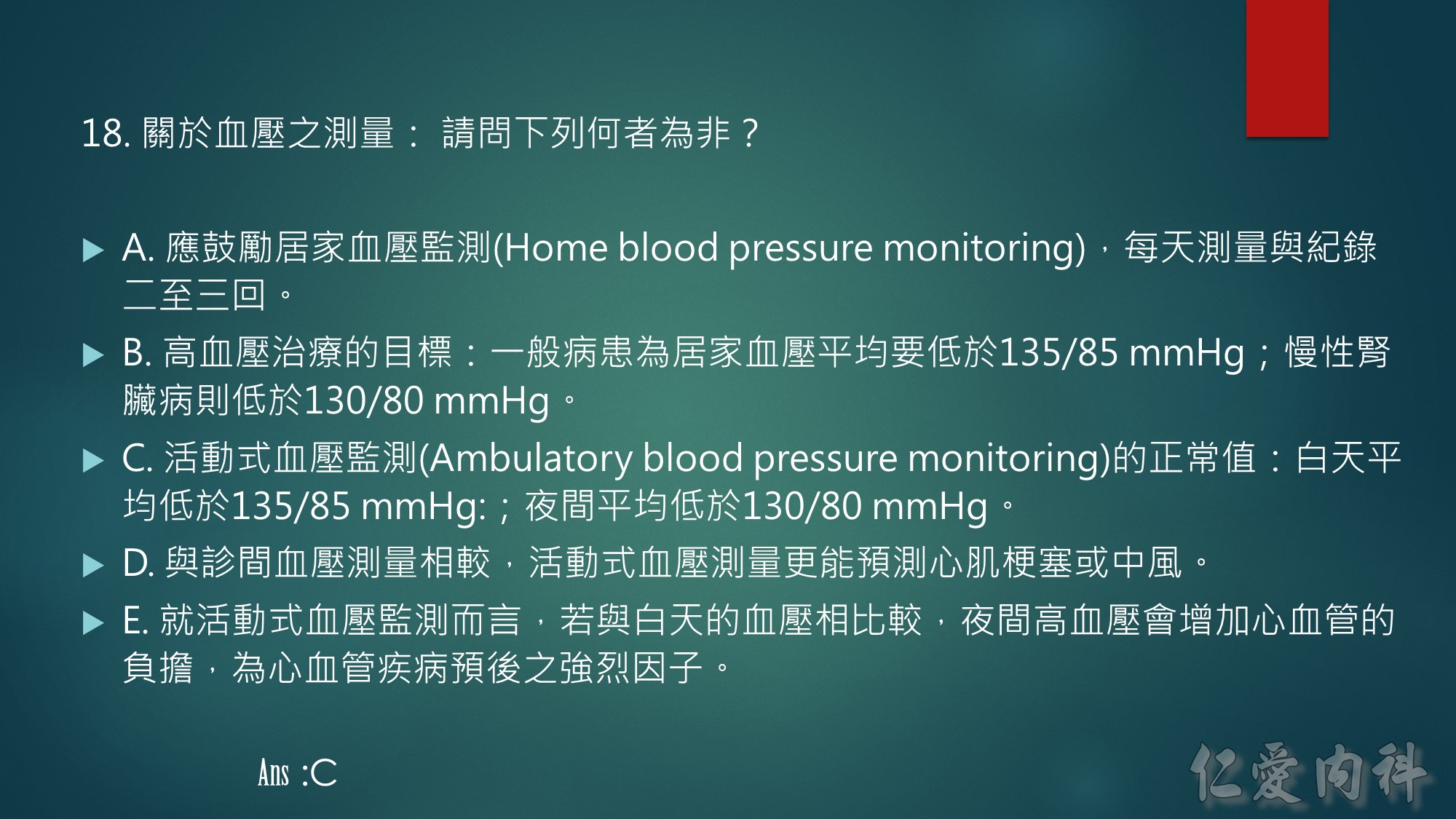
台灣高血壓guideline
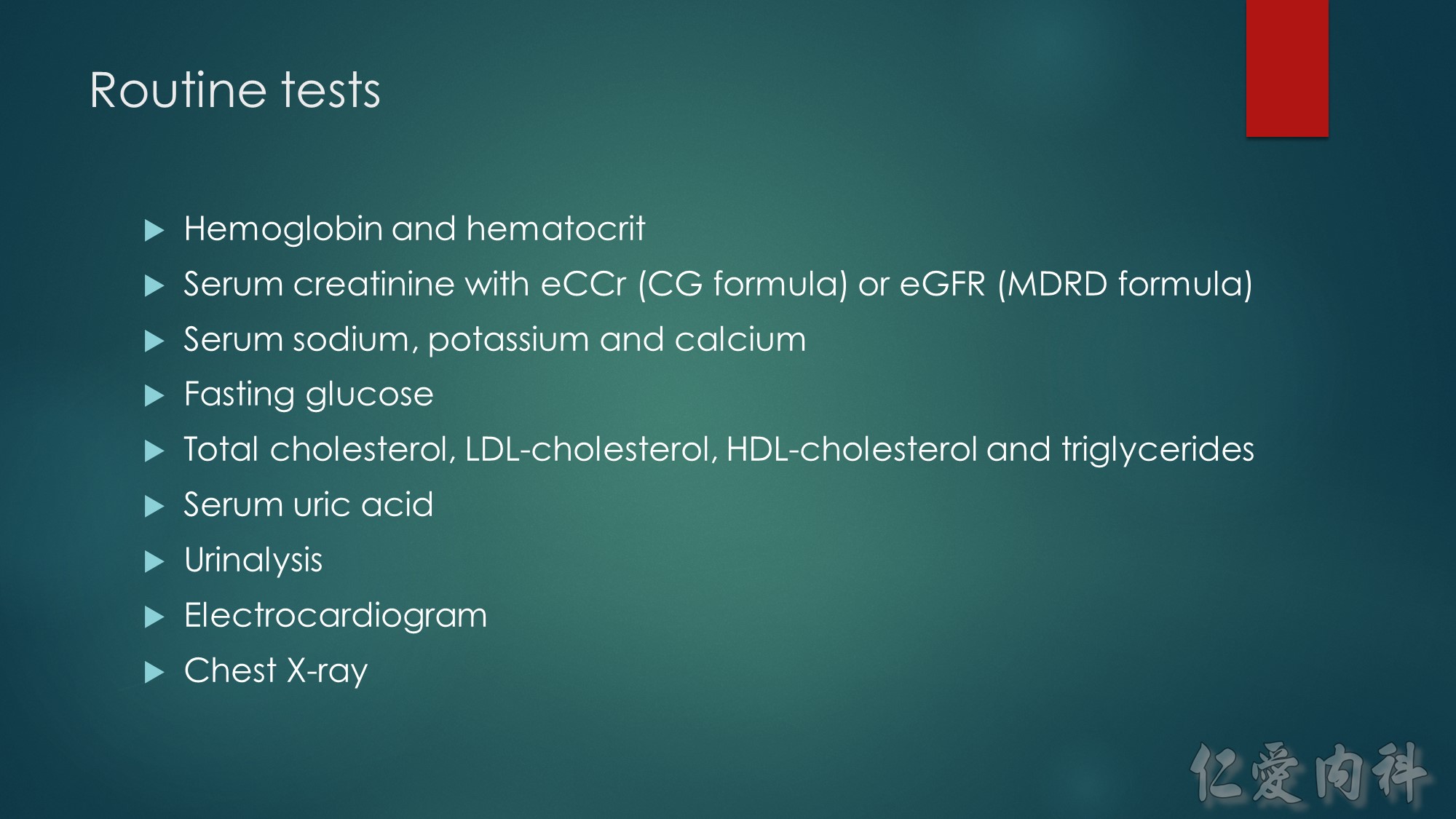
台灣高血壓guideline- routine test
曾有考題選項為renal echo,錯! Renal echo 是當懷疑為 secondary H/T 時才安排做的。
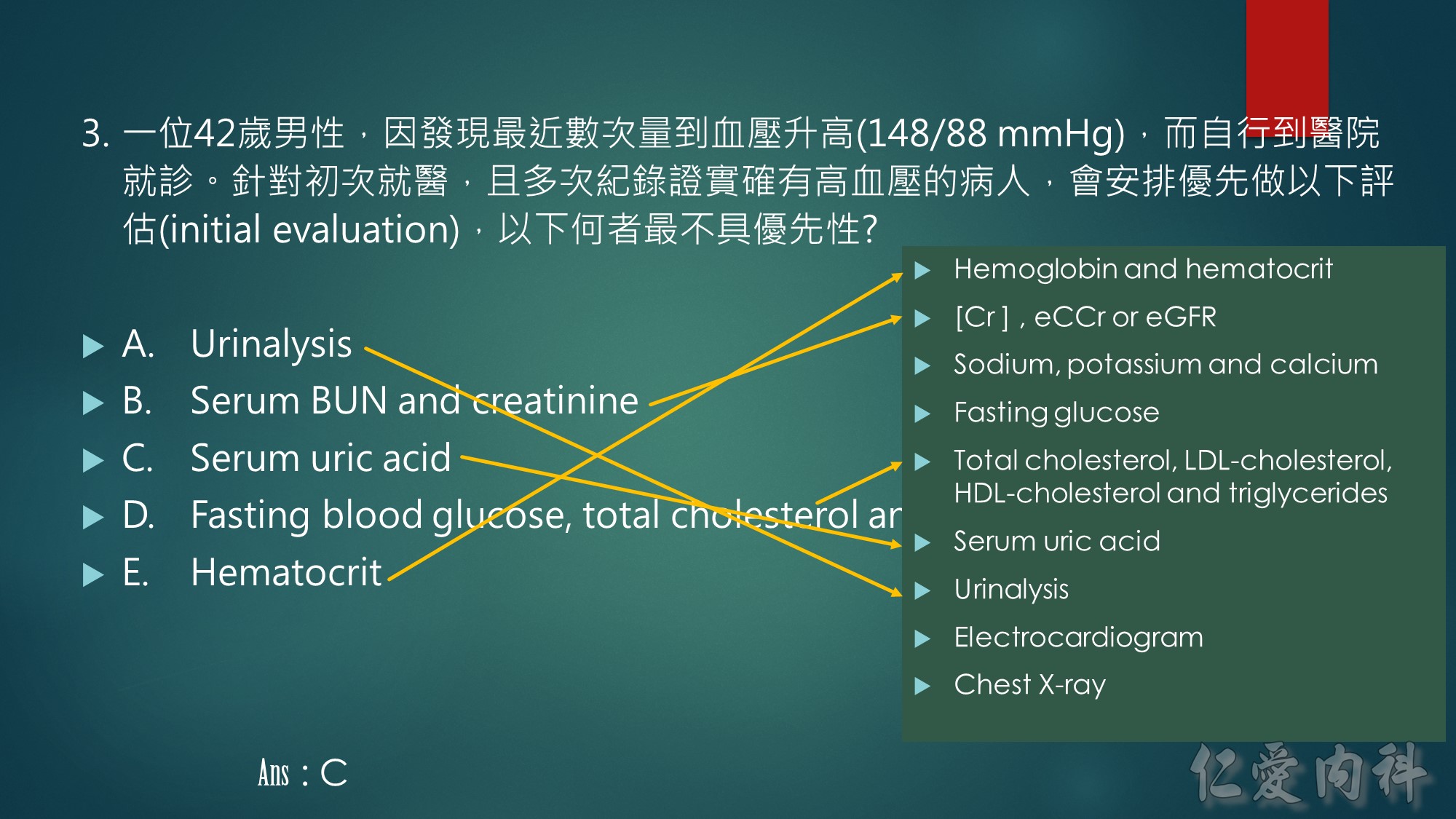
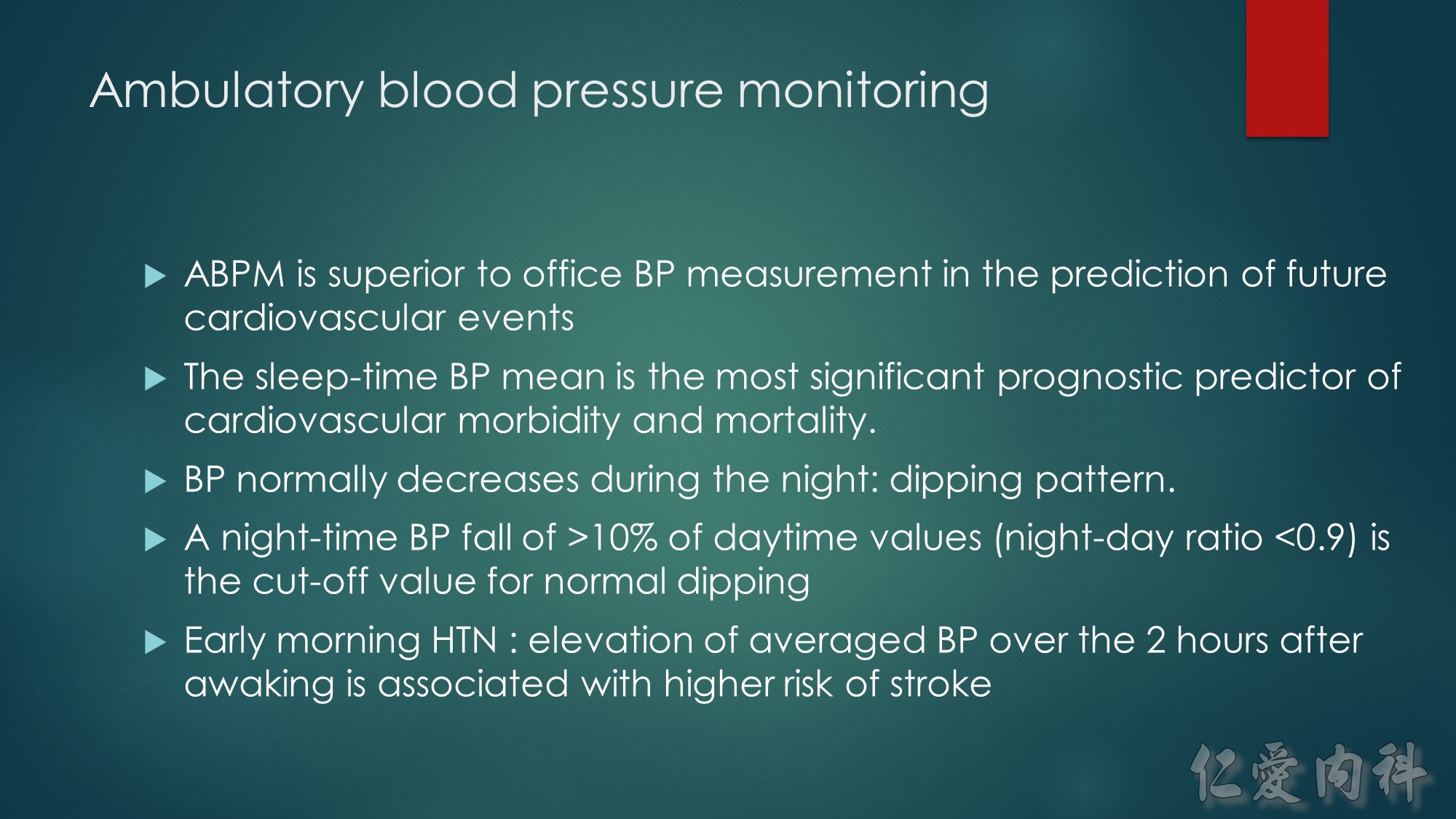
C 因為參考的是ACC guideline(見下頁)
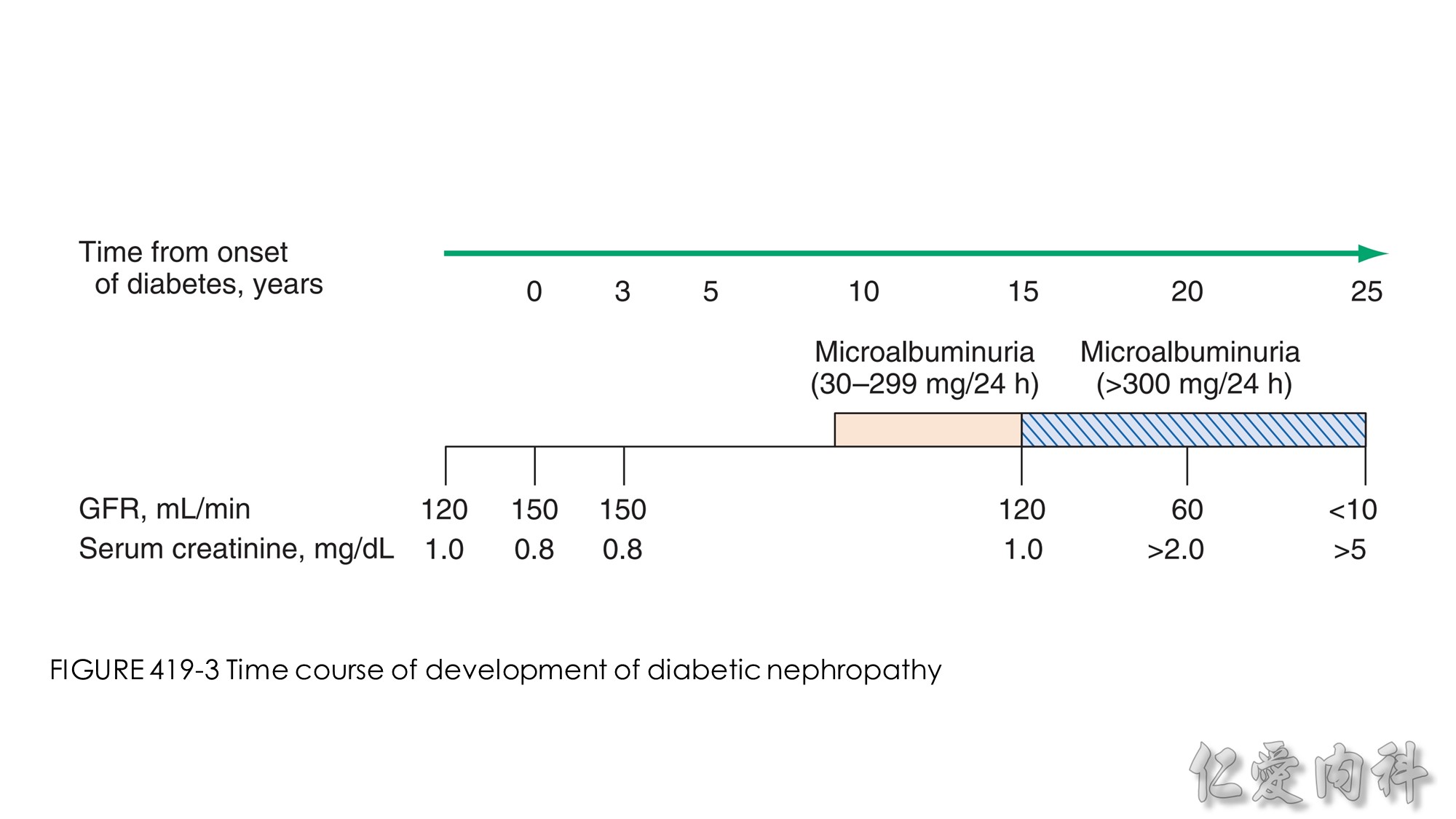
DM glomerulus damage 最早可看到albuminuria,一旦出現albuminuria, CV risk 隨之上升。
抽菸加速DM nephropathy
Type I DM, 一旦有retinopathy,通常也已有nephropathy
Type II DM,就沒有上述強烈相關。
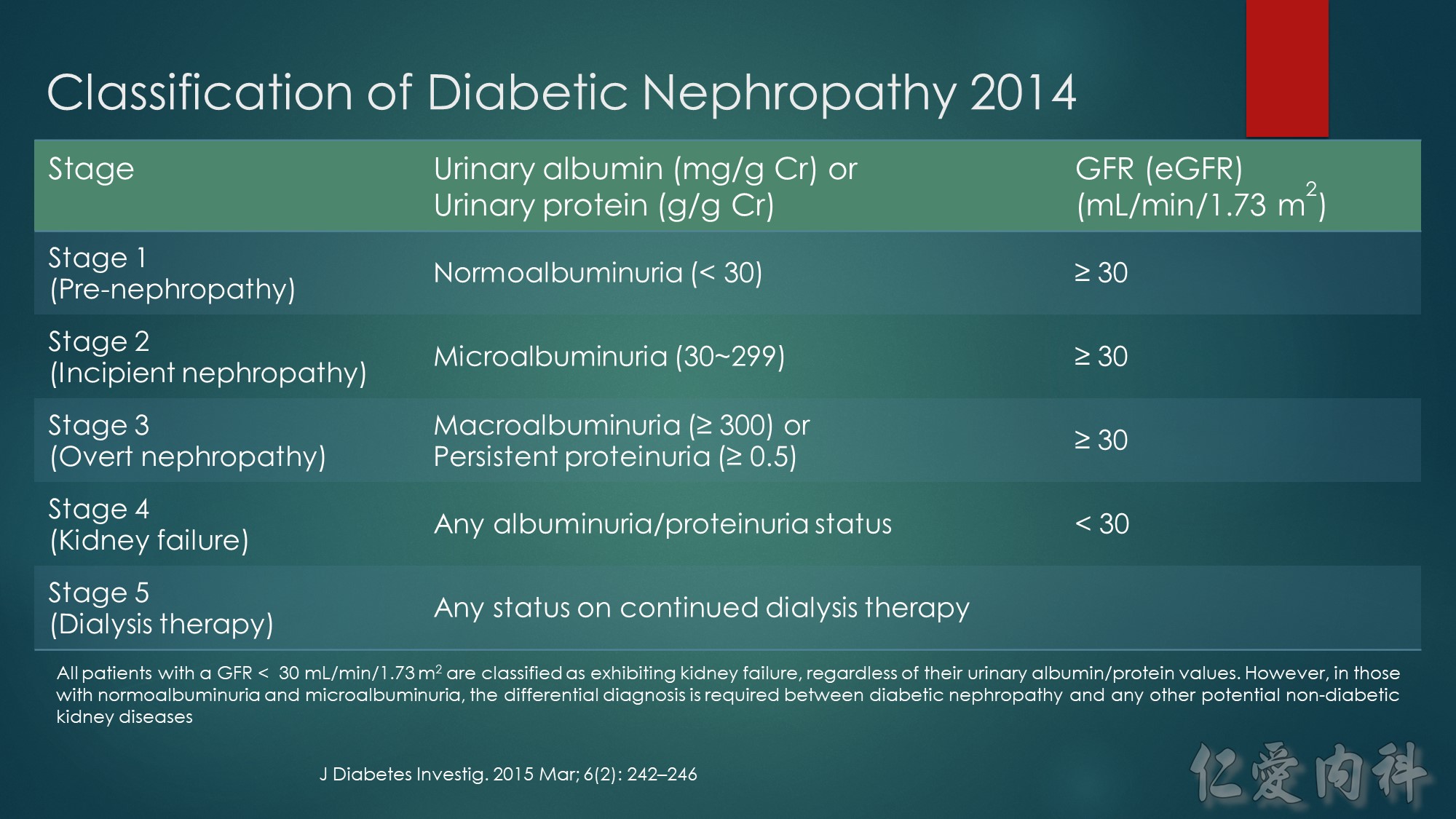
Microalbuminuria 時期, 吃ACEI/ARB, 腎功能還可能逆轉改善。一旦進入macroalbuminuria,就無法逆轉,只能減緩惡化,若無法控制,5-10年後進入洗腎
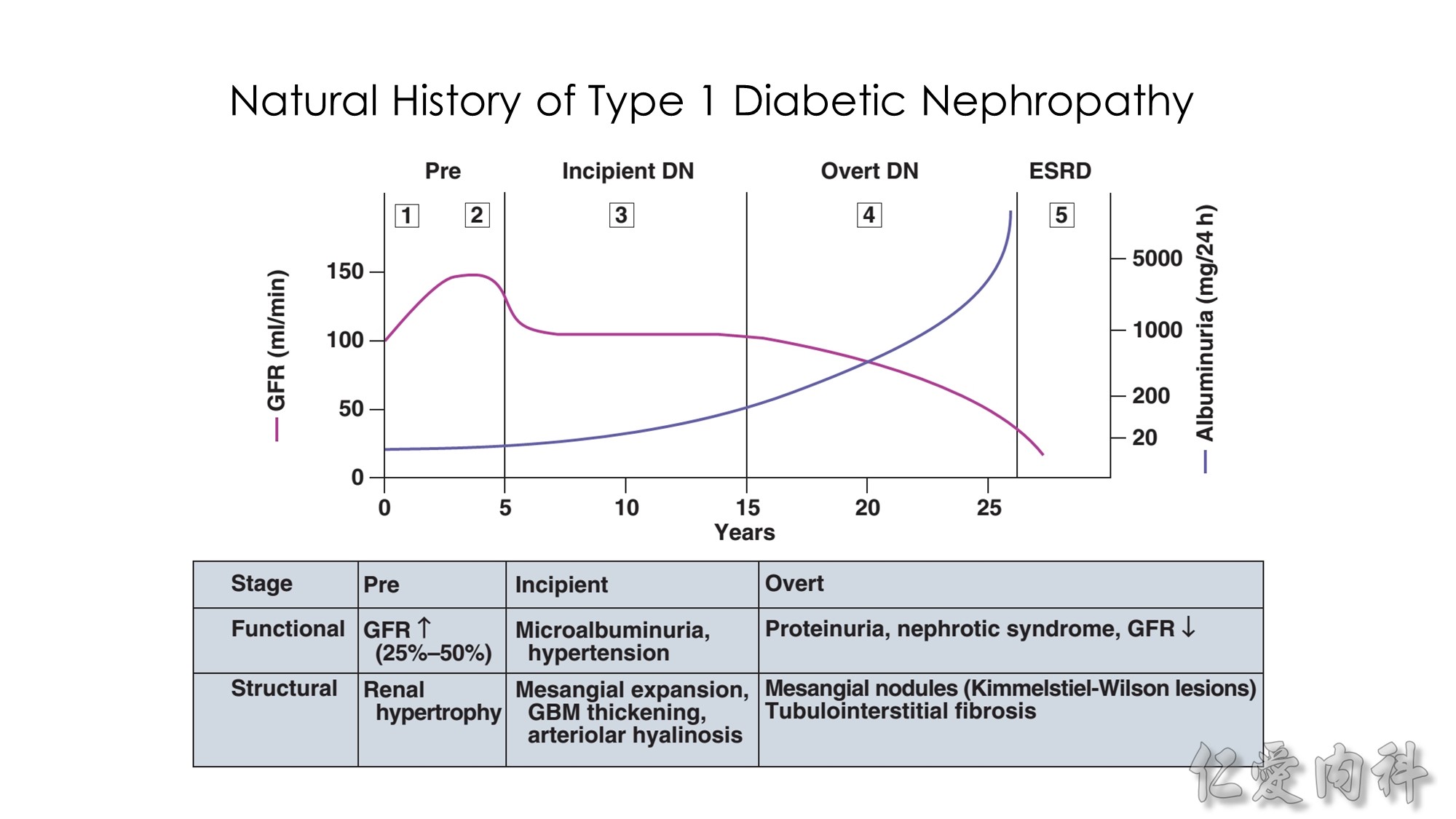
Pre DM nephropathy時腎臟hypertrophy, hyperfiltration,因此DMN的病人如果腎臟已經是跟正常人一樣的大小時,表示已經不是pre DMN,已在進展/變不好的過程中。
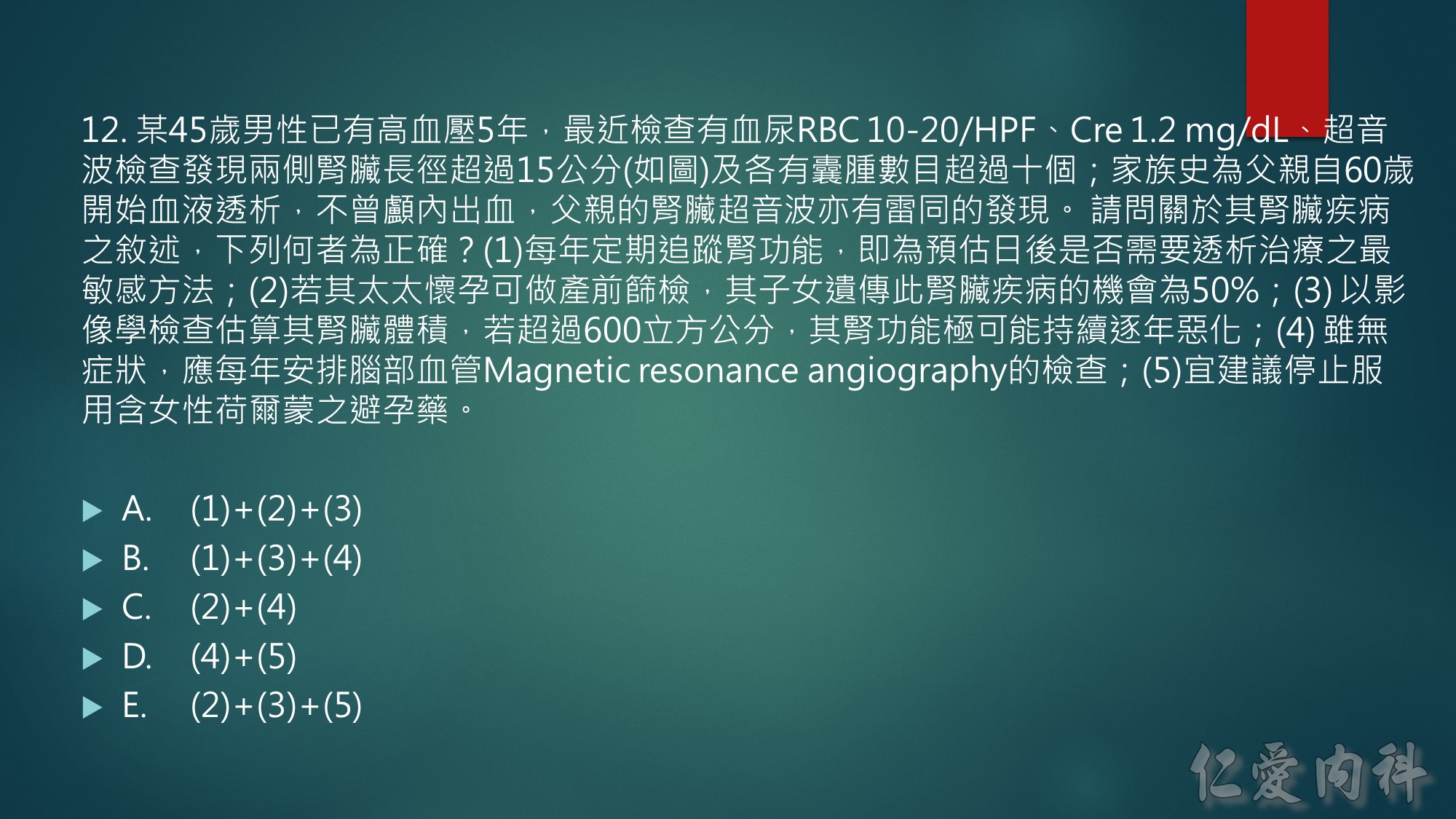
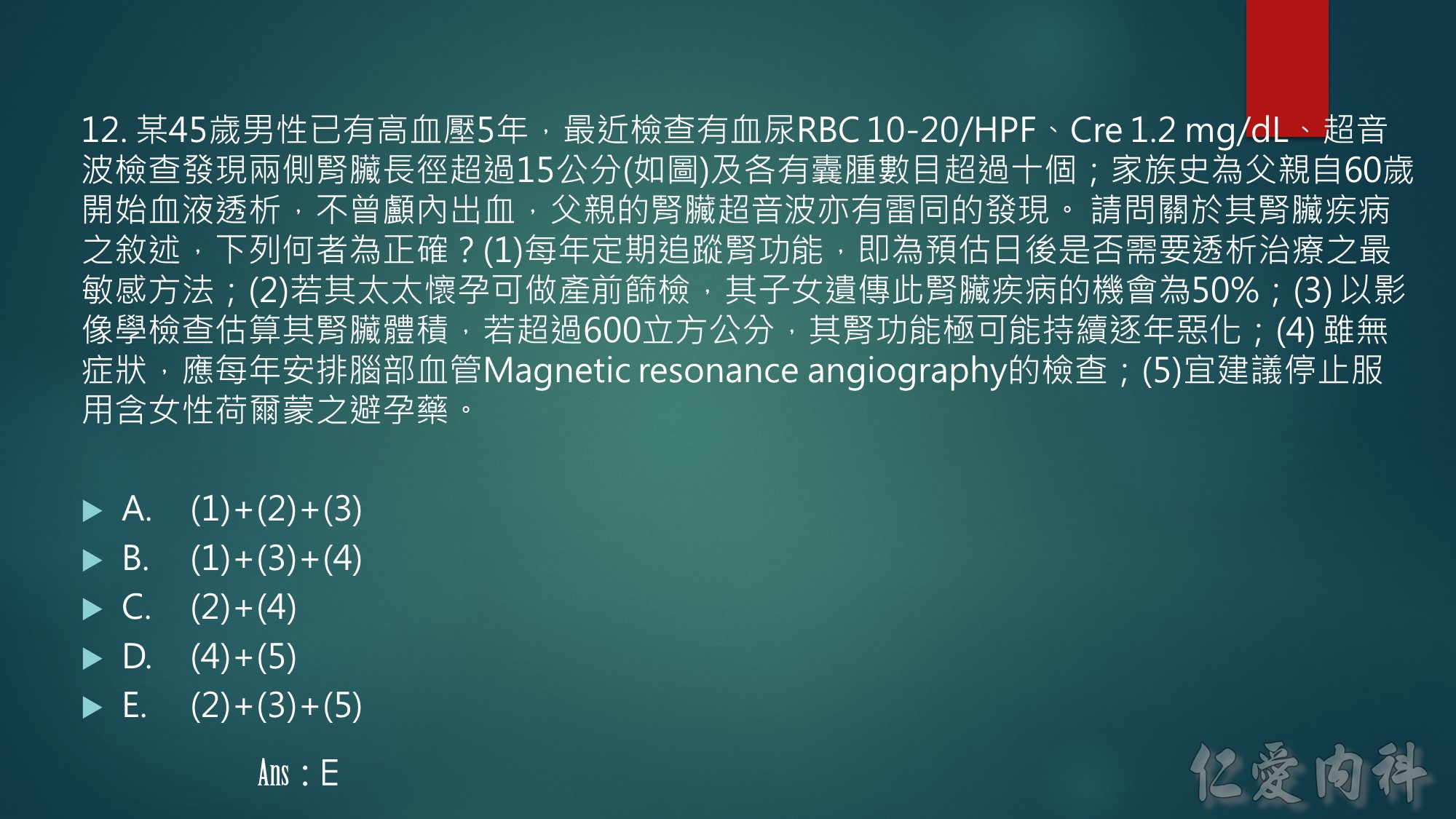
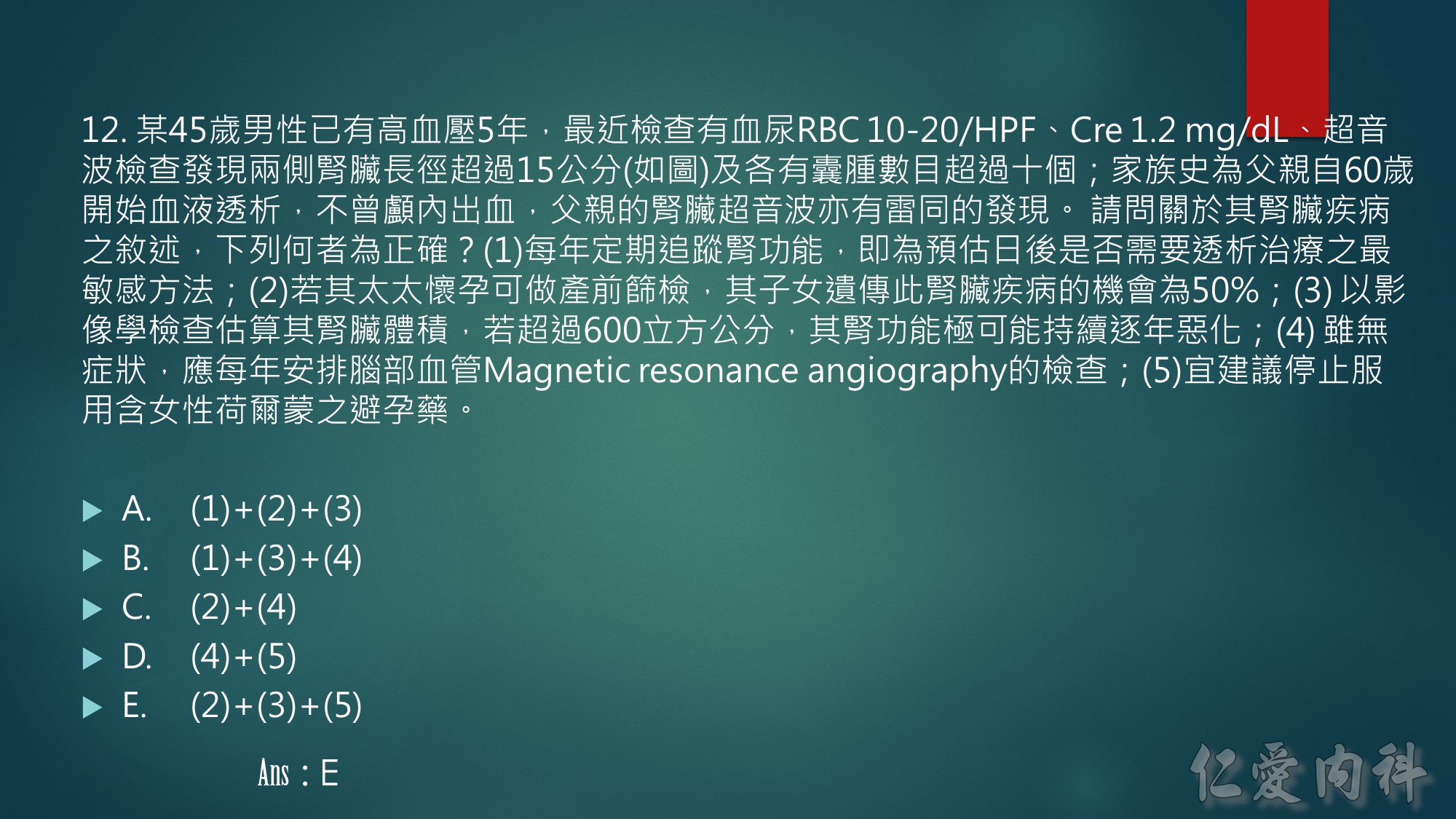
因此若臨床上腎功能不好但腎臟大小正常時,要考慮 DMN、多囊腎、hydronephrosis
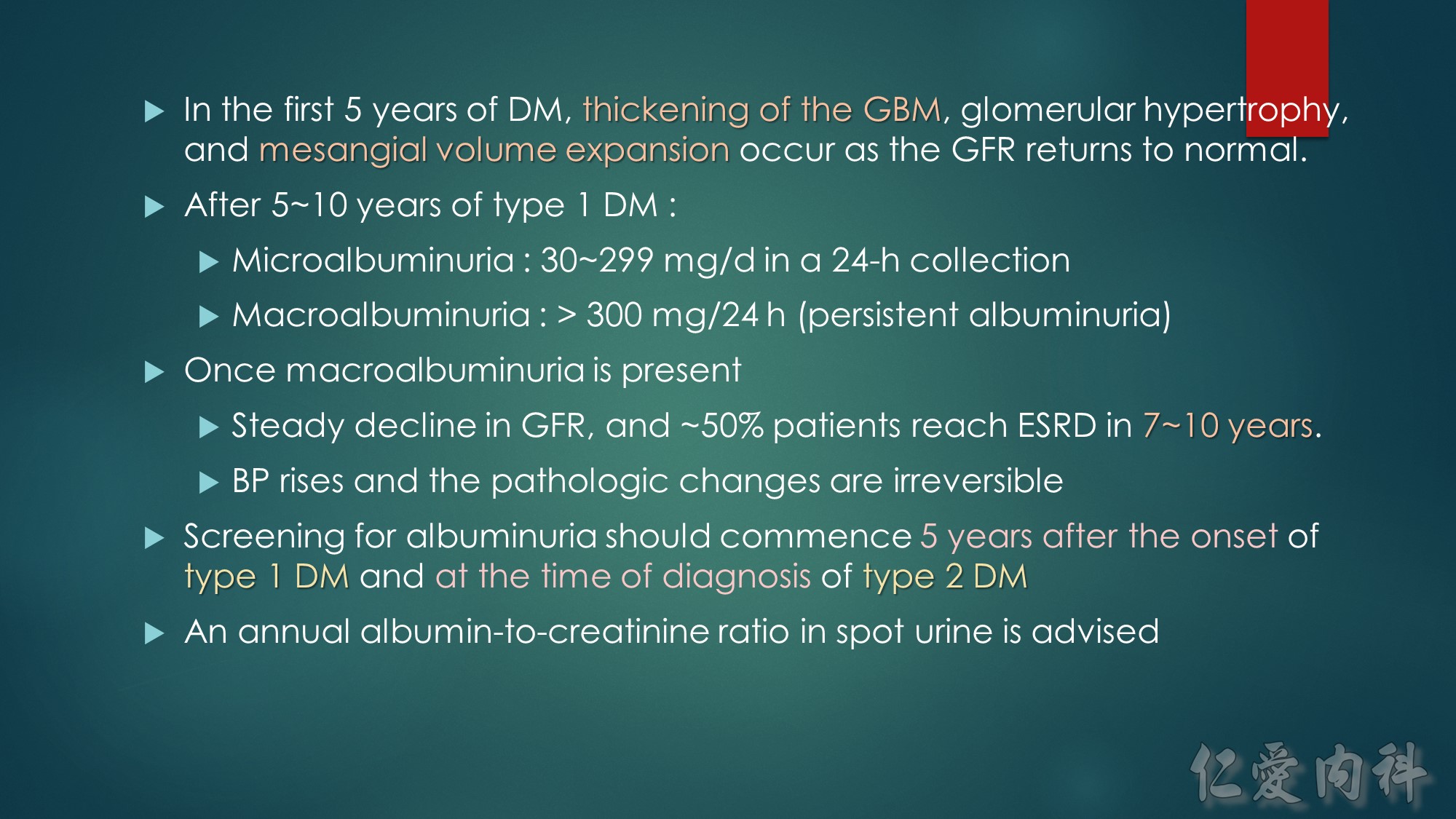
開始驗尿蛋白的時機: T1DM診斷五年後、T2DM初診斷時(因為不知道之前已經多久了)
每年至少驗一次ACR
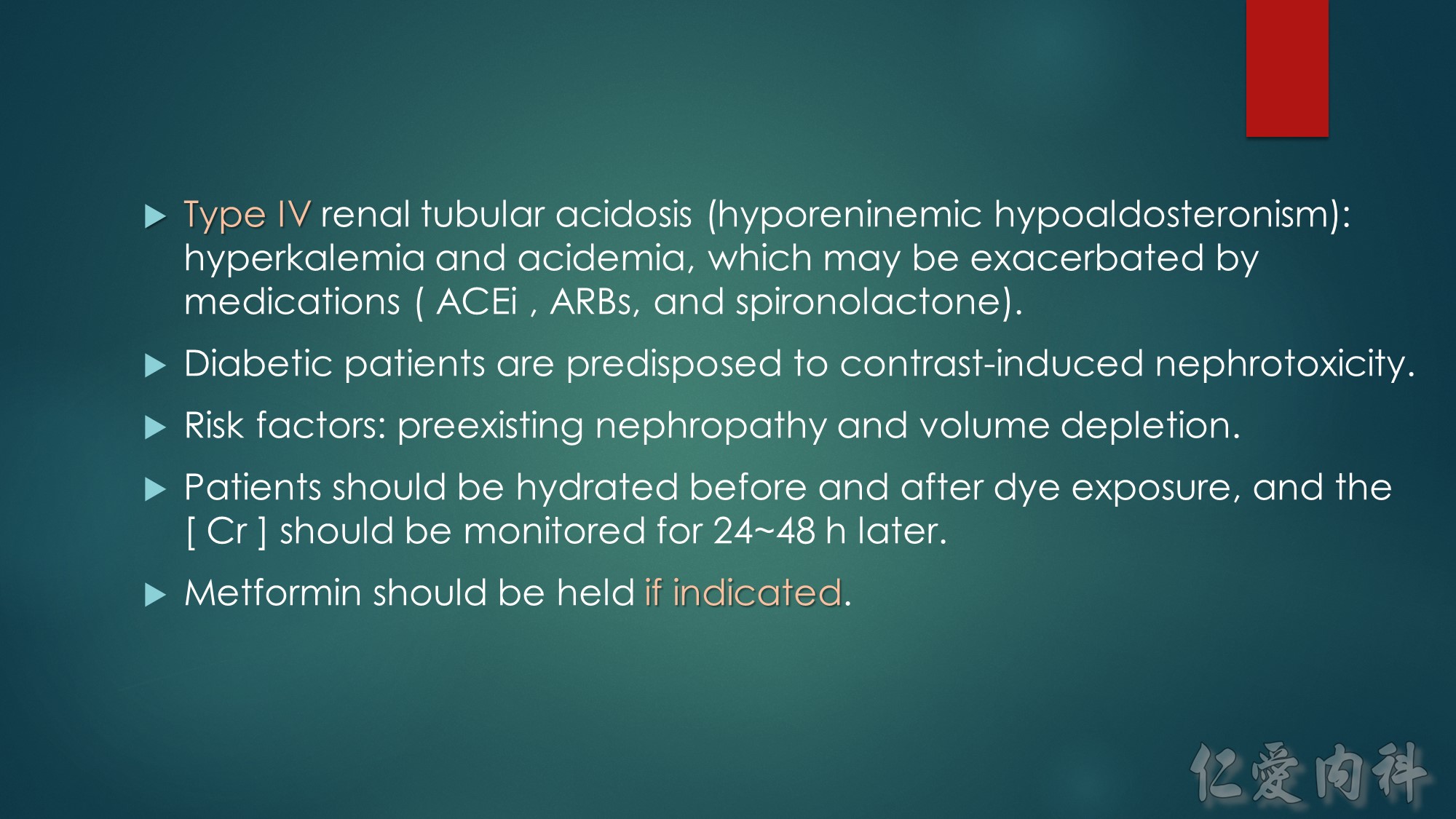
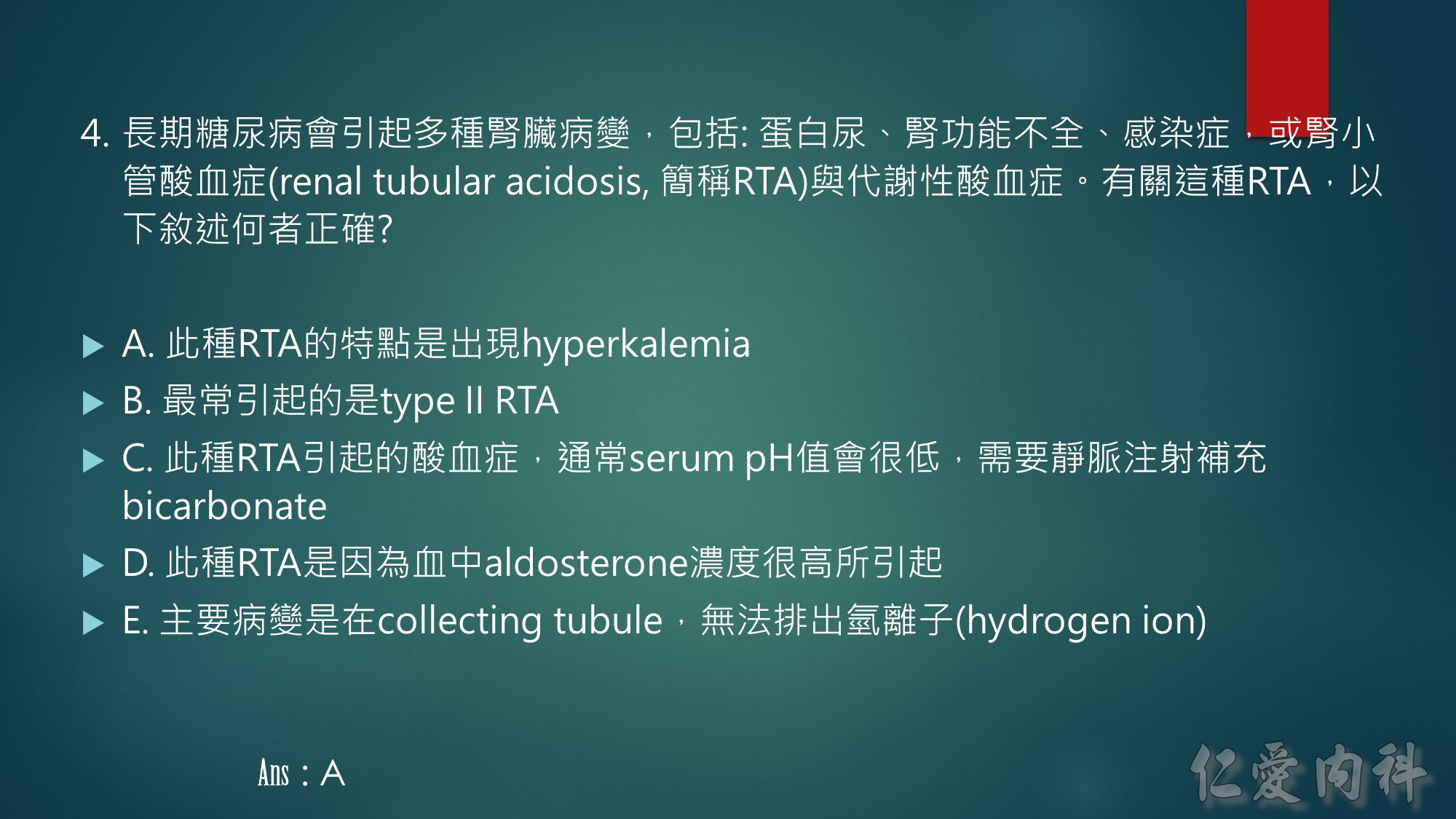
* DMN會造成Type 4 RTA,因為腎絲球有問題所以無法製造renin→hypo-renin, hypo-aldosteronism,無法吸Na、排K、排H,此時若使用ACEI/ARB會使情況加劇。
* DM病人也容易 contrast induced nephropathy,risk factor為本來就有nepropathy 或 volume depletion。預防方法為hydration,並記得monitor cr level (24~48 hr),Hold metformin。
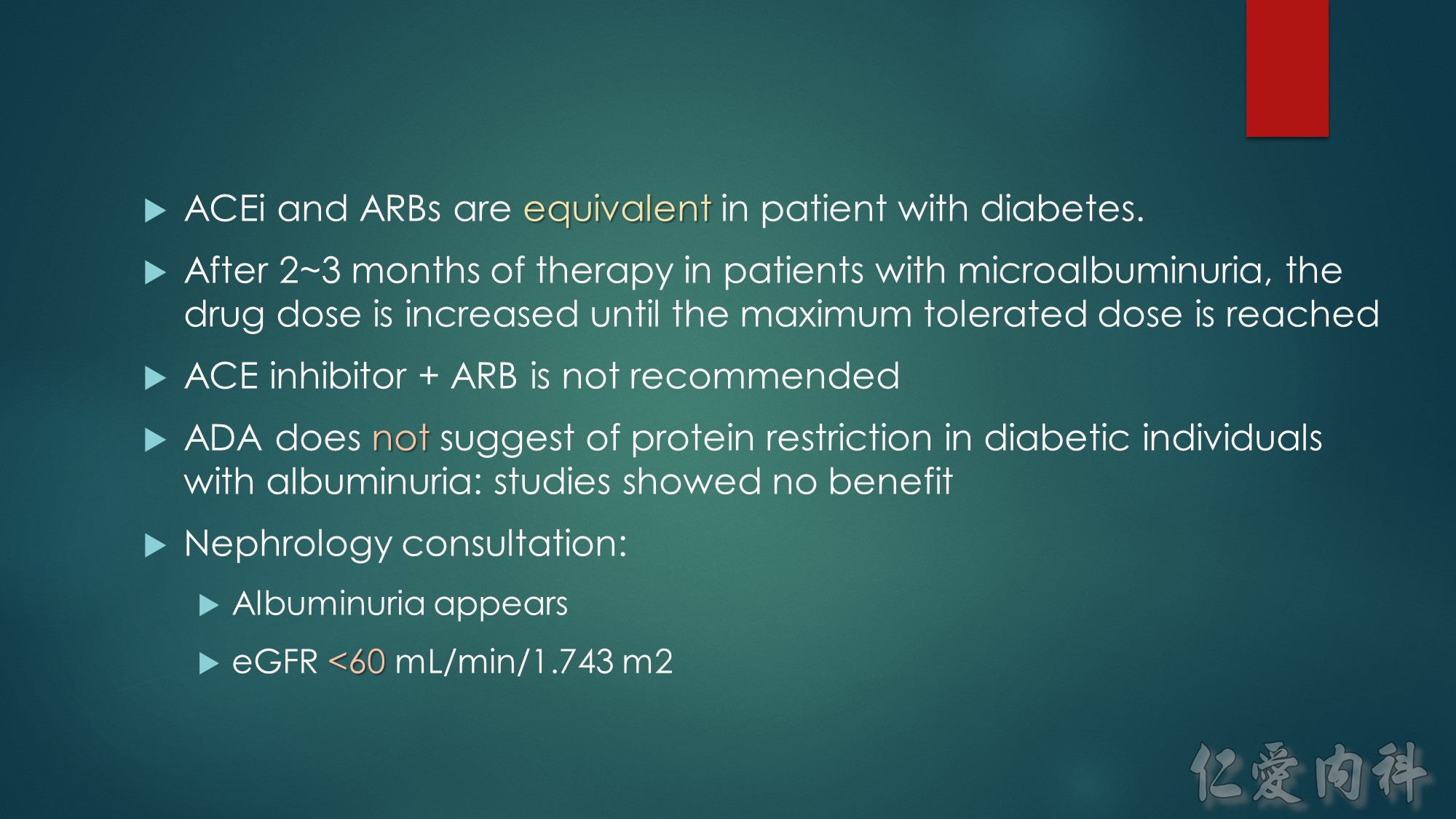
對DM病人來說ACEI跟ARB其實是一樣的,只是ARB是不會咳嗽的ACEI。
但不建議combine 使用兩者。
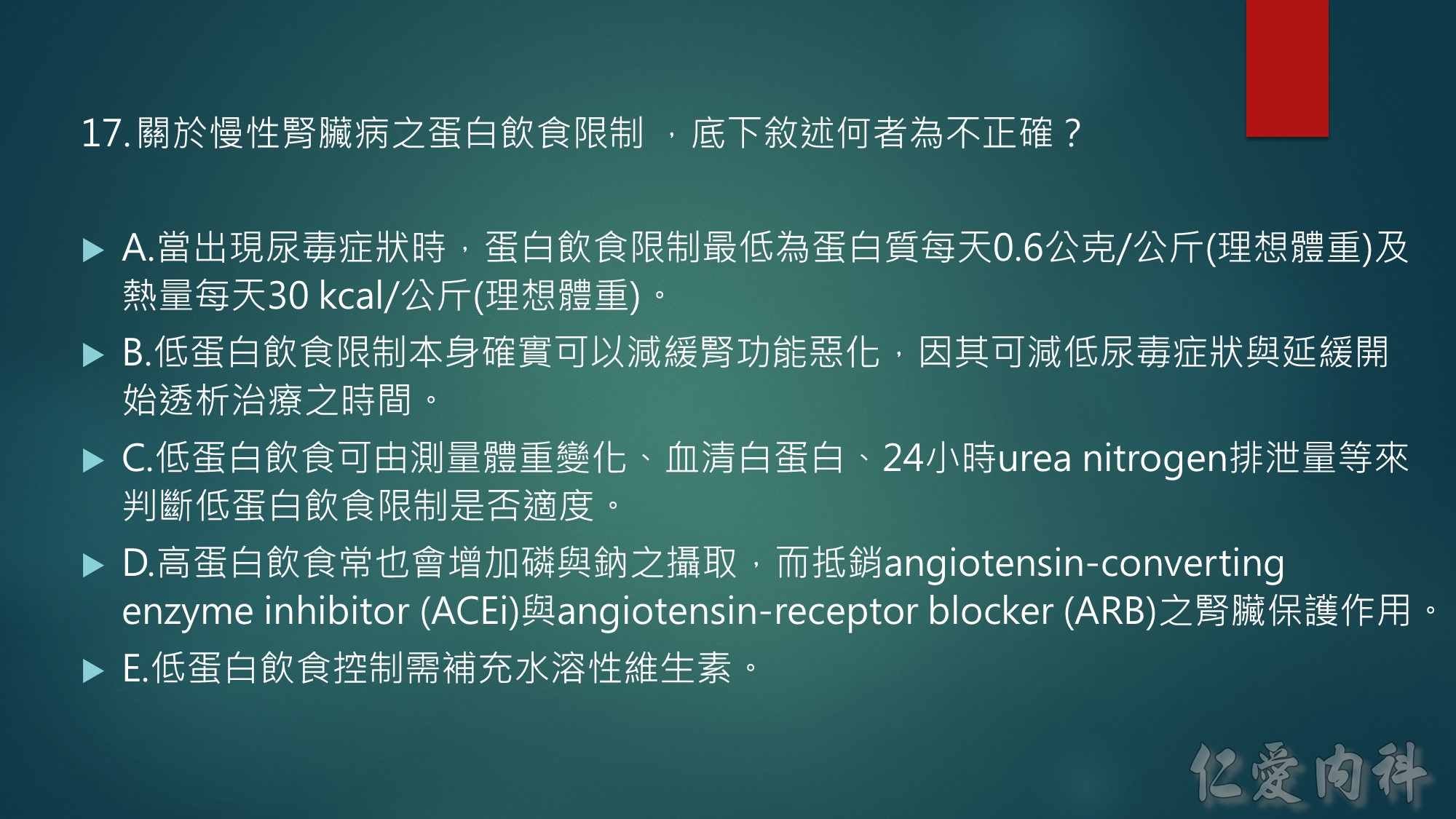
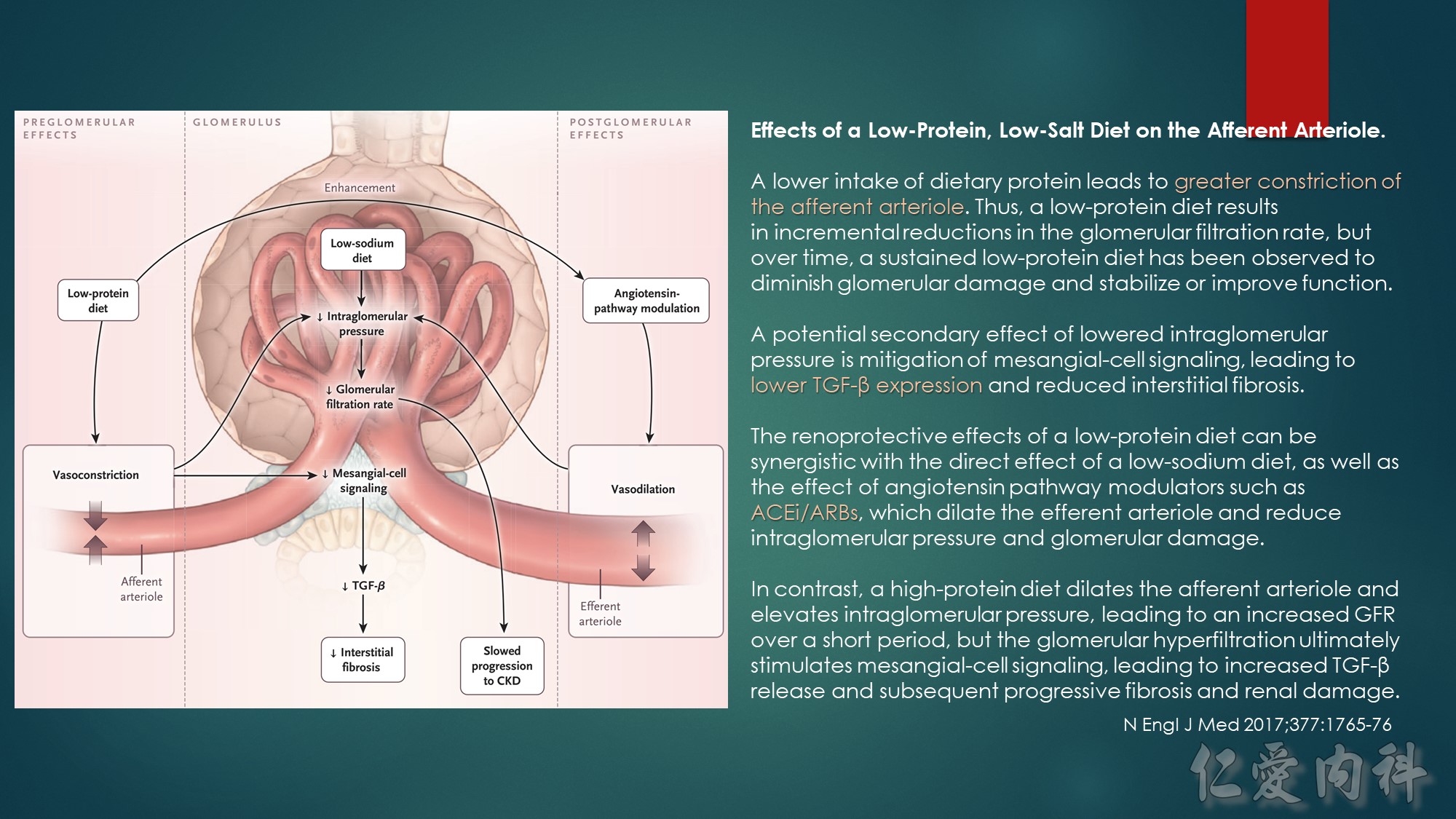
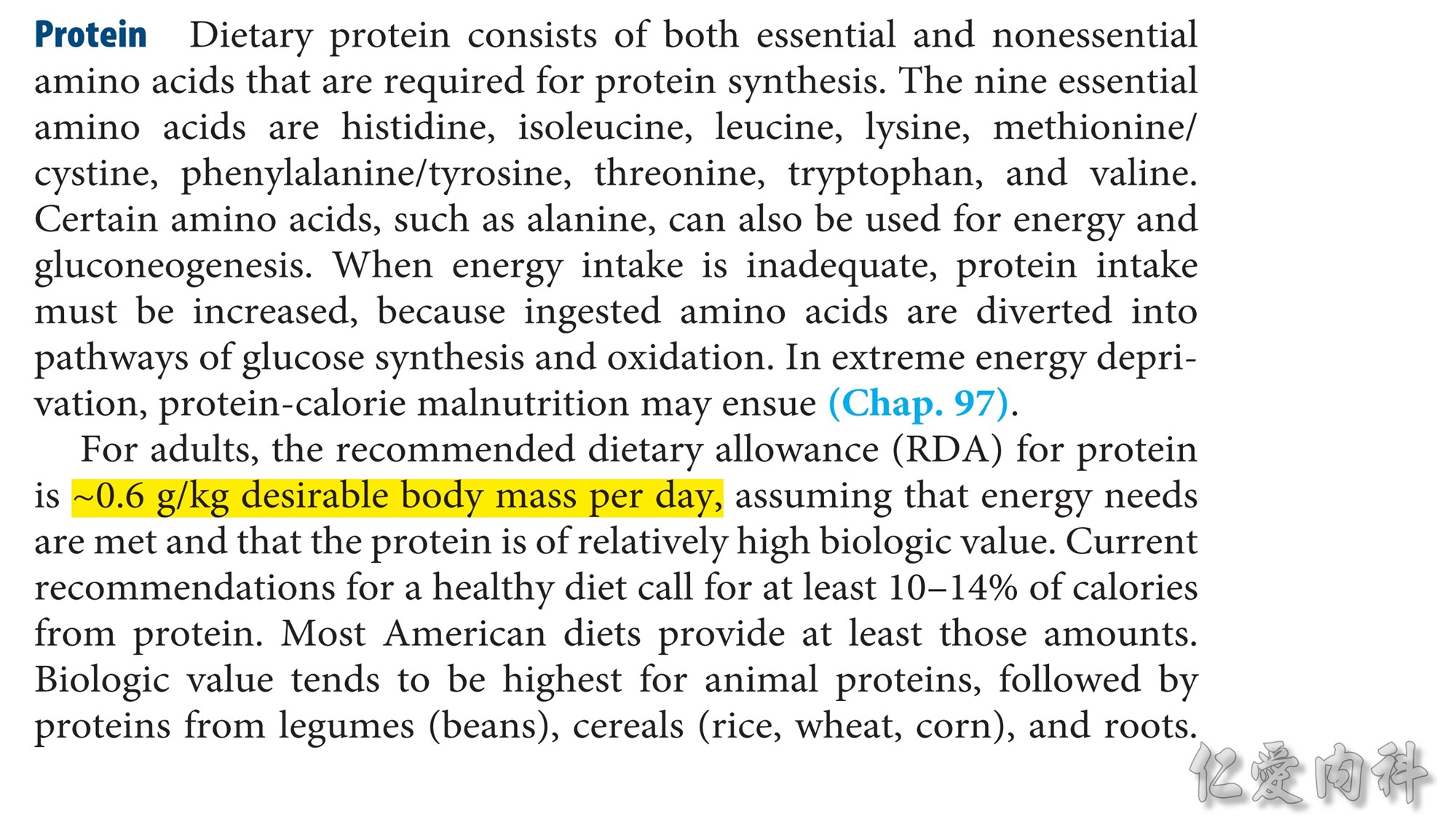
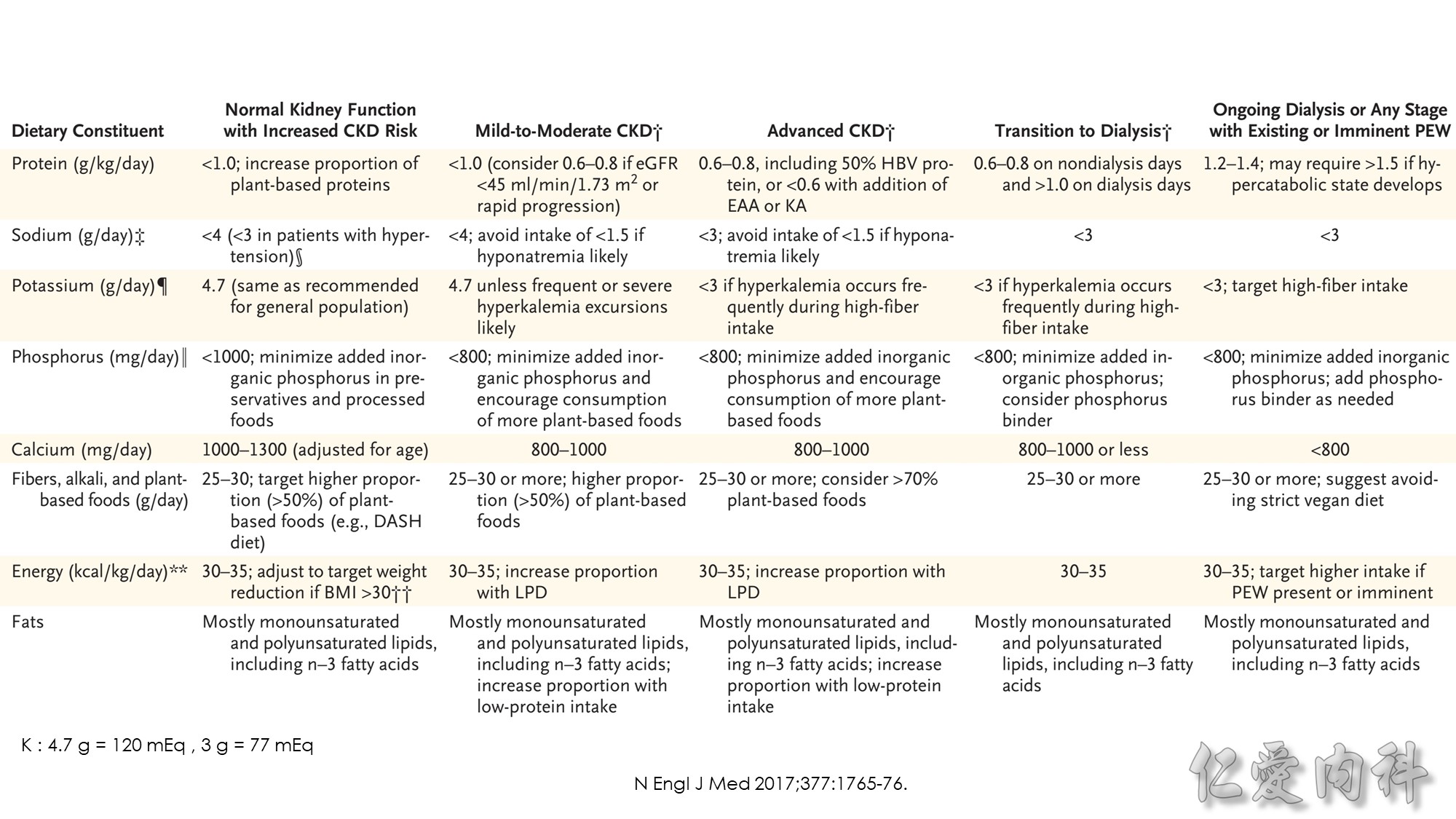
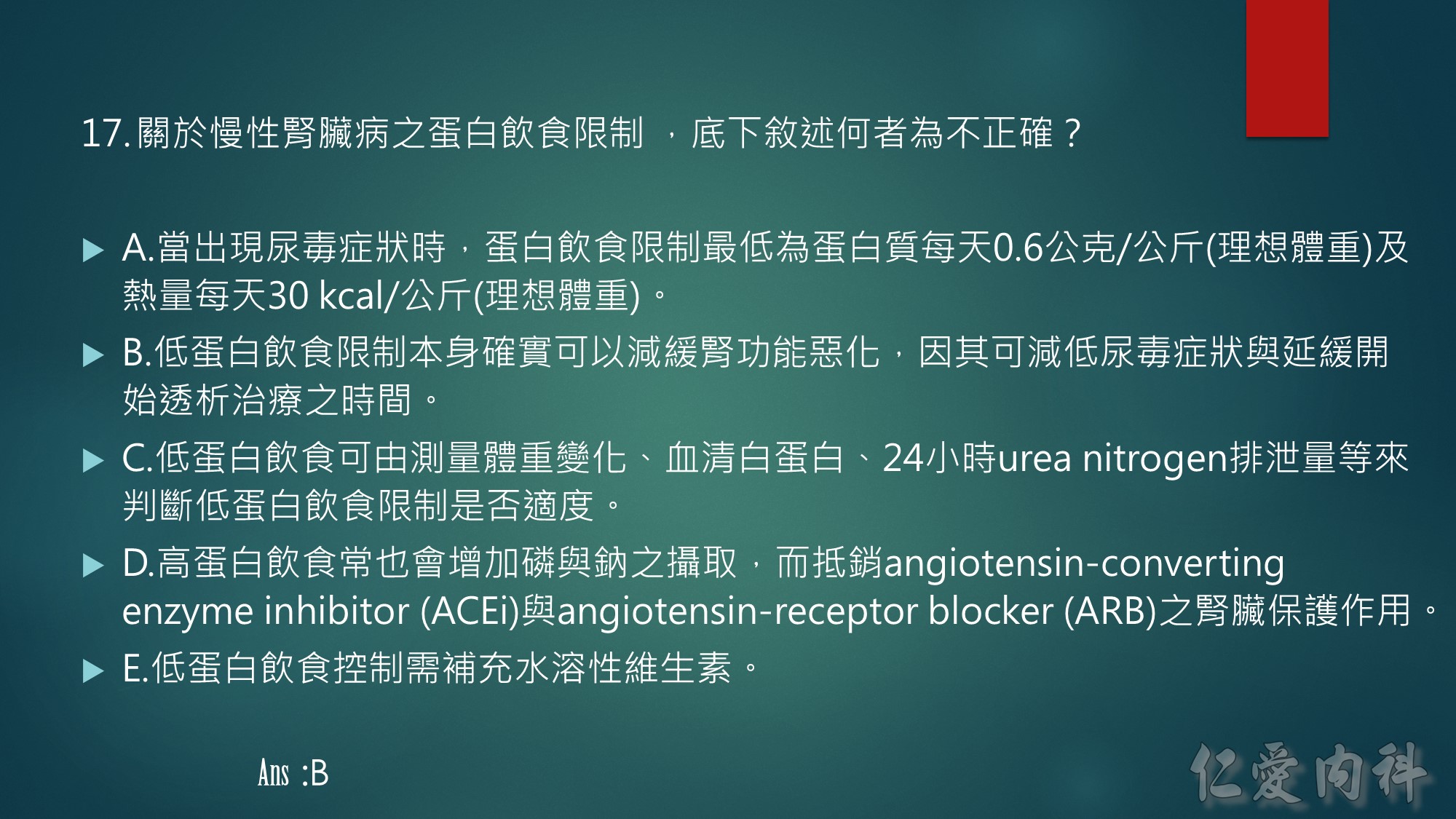
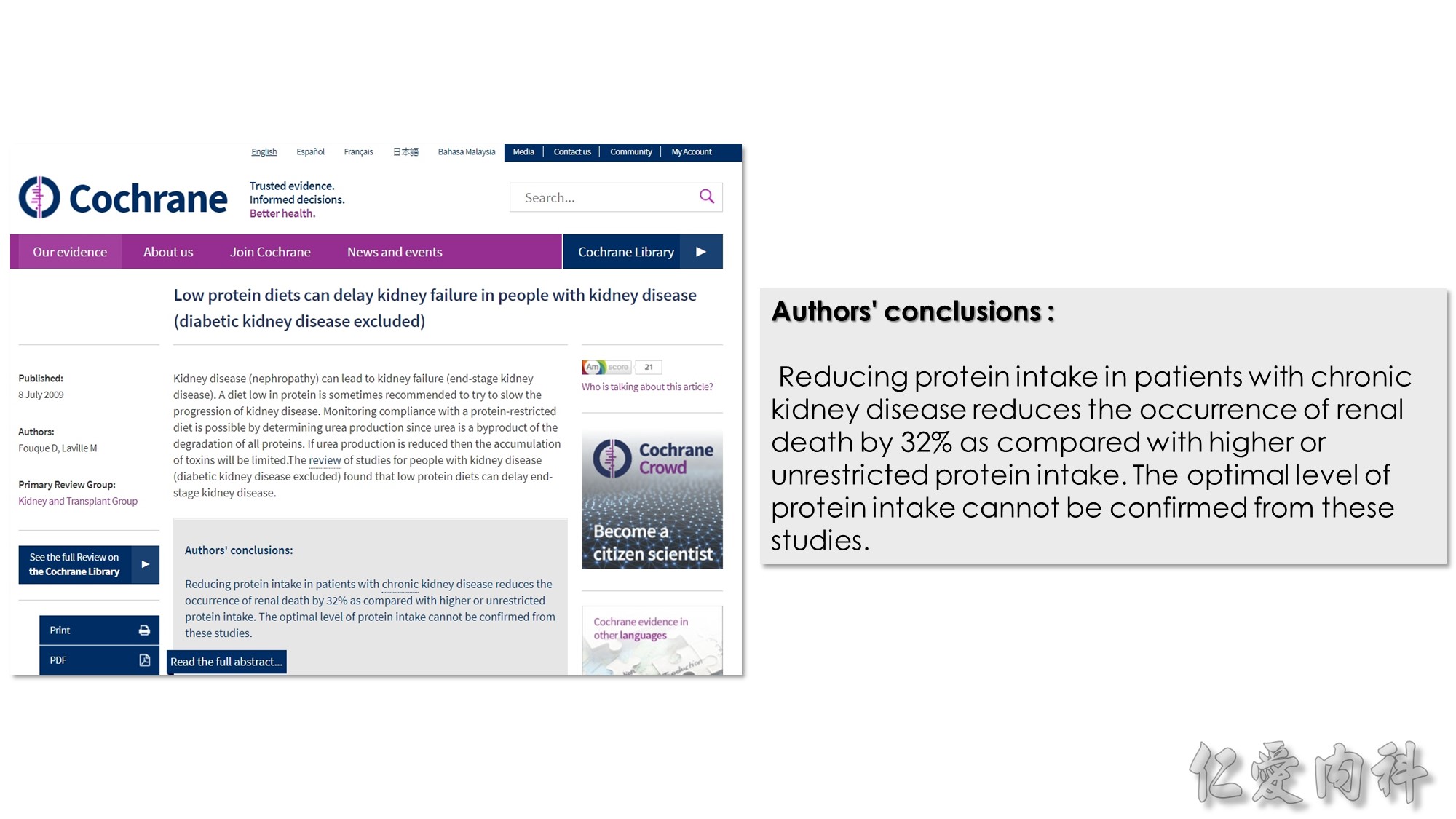
DMN的病人不需要限蛋白!!!
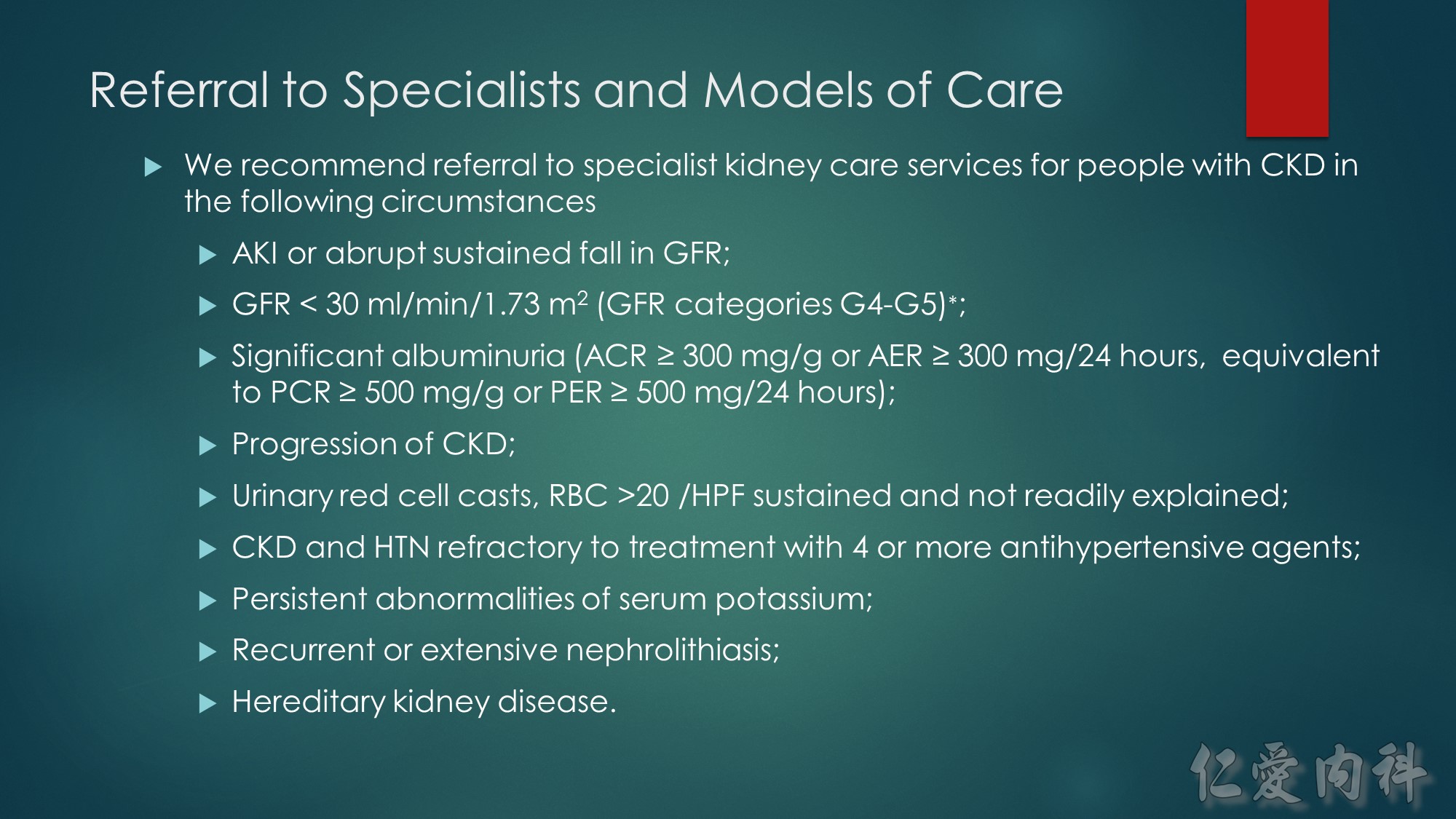
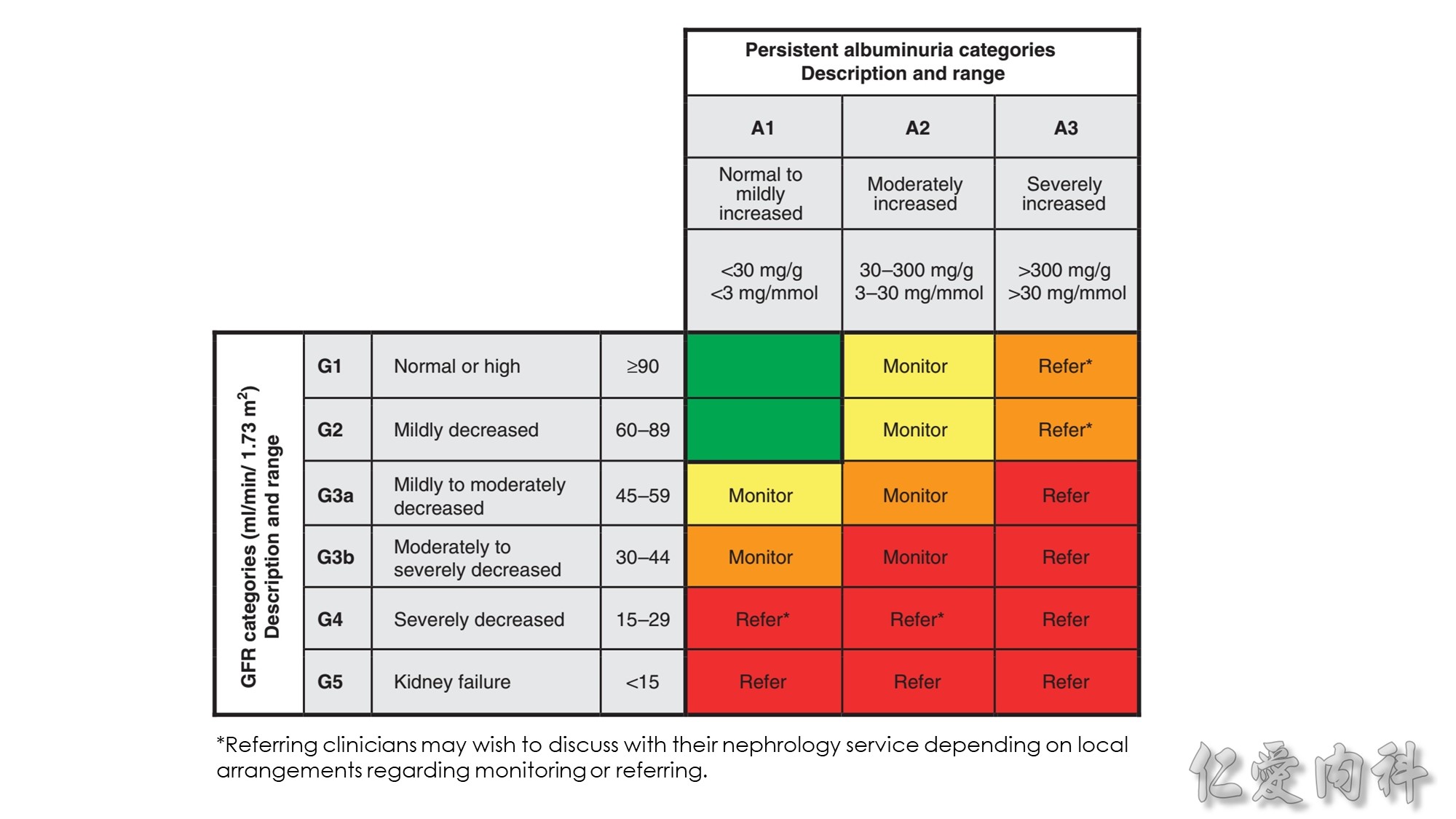
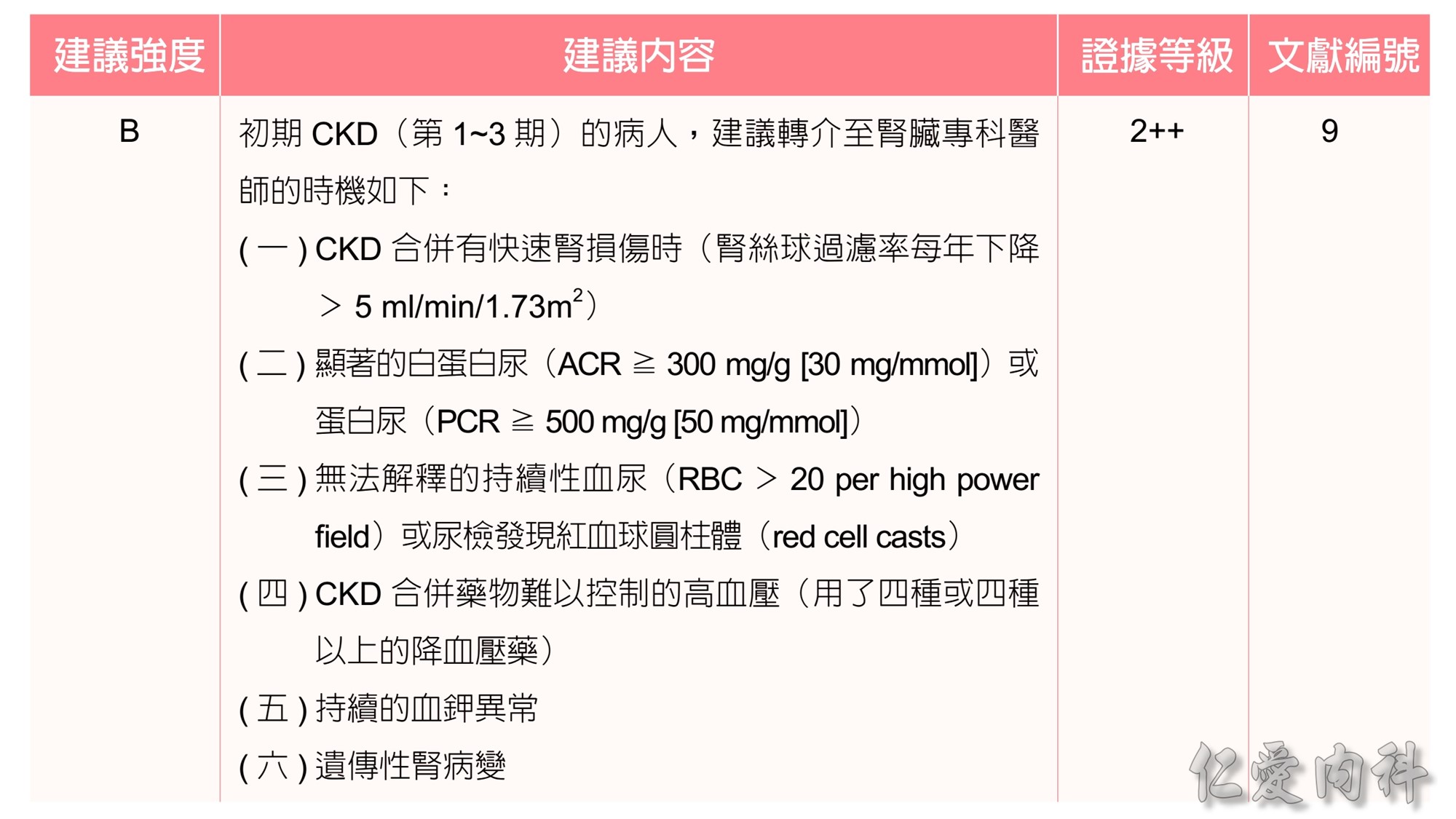
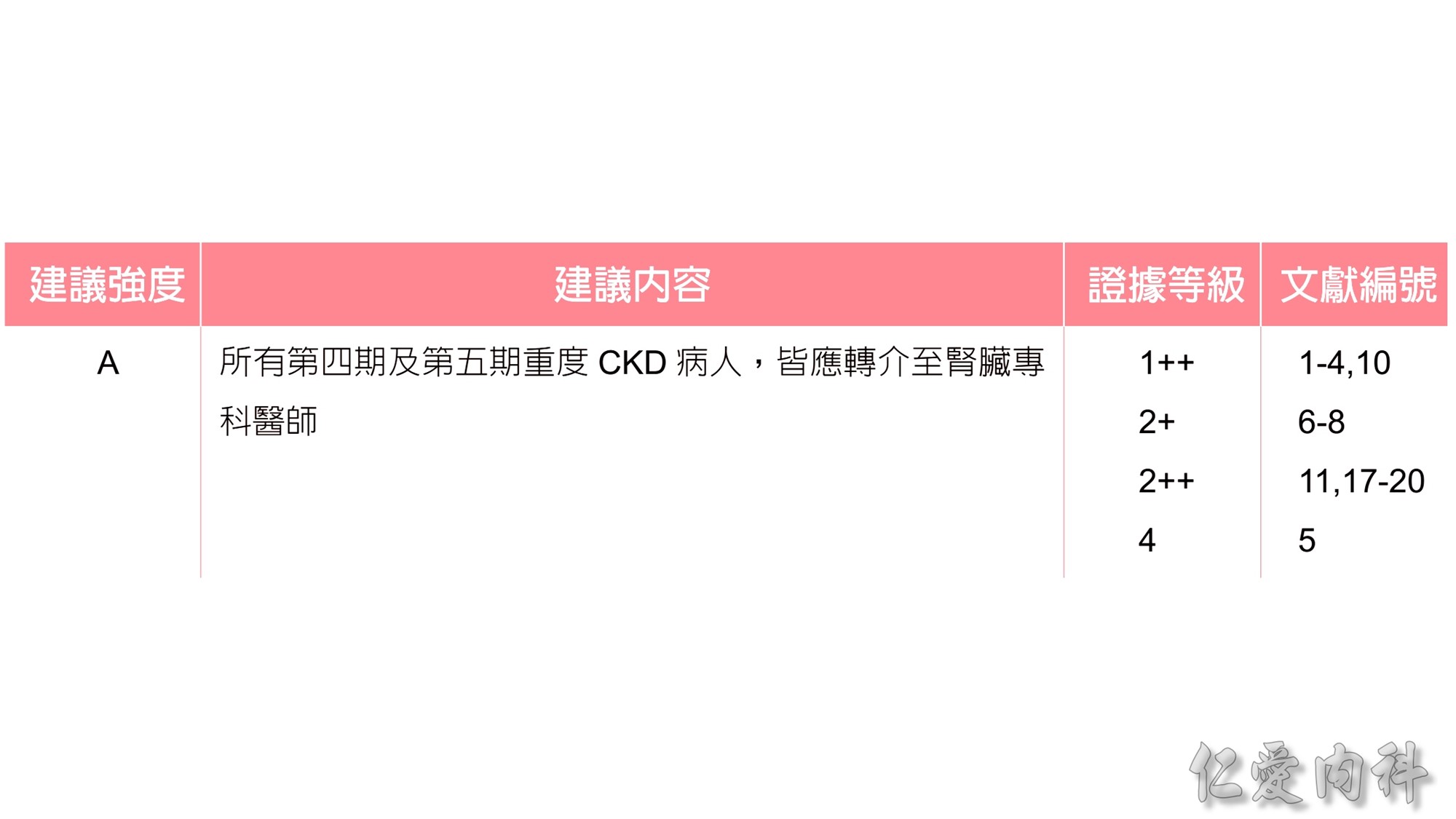
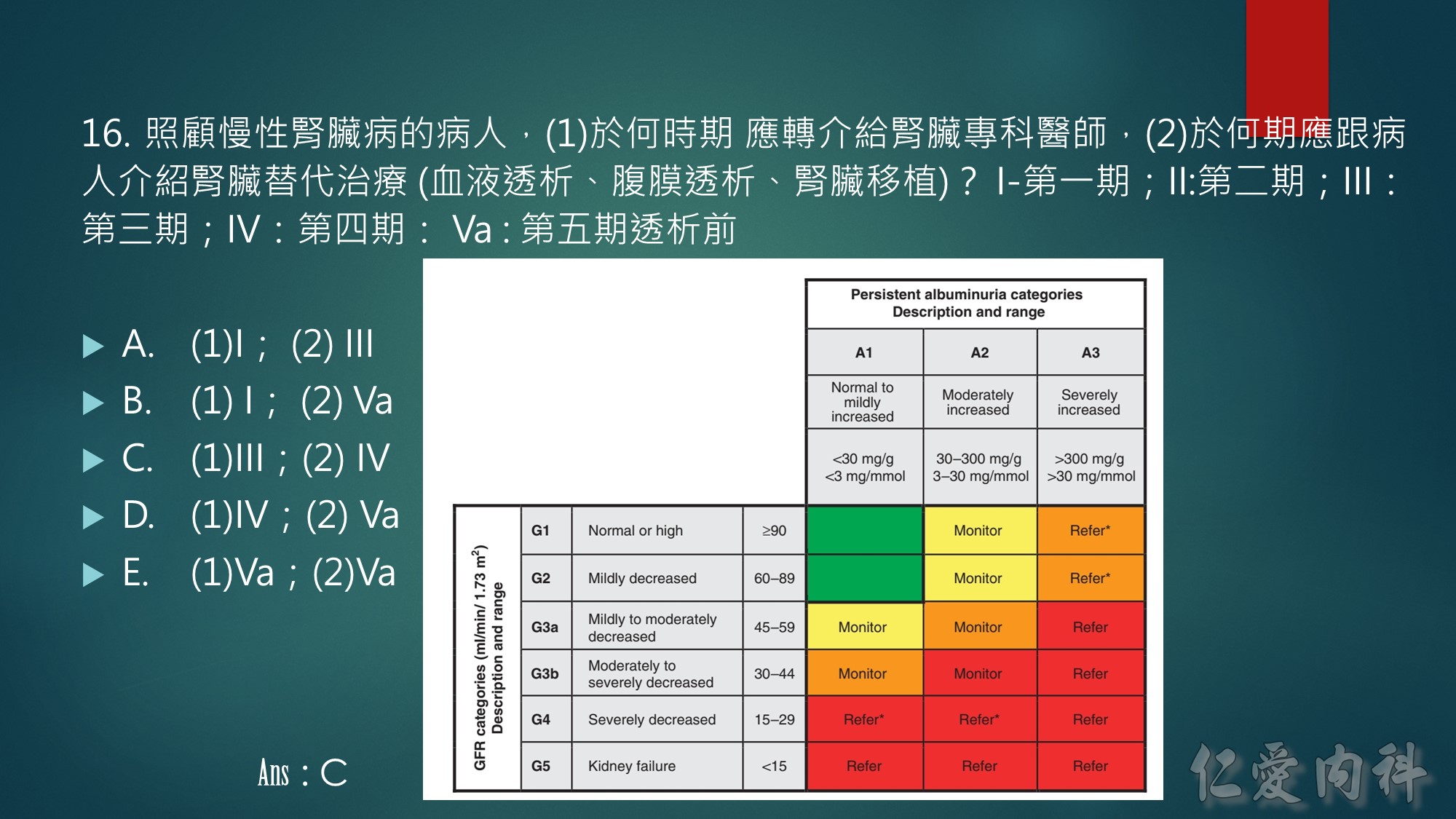
會診腎臟科的時機: 尿蛋白出現時、eGFR<60
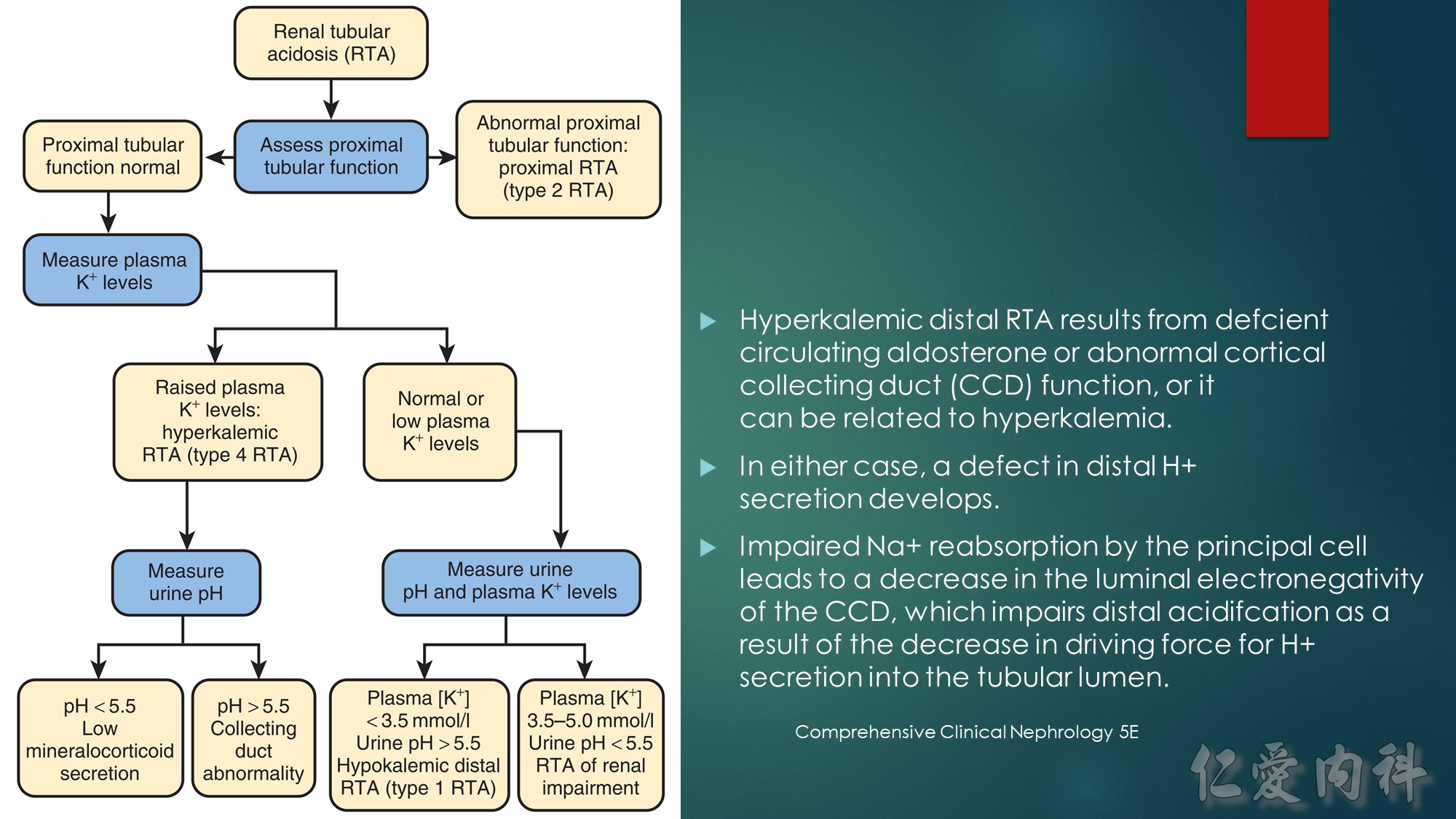
除了type 4之外的RTA都是低血鉀、僅type 4為高血鉀。
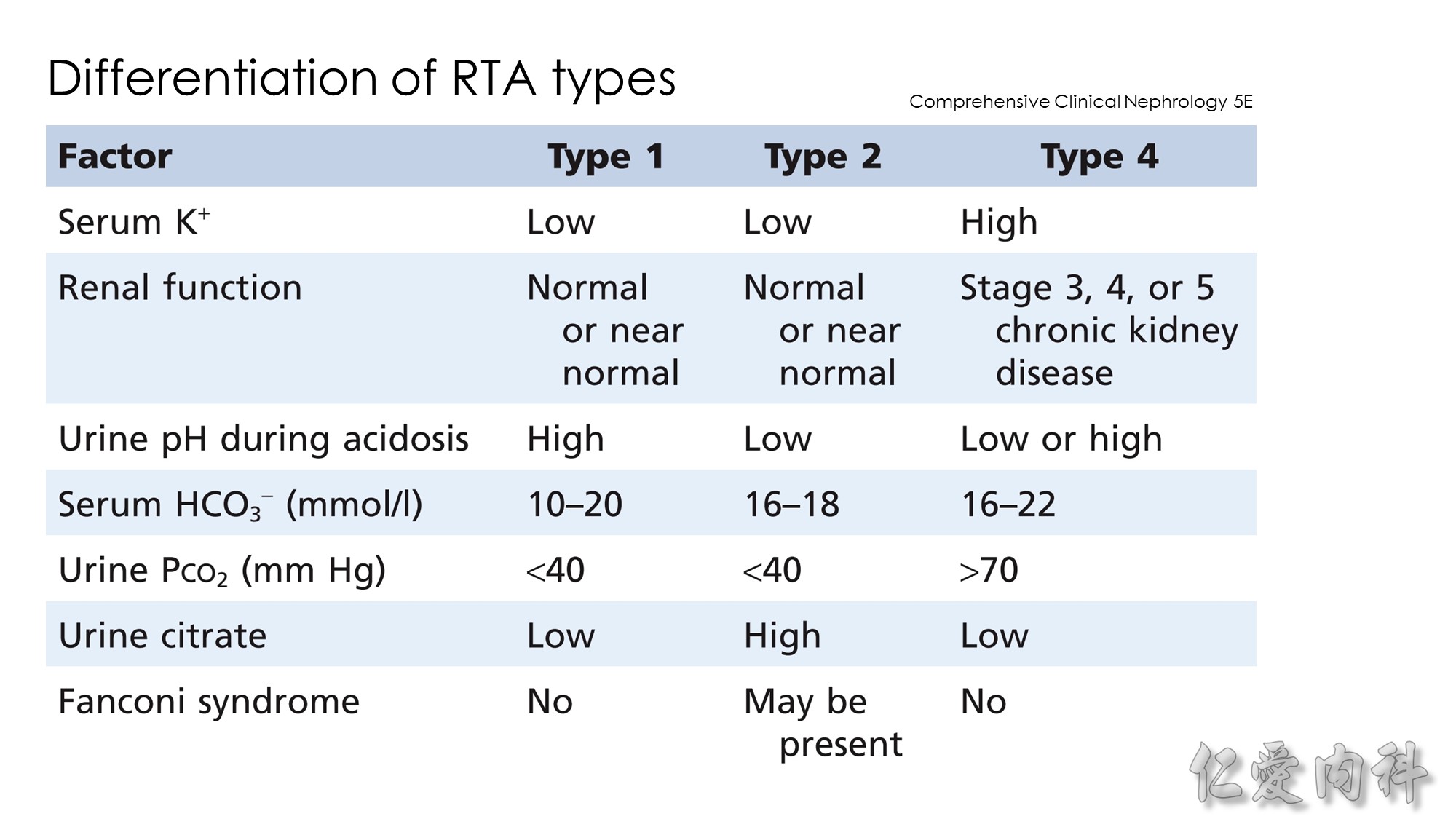
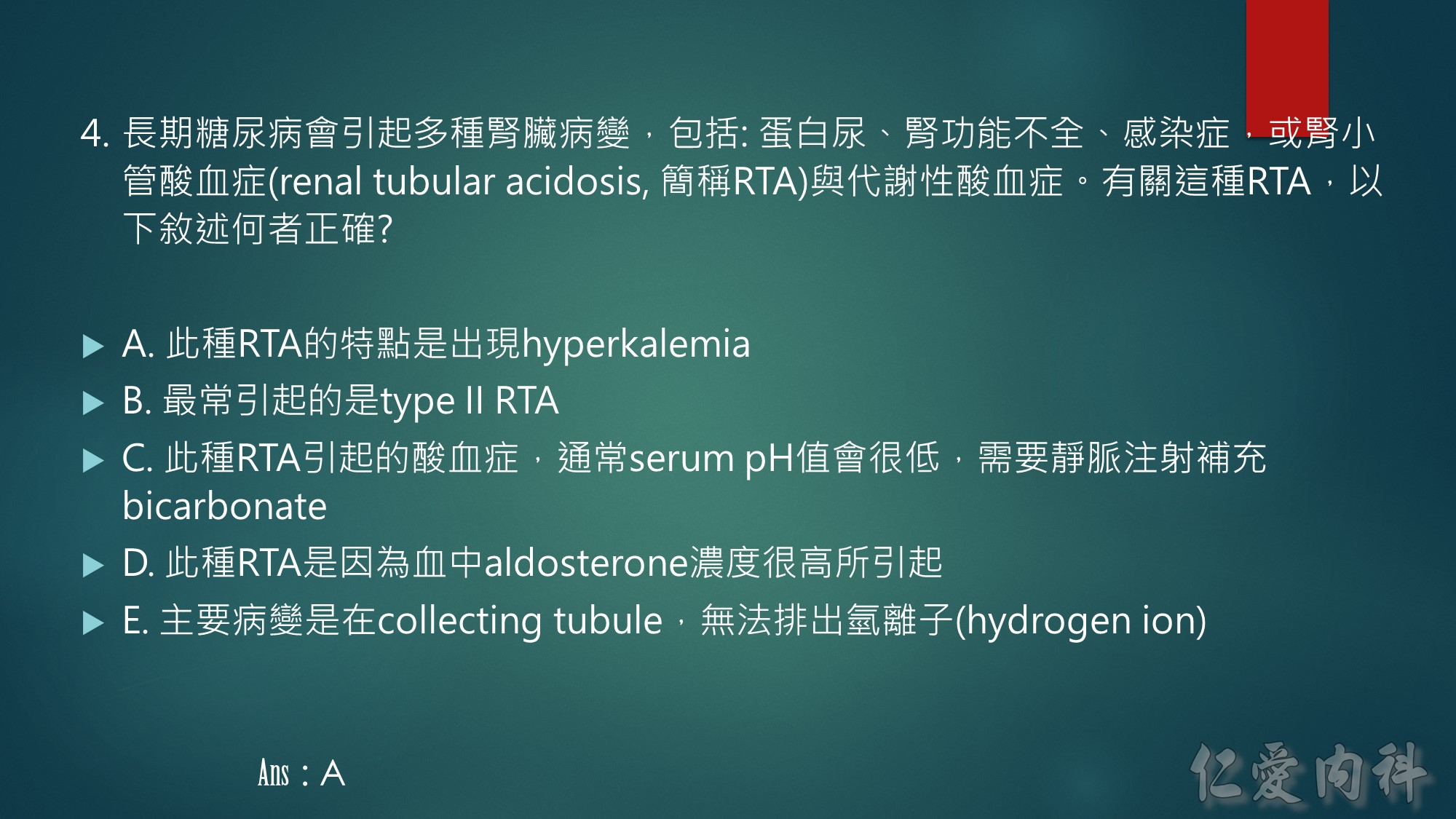
B: type 4
C: pH不會很低
D: aldosterone低
E: 是因為K高,抑制ammonia genesis,因此無法排出H
使用metformin的病人,其post-contrast AKI的機會並沒有比較高。
目前為止也沒有使用metformin的病人,使用顯影劑之後造成lactic acidosis的案例,前提是properly selected for metformin。
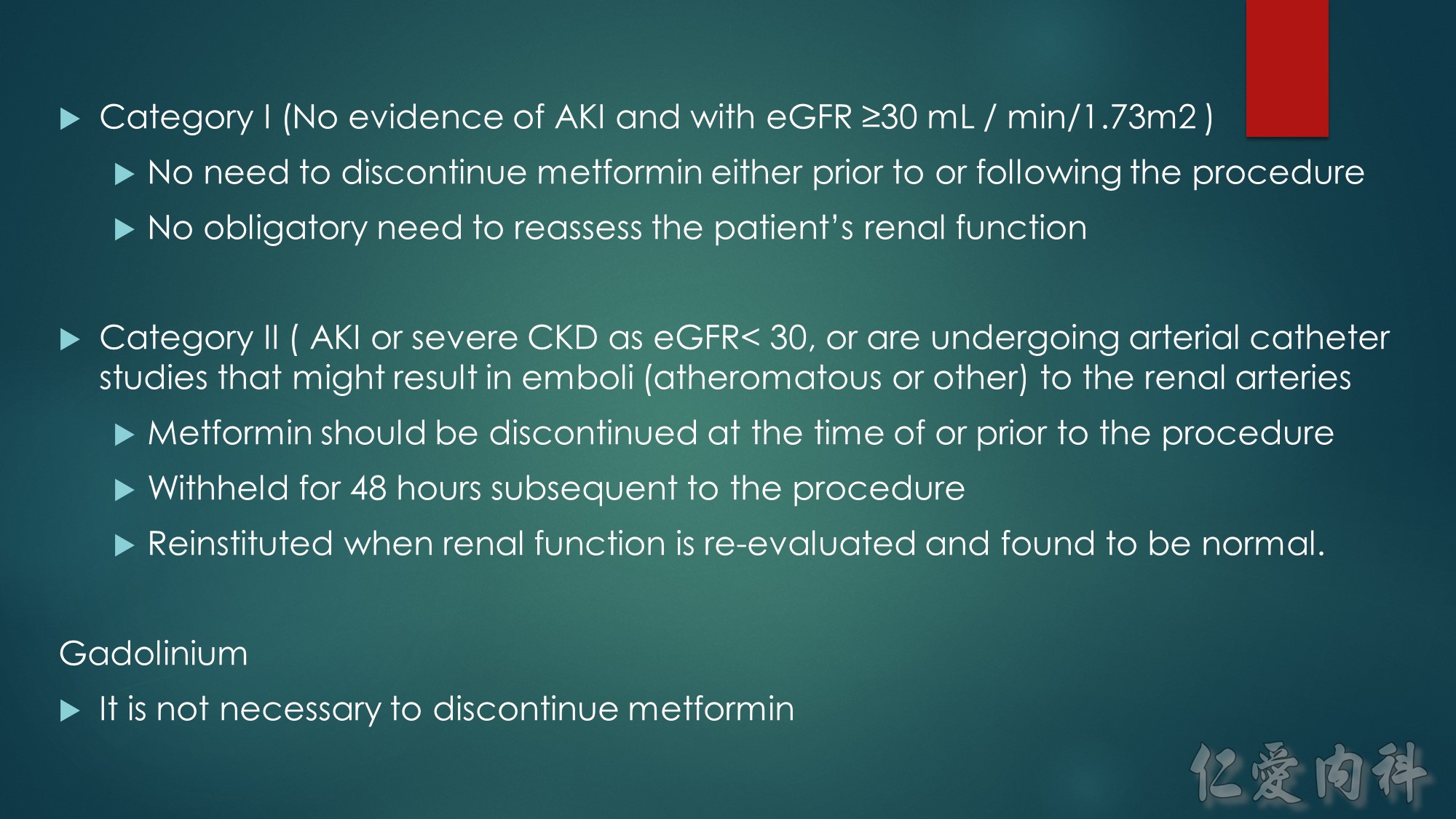
Contrast CT??
1.eGFR>30: 做contrast image study不用停藥,不用特別follow腎功能
2.eGFR<30或是進行的procedure是可能會產生emboli進一步造成renal artery obstruction的,就要在檢查進行當天~檢查後48小時停藥,follow creatinine沒有上升才能把藥家回去。
Contrast MRI?(gadolinium)
不須停用metformin。
*但須注意,過去的說法是gadolinium不傷腎,但目前的evidence證實,CKD stage4 以上不可使用gadolinium,因為會造成NSF(nephrogenic systemic fibrosis)。因為gadolinium為重金屬,會沉積在皮膚、心臟、肝腎等等造成fibrosis。腎功能不好的病人其排出gadolinium的功能較差,重金屬沉積的機會就高。
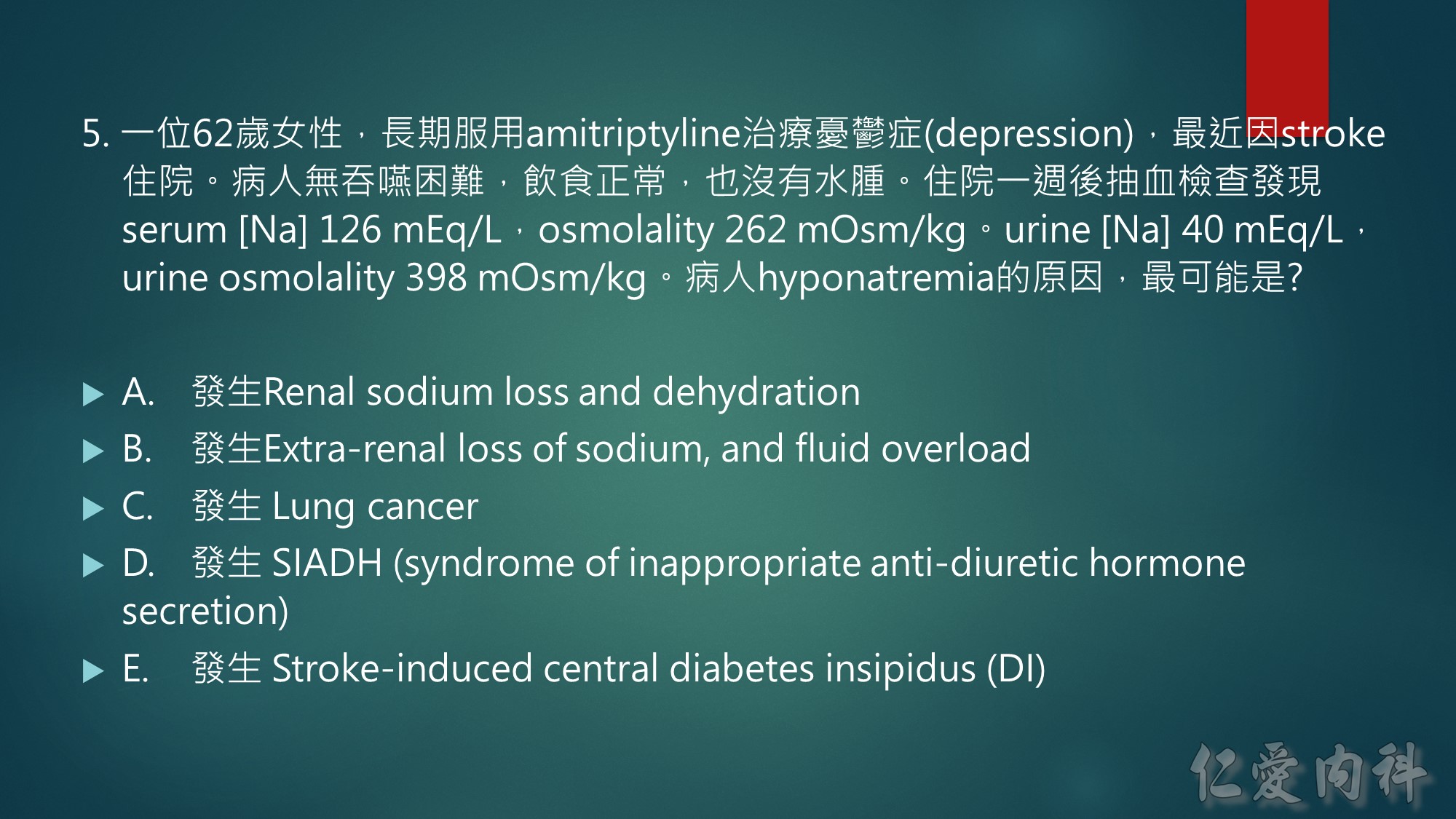
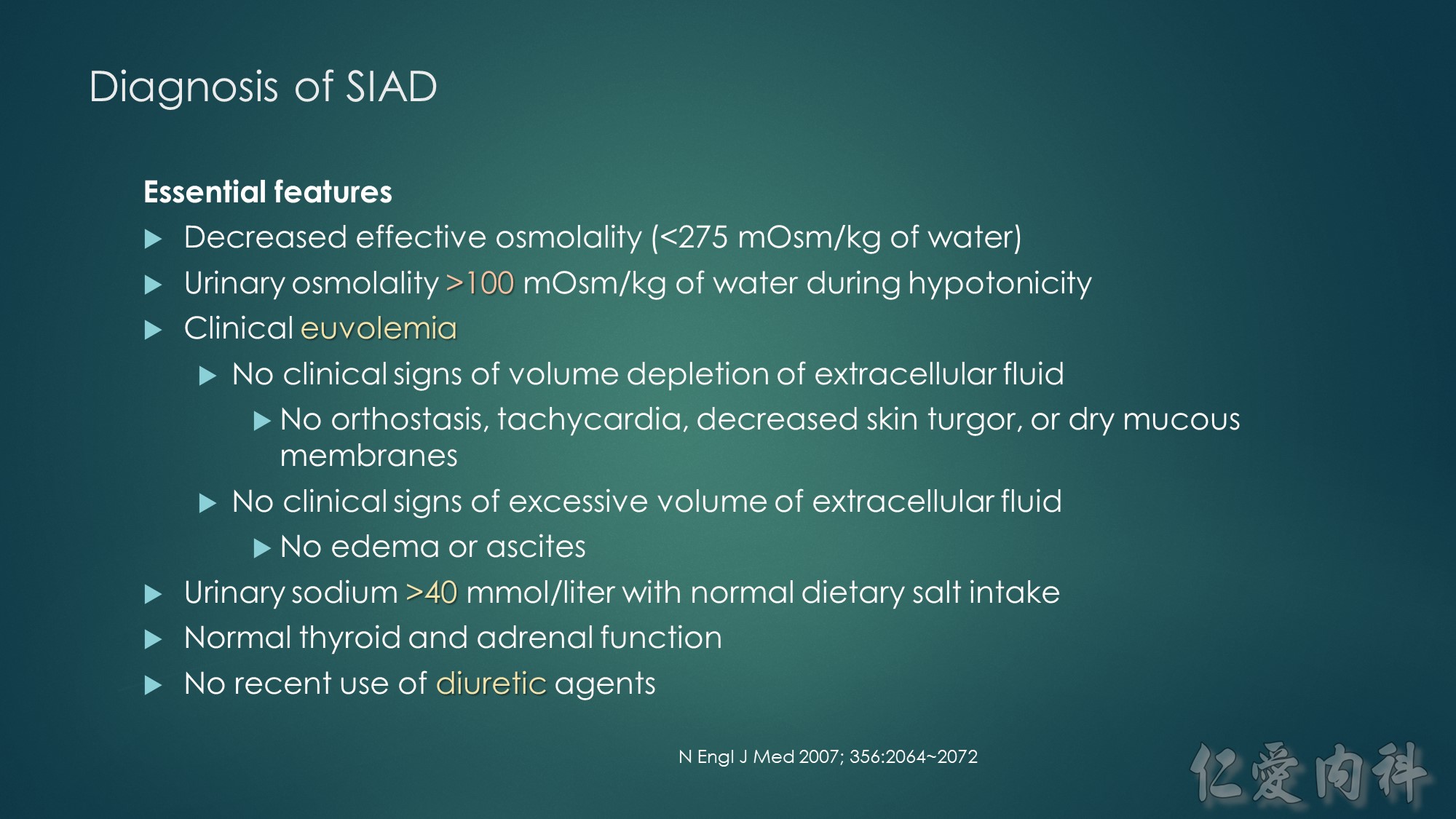
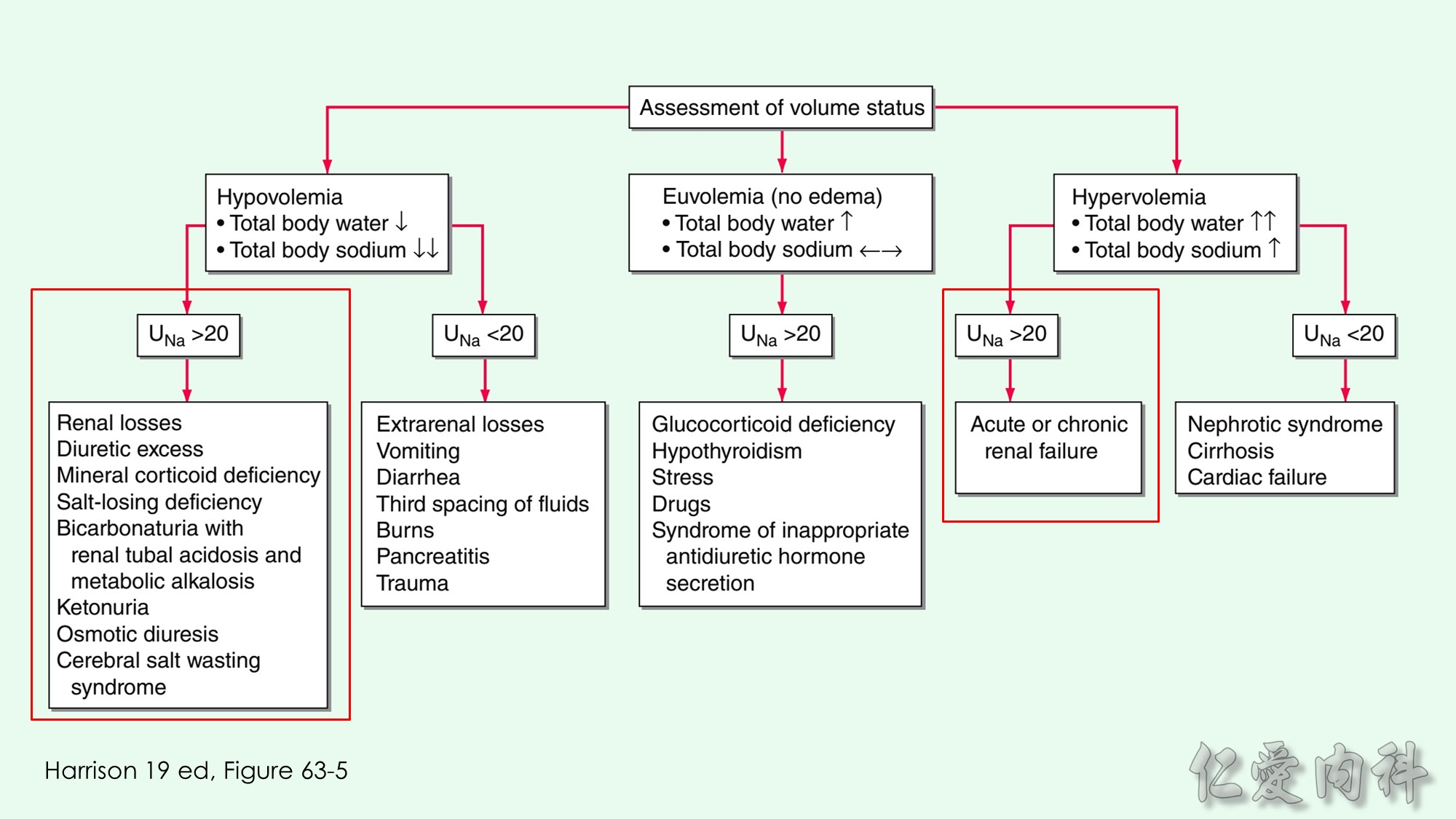
低血鈉第一步看osmolality。
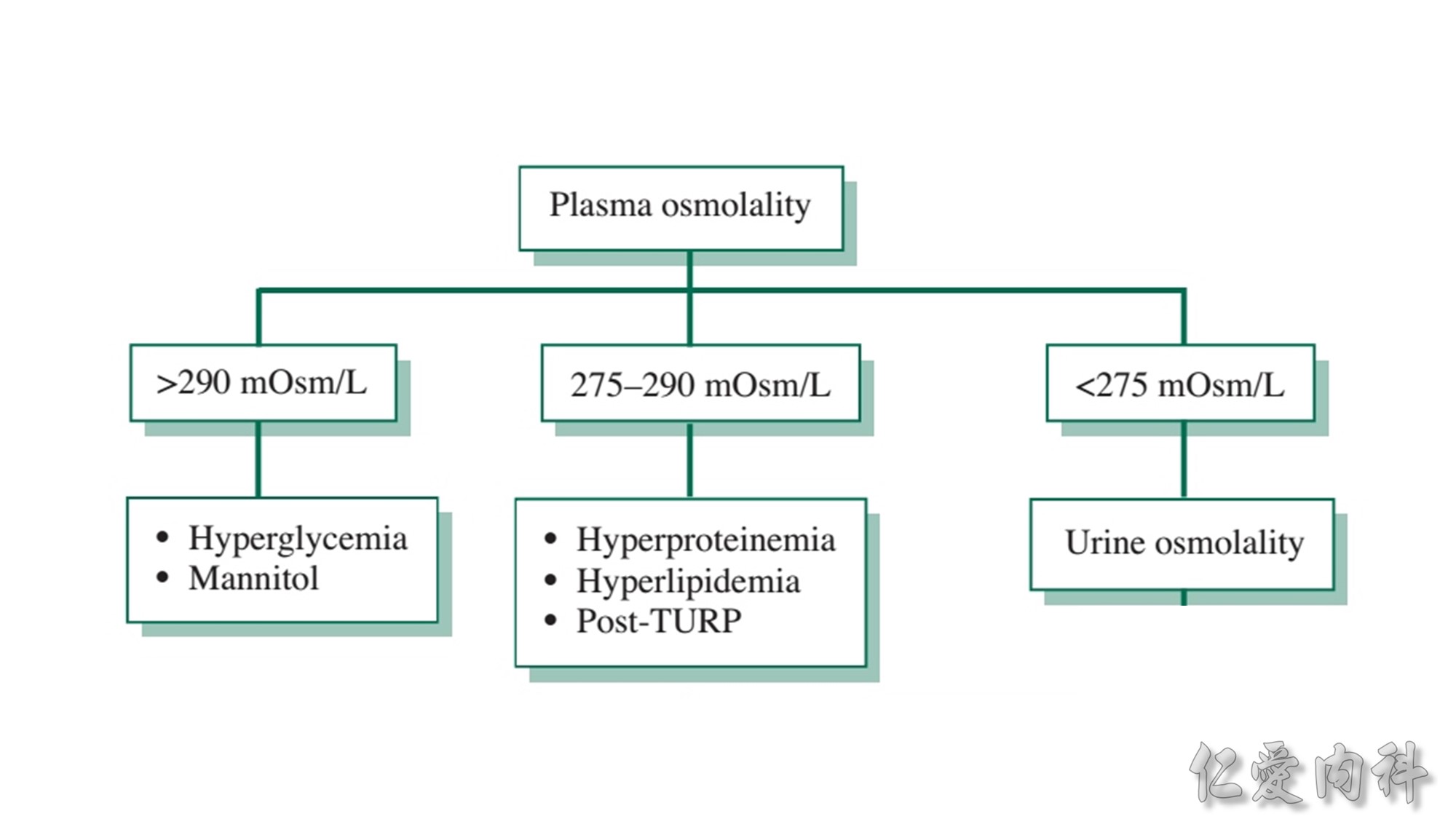
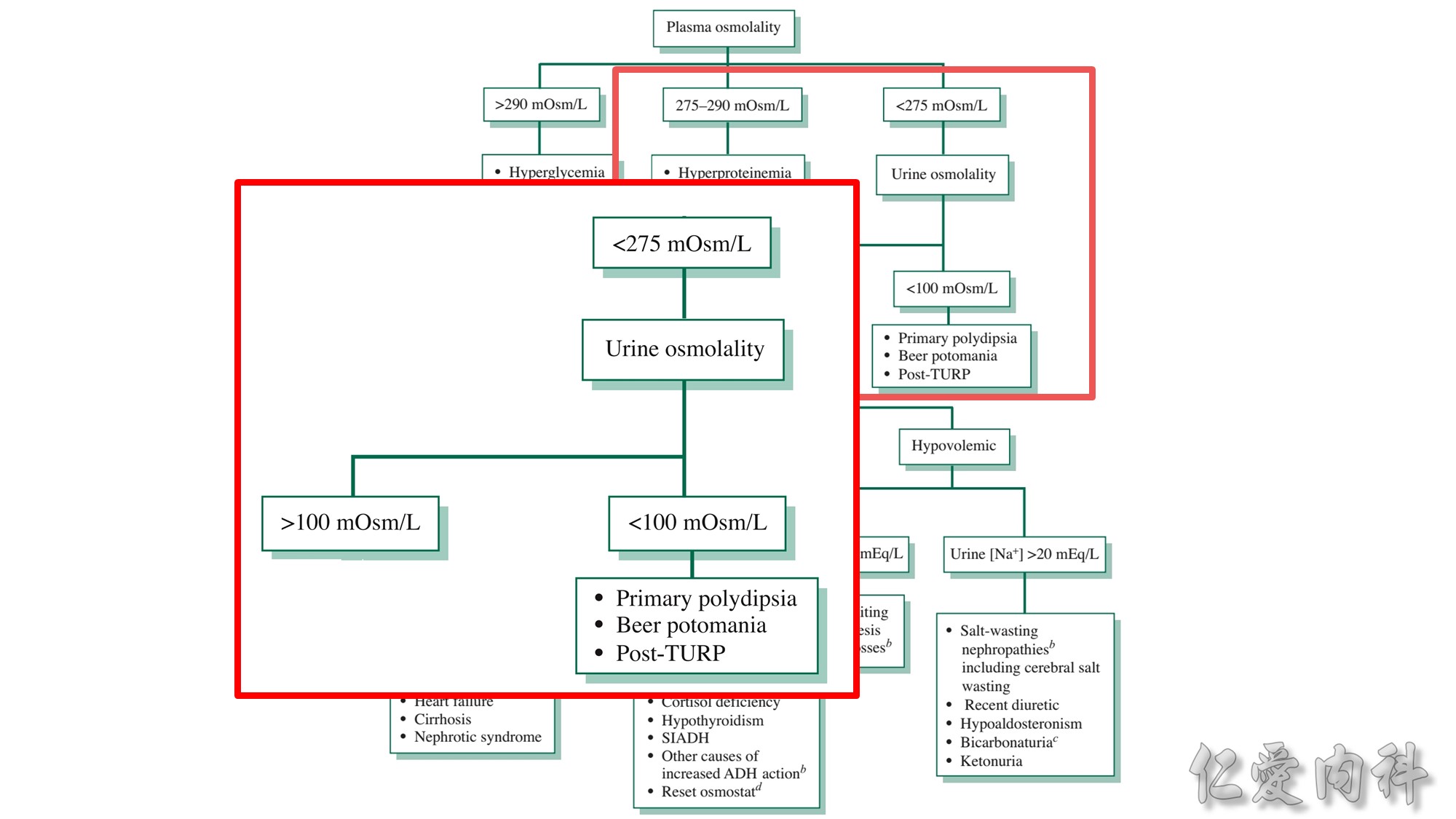
低血鈉第一步看osmolality。
這個Case osmolality是低的,因此是真的低血鈉。
第二步是看volume status。
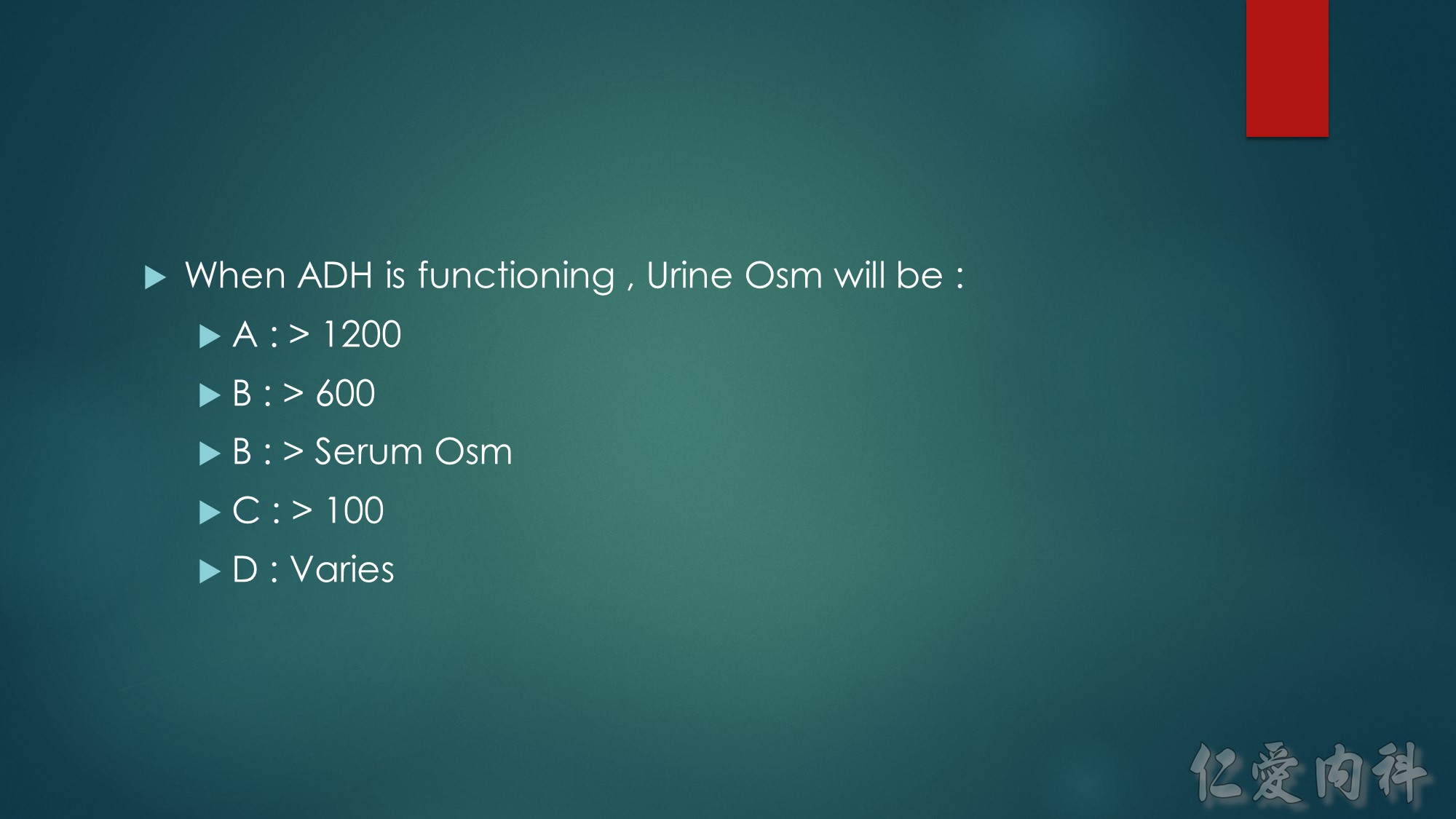
– 若病人ADH有作用,urine osmolality>100
– 若病人是腫的,可能HF, liver failure, nephrotic syndrome,雖然水多,但是effective volume不夠,身體拼命吸水吸鹽,只是吸水比起吸鹽多→ADH有作用!
– 若病人是乾的,urine osmolality也是上升的,因為想把水吸回來→ADH有作用!
– 若euvolemia,ADH又分泌,才算SIADH
– 結論: 在true hypotonic hyponatermia之下,除了多喝水的那種,ADH都是有分泌的
– 若urine osmolality<100表示是喝太多水稀釋掉的。
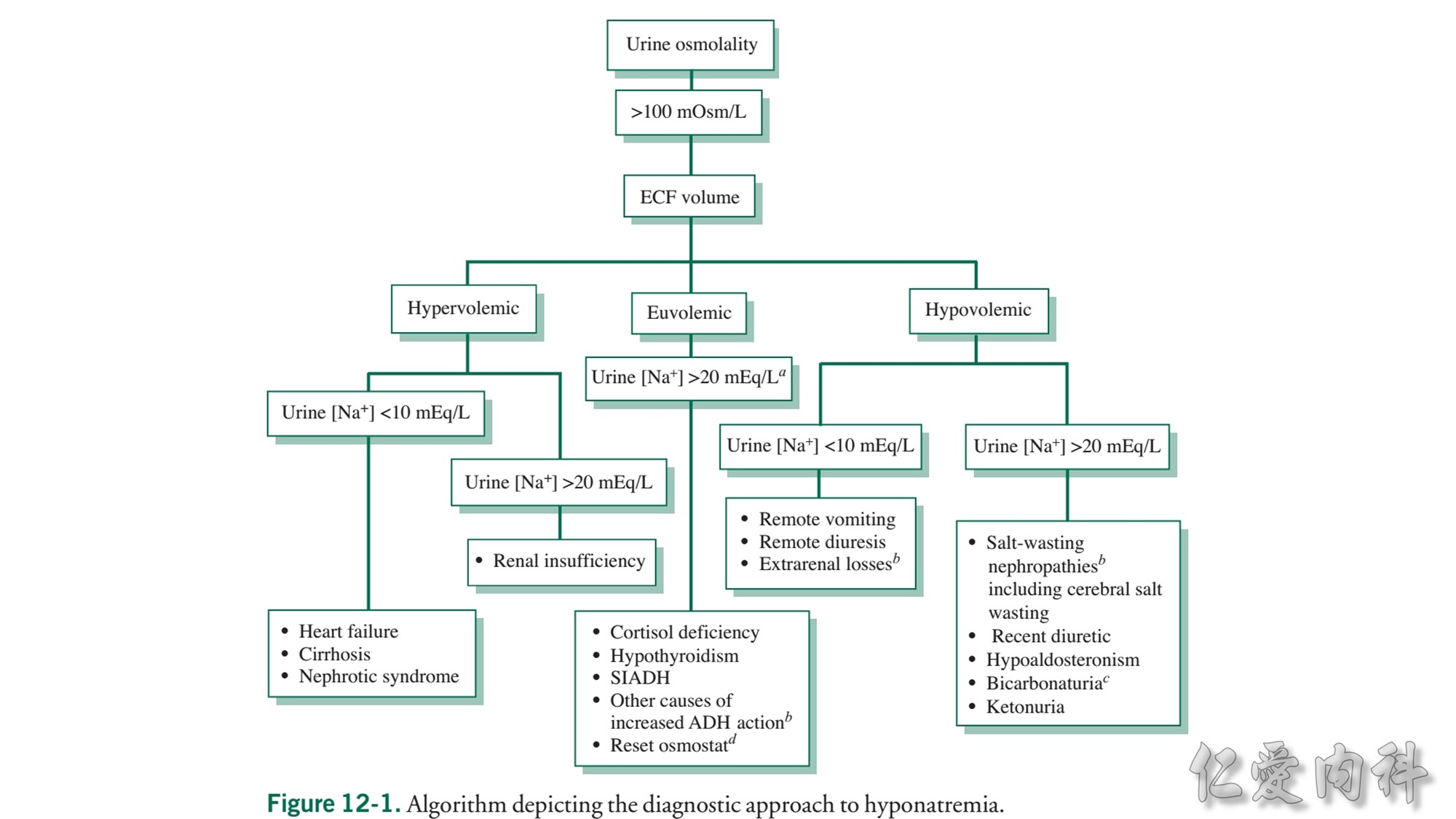
看volume status。
– 若病人ADH有作用,urine osmolality>100
– 若病人是腫的,可能HF, liver failure, nephrotic syndrome,雖然水多,但是effective volume不夠,身體拼命吸水吸鹽,只是吸水比起吸鹽多→ADH有作用!
– 若病人是乾的,urine osmolality也是上升的,因為想把水吸回來→ADH有作用!
– 若euvolemia,ADH又分泌,才算SIADH
– 結論: 在true hypotonic hyponatermia之下,除了多喝水的那種,ADH都是有分泌的
– 若urine osmolality<100表示是喝太多水稀釋掉的。
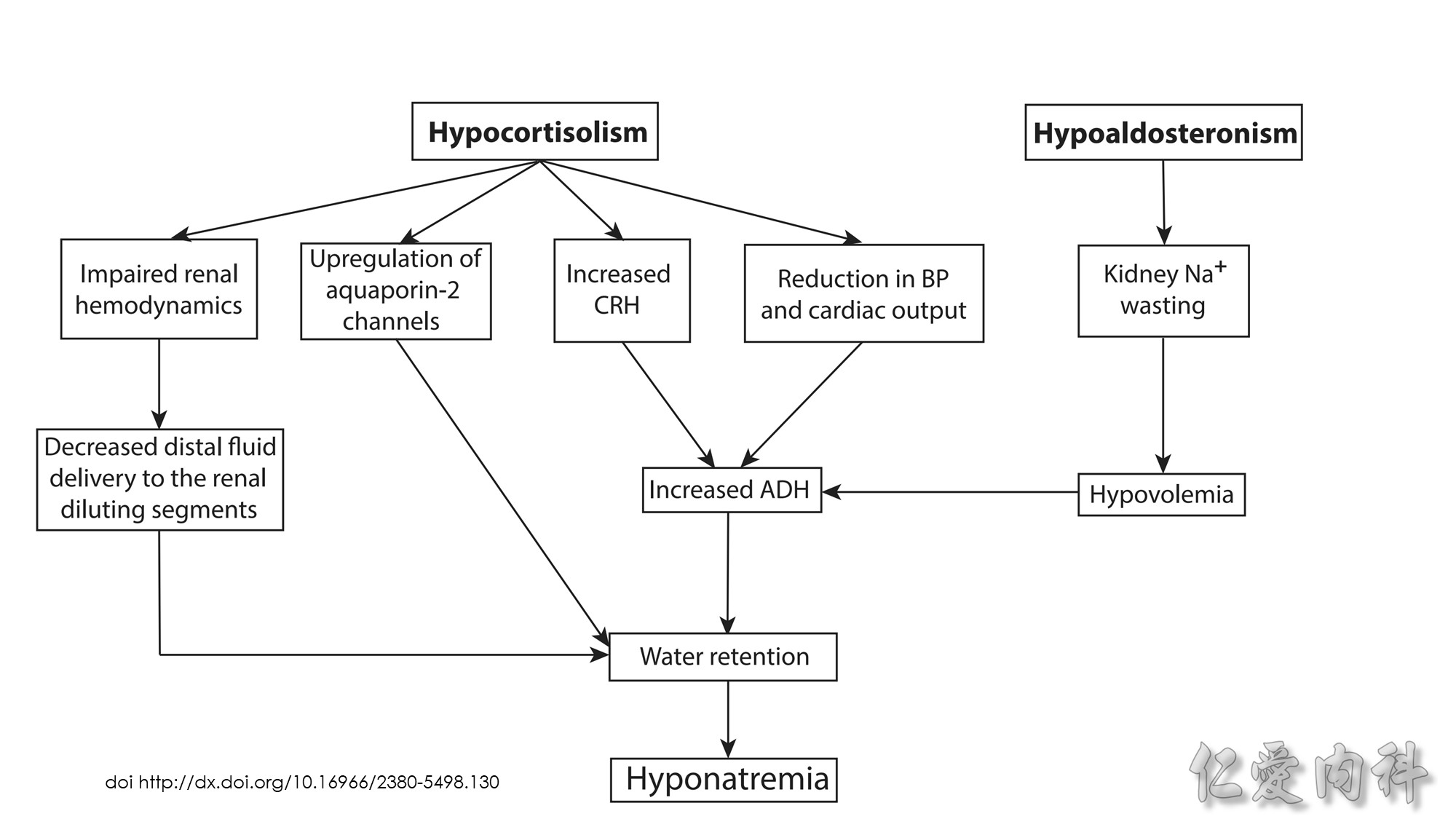
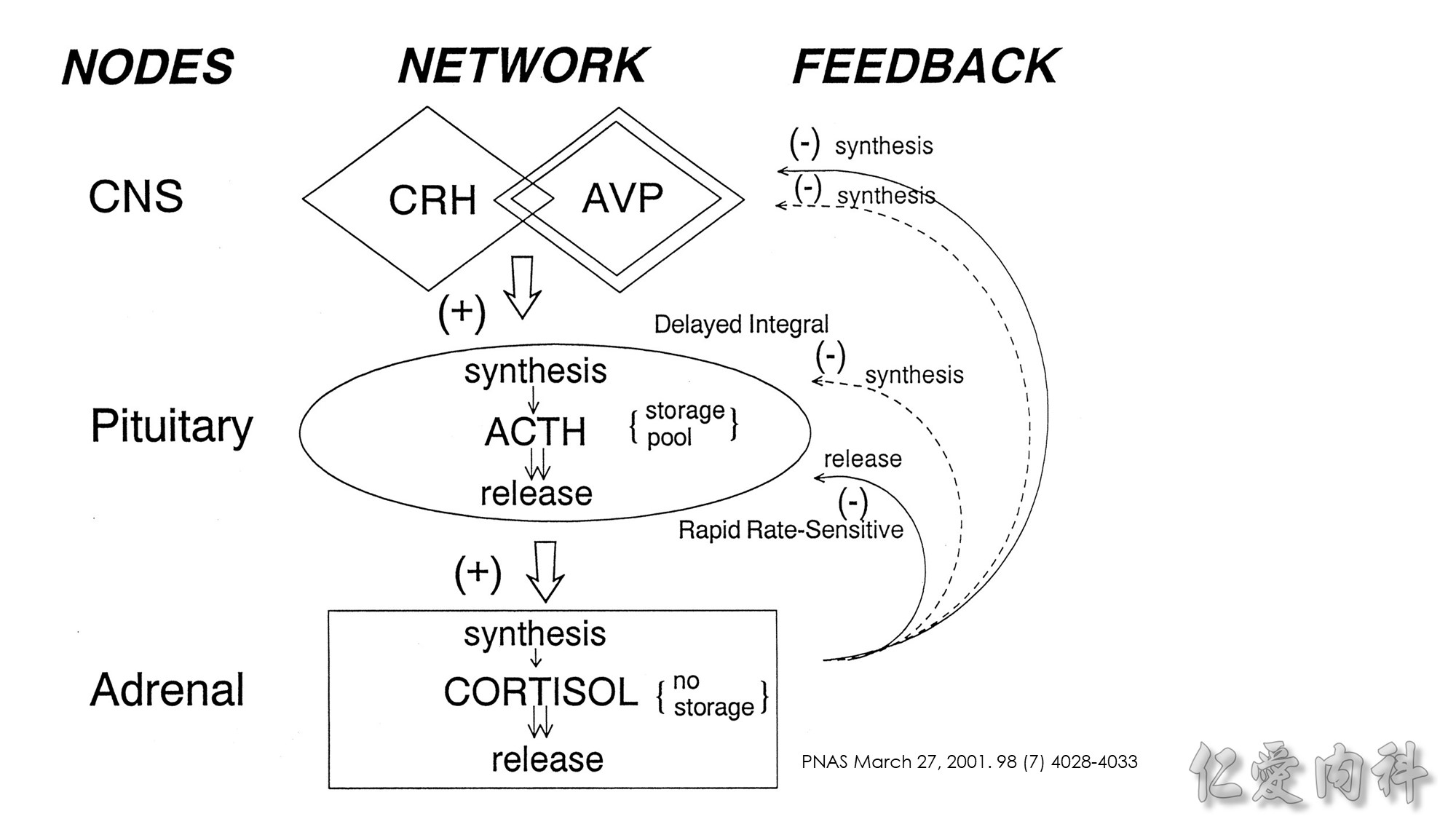
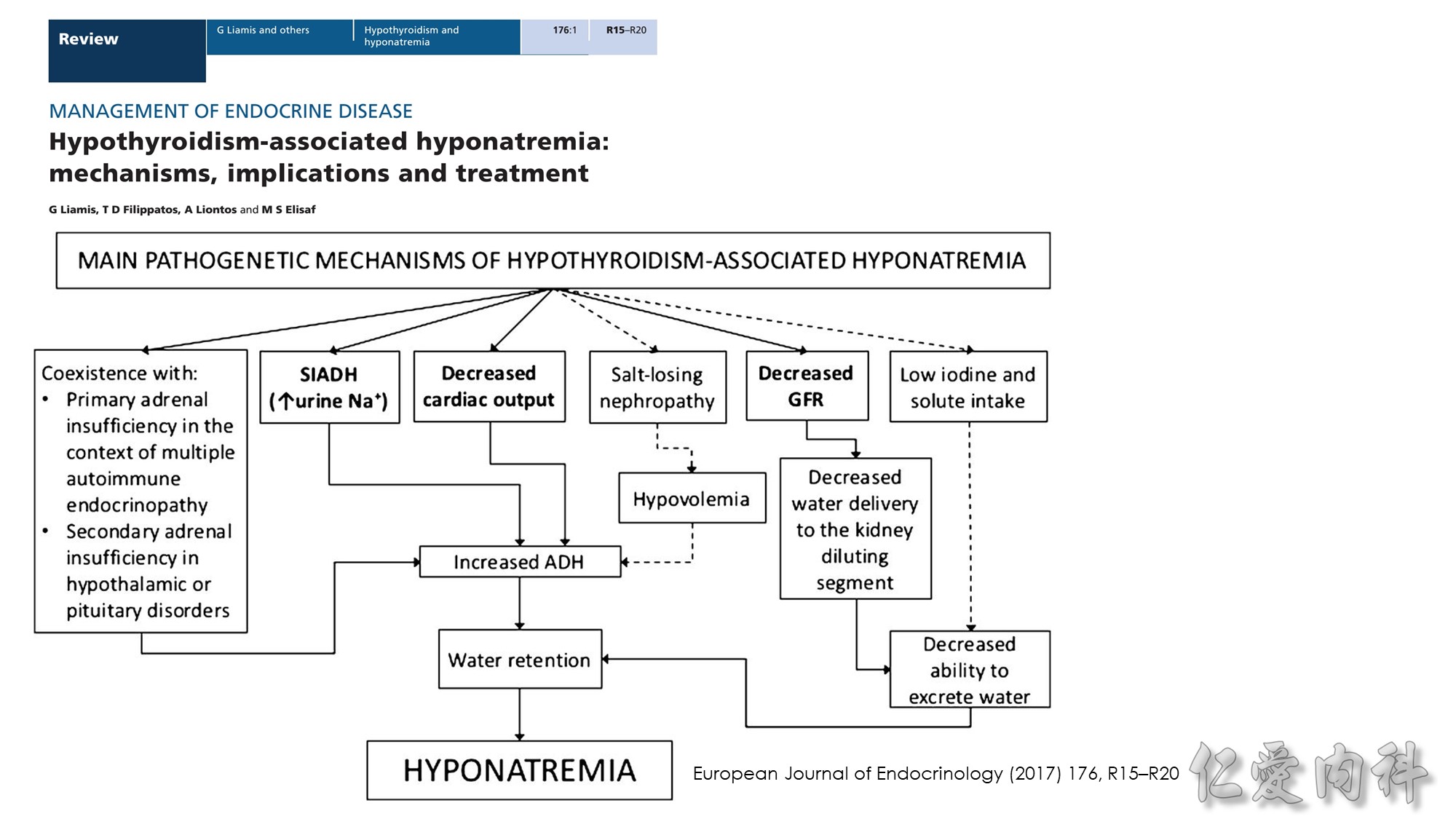
* 另外hypothyroidism, adrenal insufficienc也會SIADH
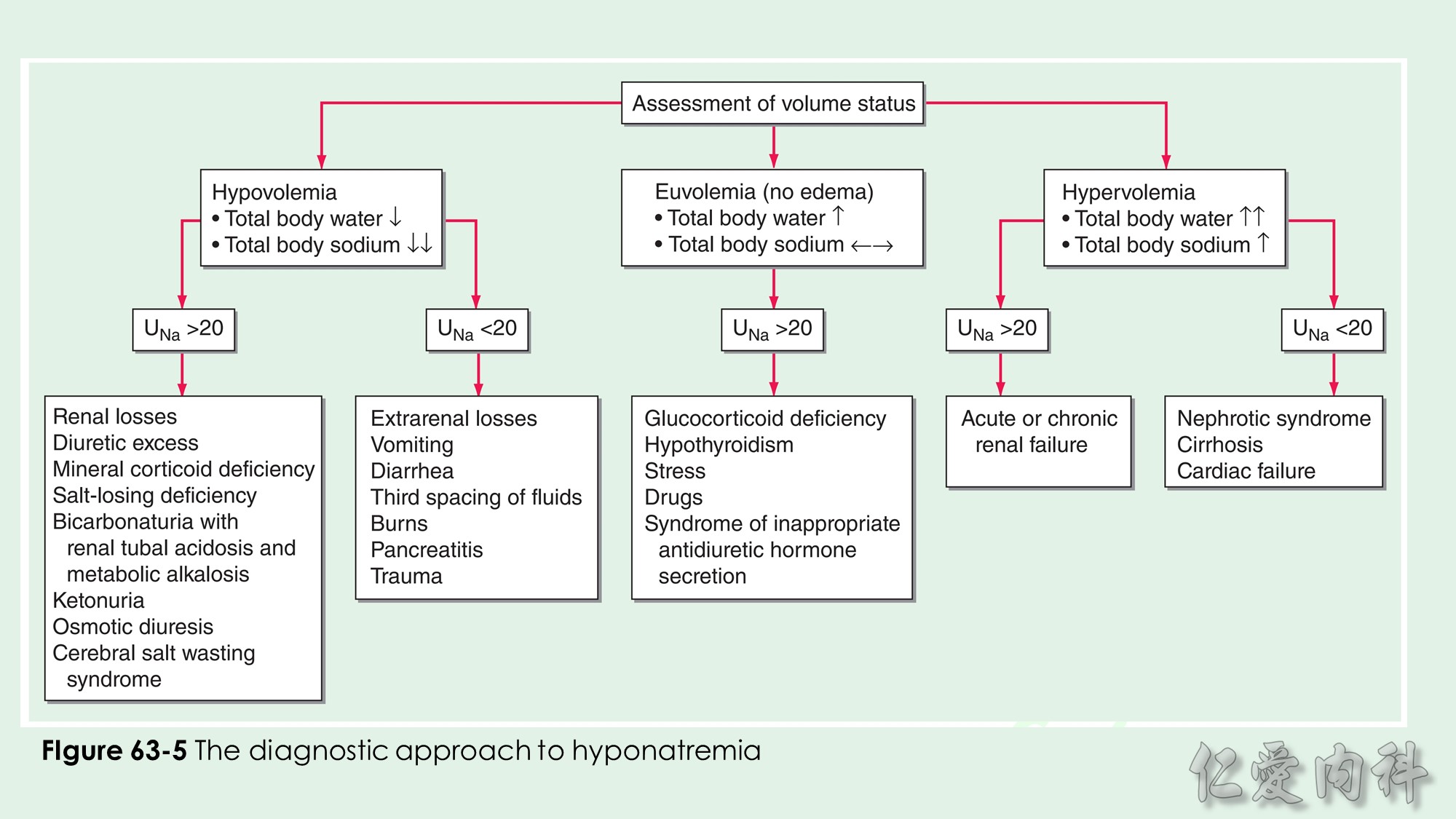
ADH function: U osm>100
SIADH的前提是euvolemic
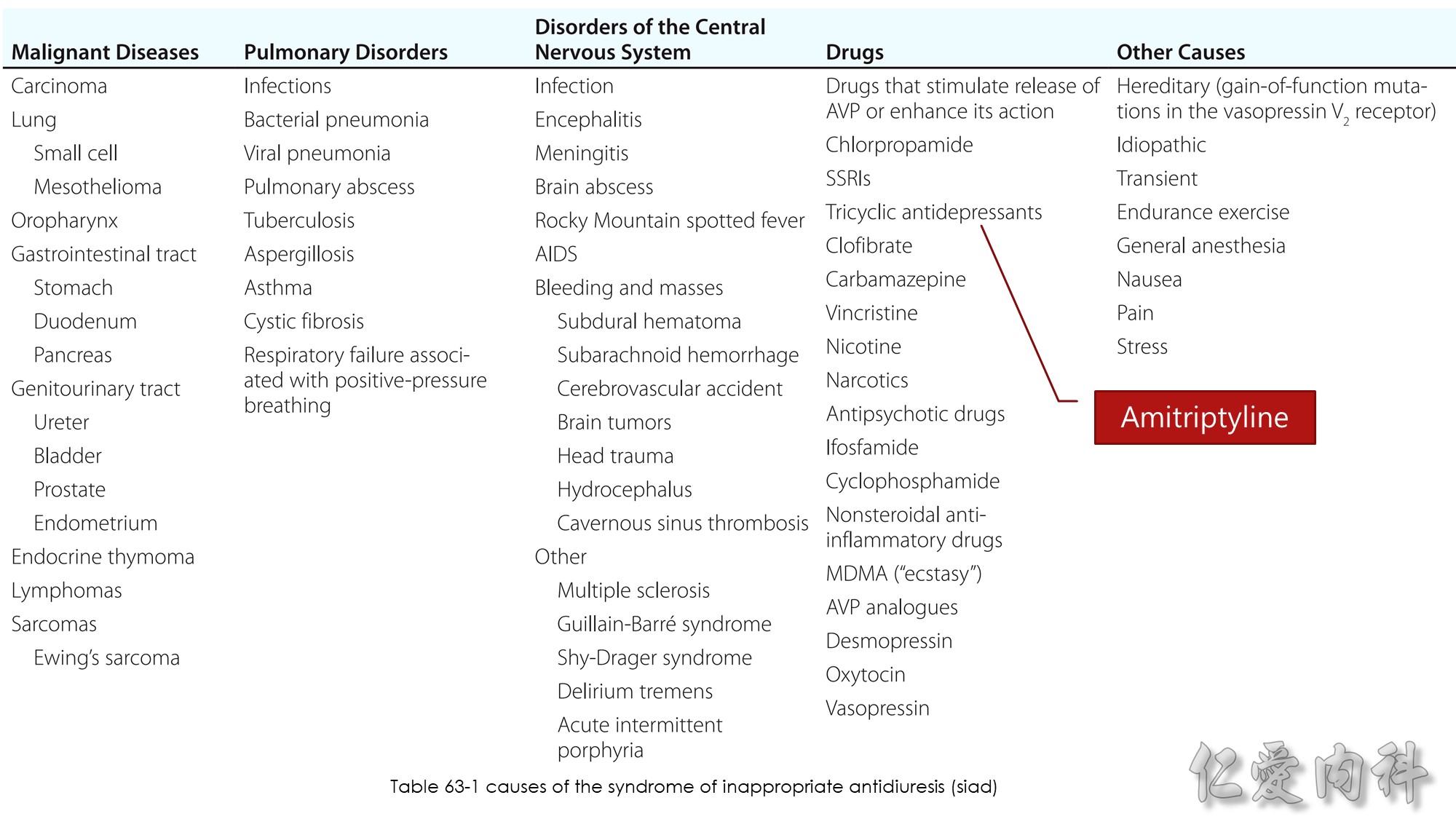
造成inappropriate ADH之藥物
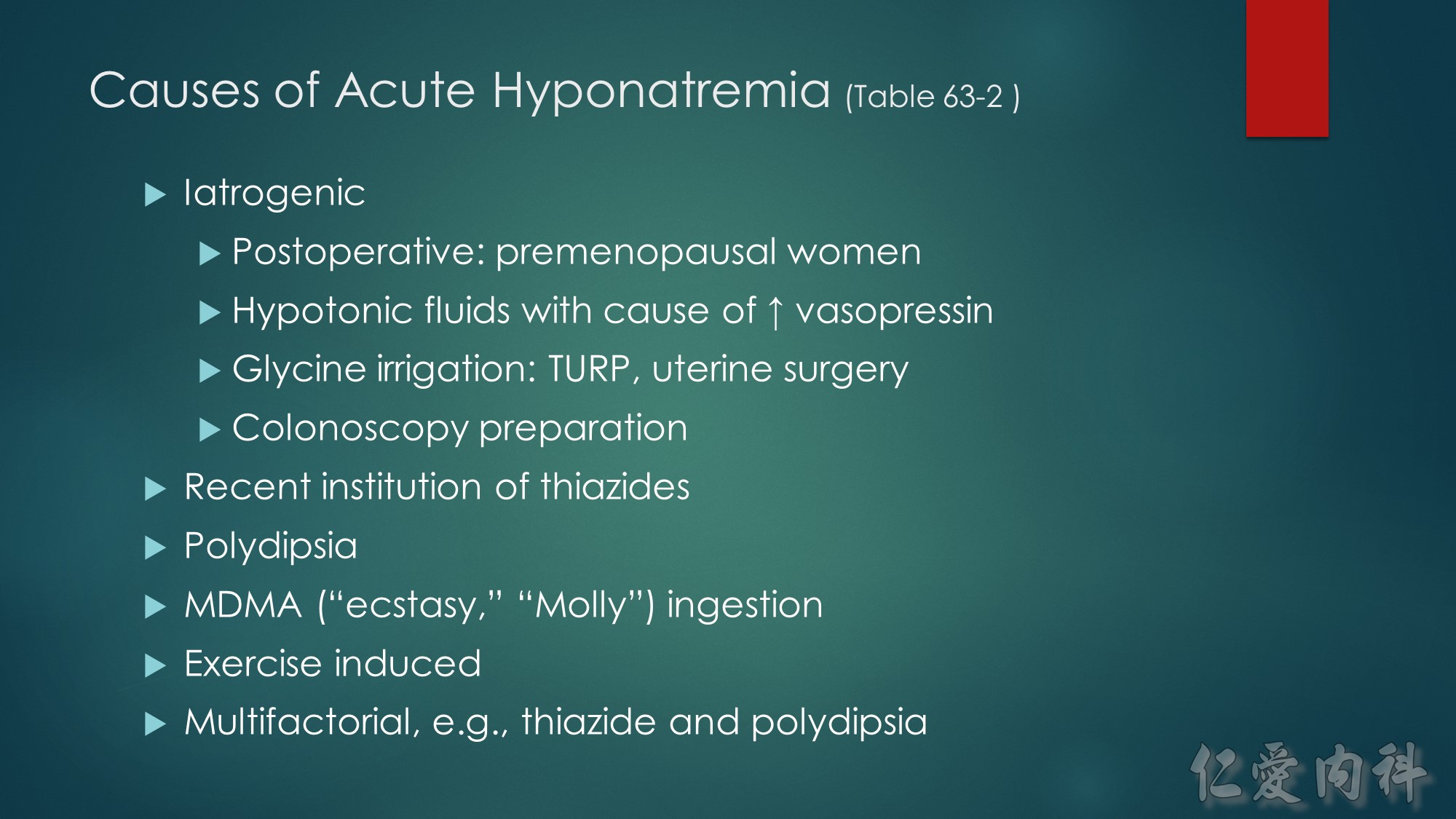
Polydipsia(>12L)

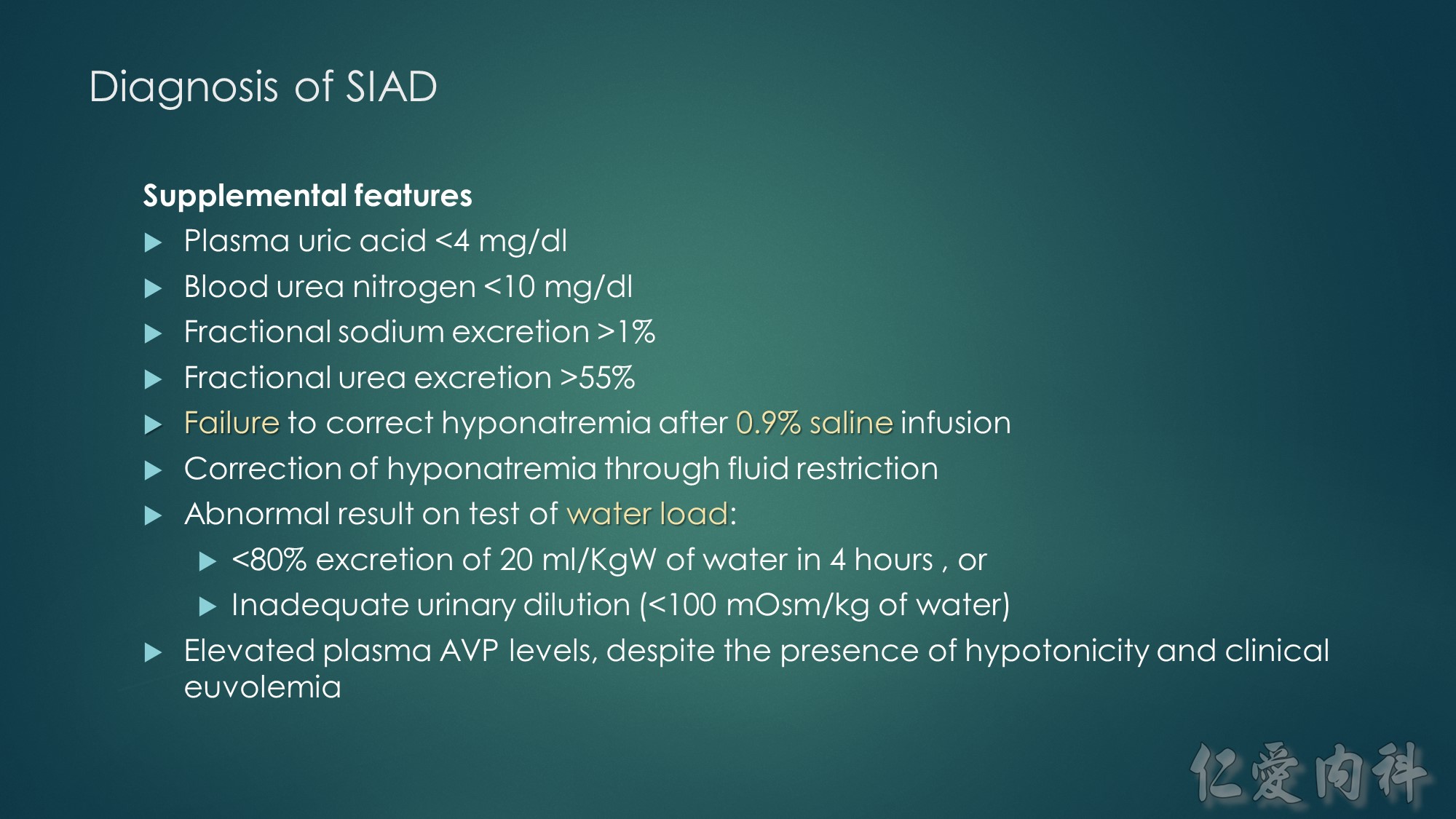
SIADH病人灌n/s,Na會越灌越低。
Water load test: 每公斤灌20cc的水,在四個小時內會排出80%的水,正常人在這樣的情況下,血osmo恆定,尿osmo下降。但SIADH的urine osmolality仍會大於100。
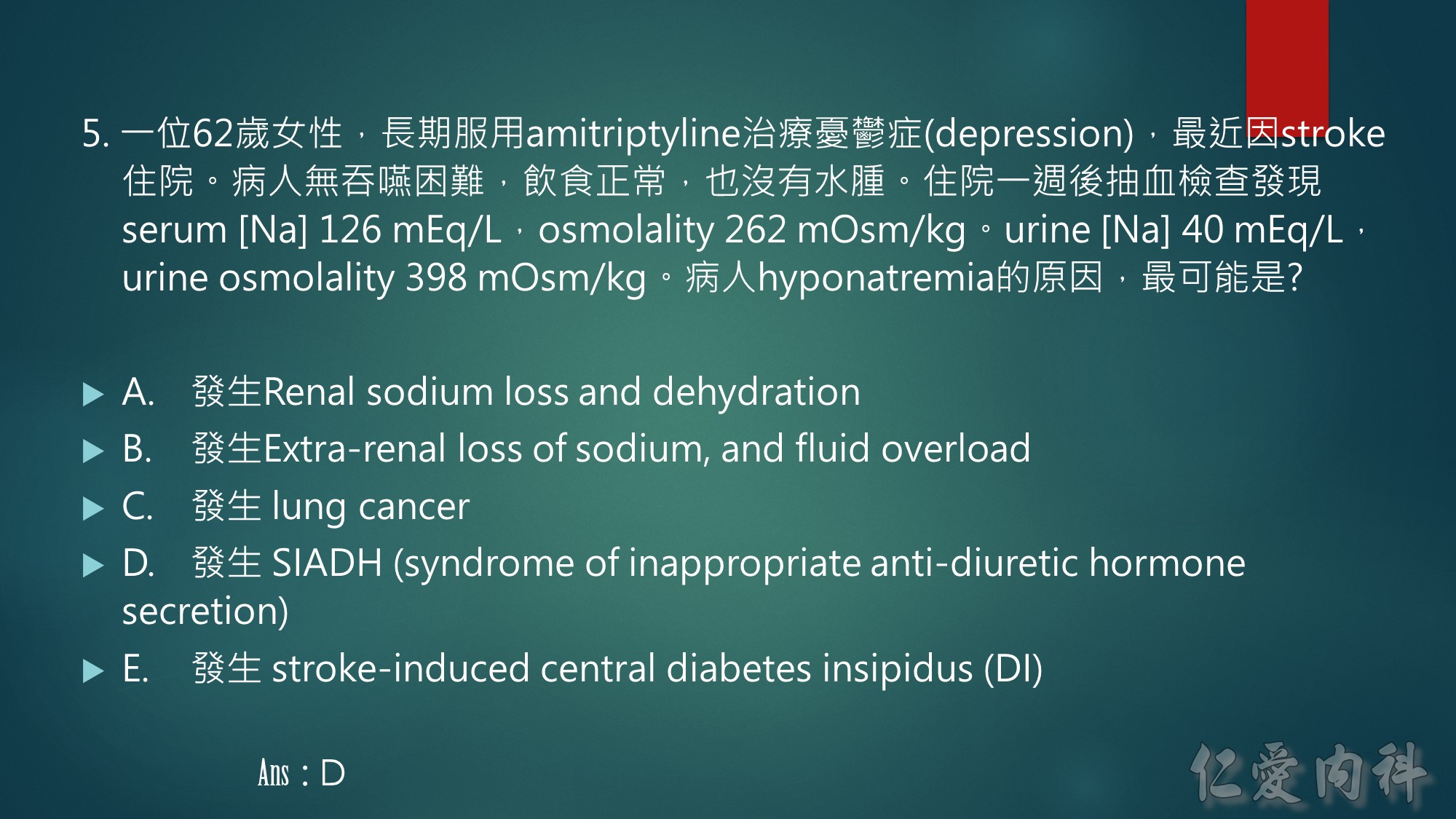
E: DI Na上升
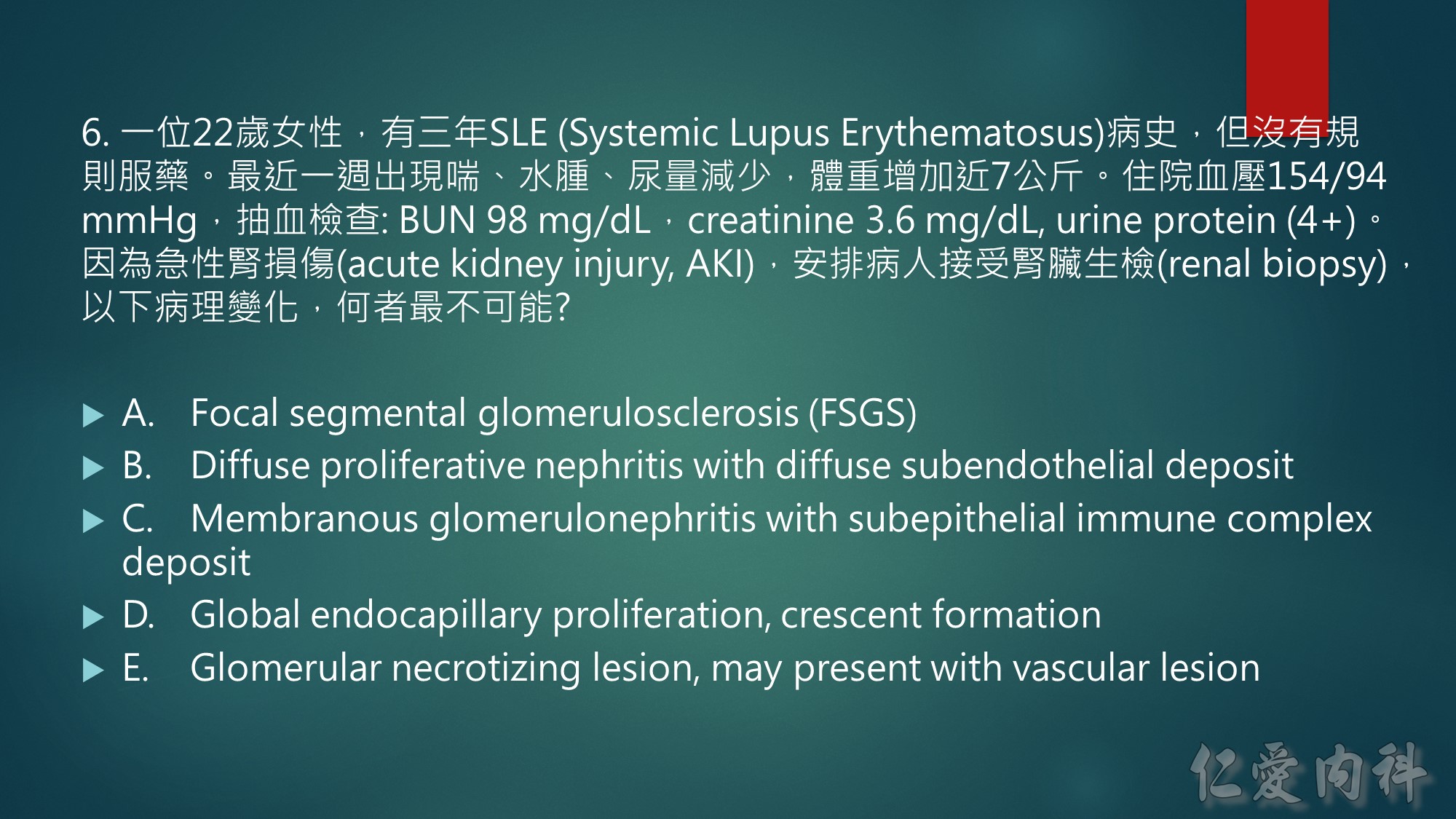
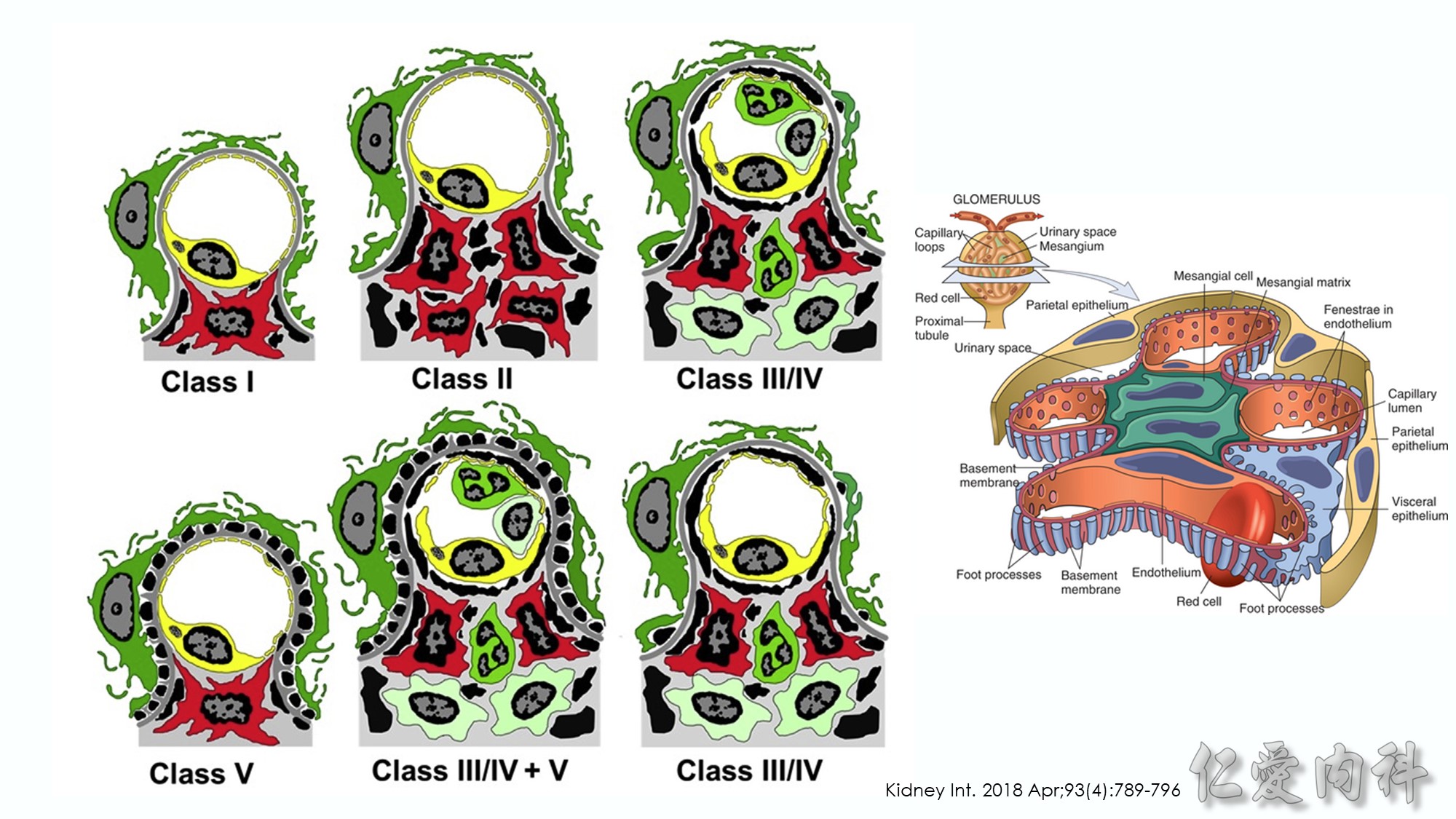
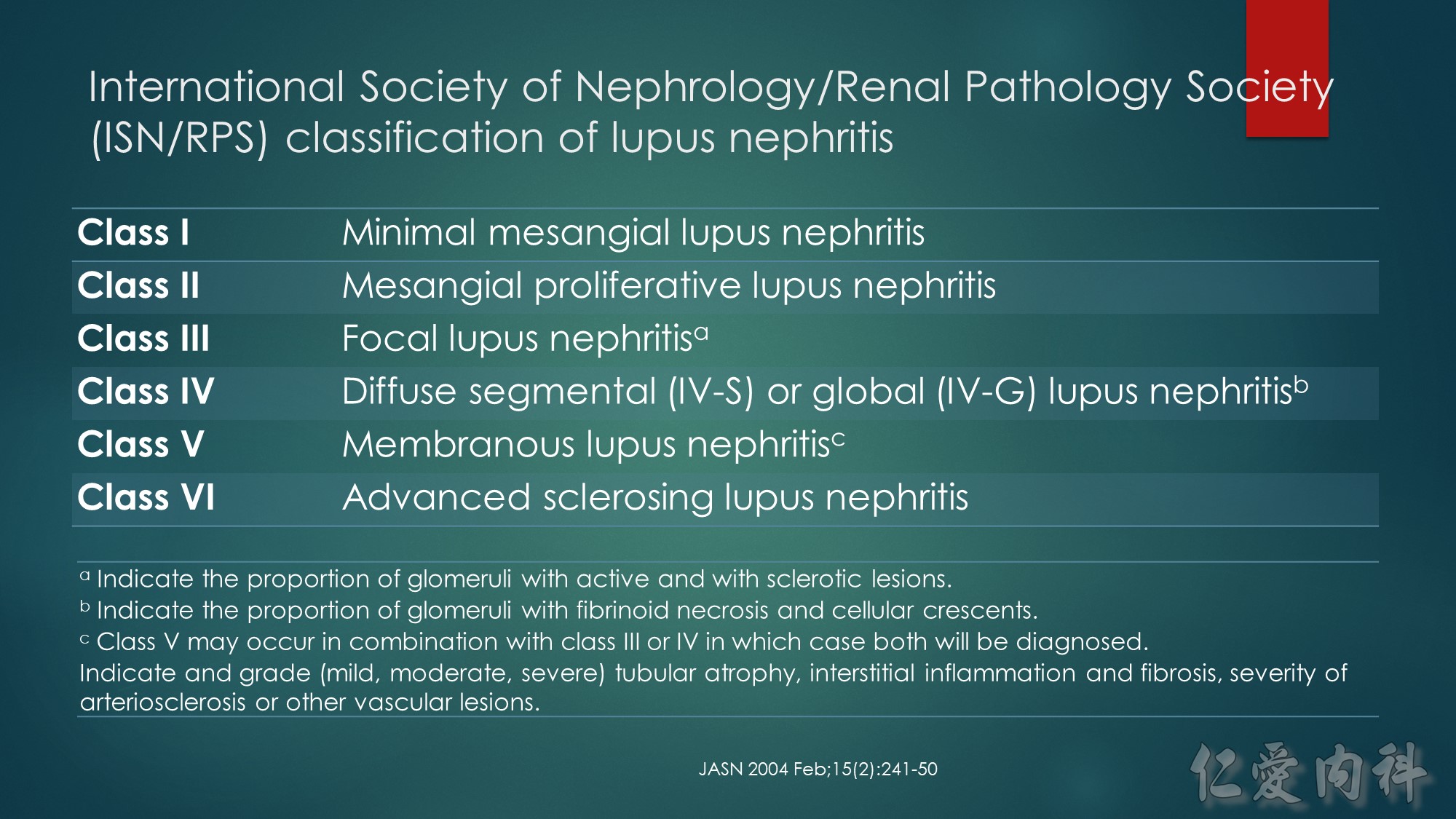
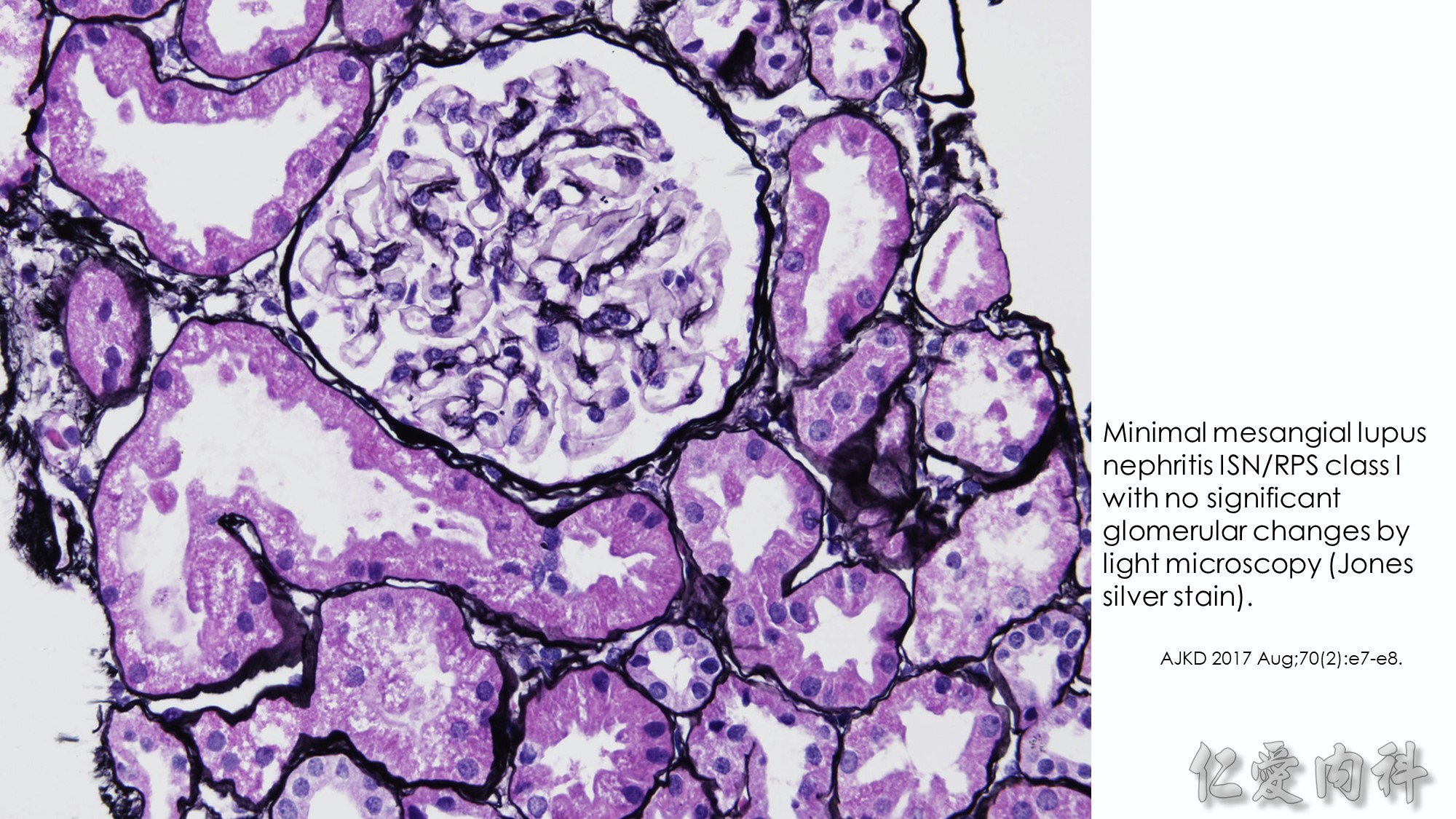
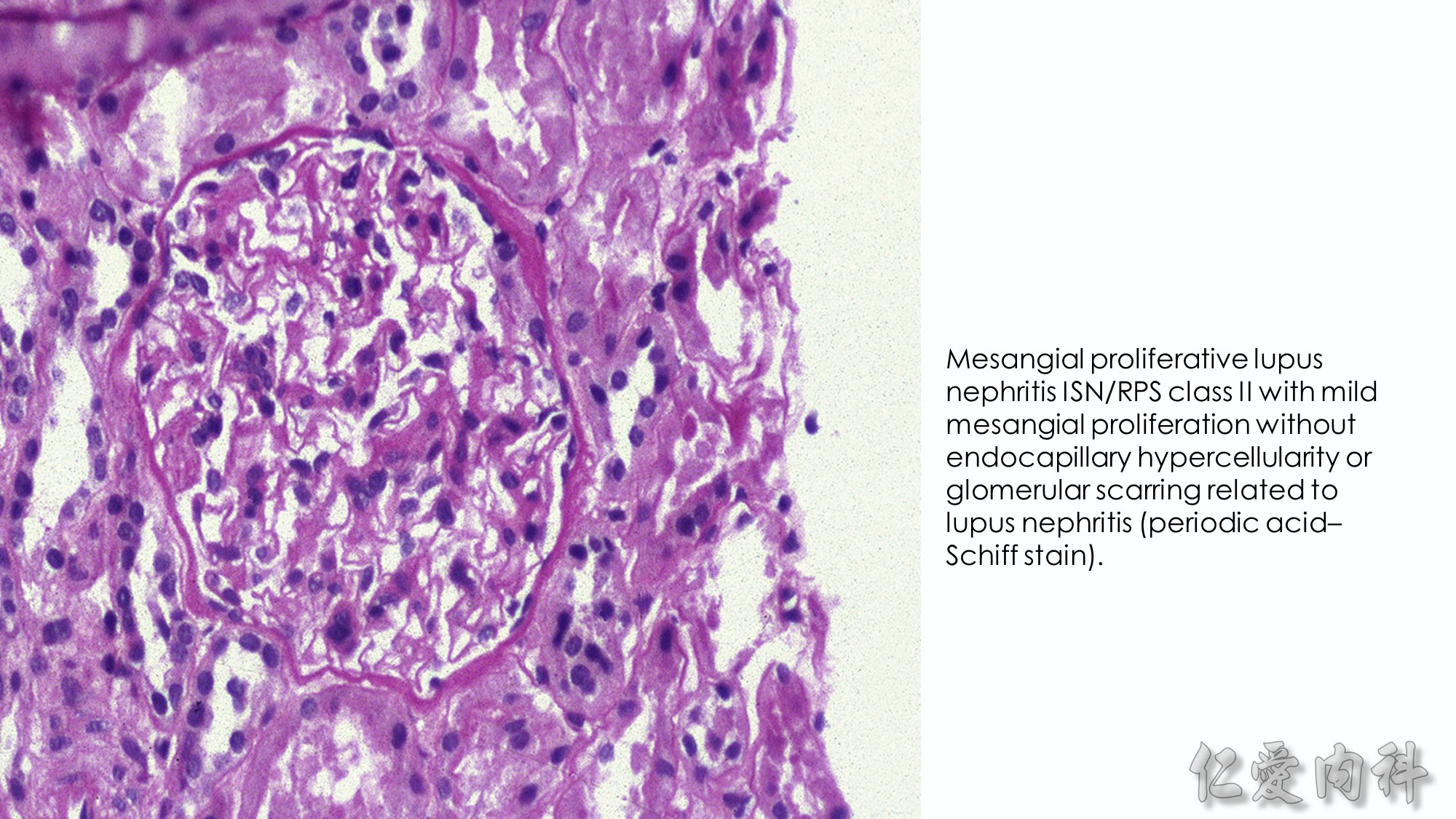
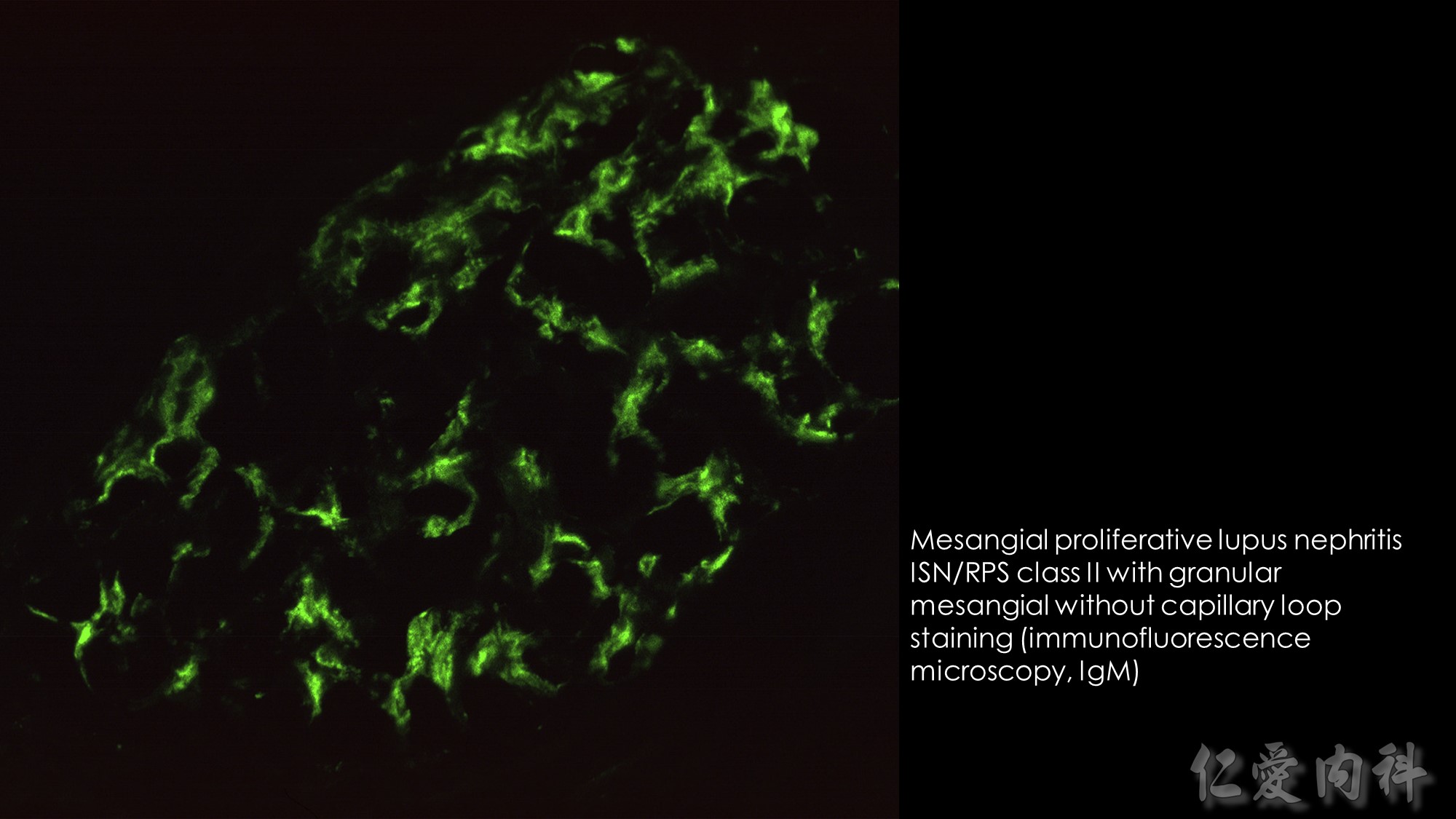
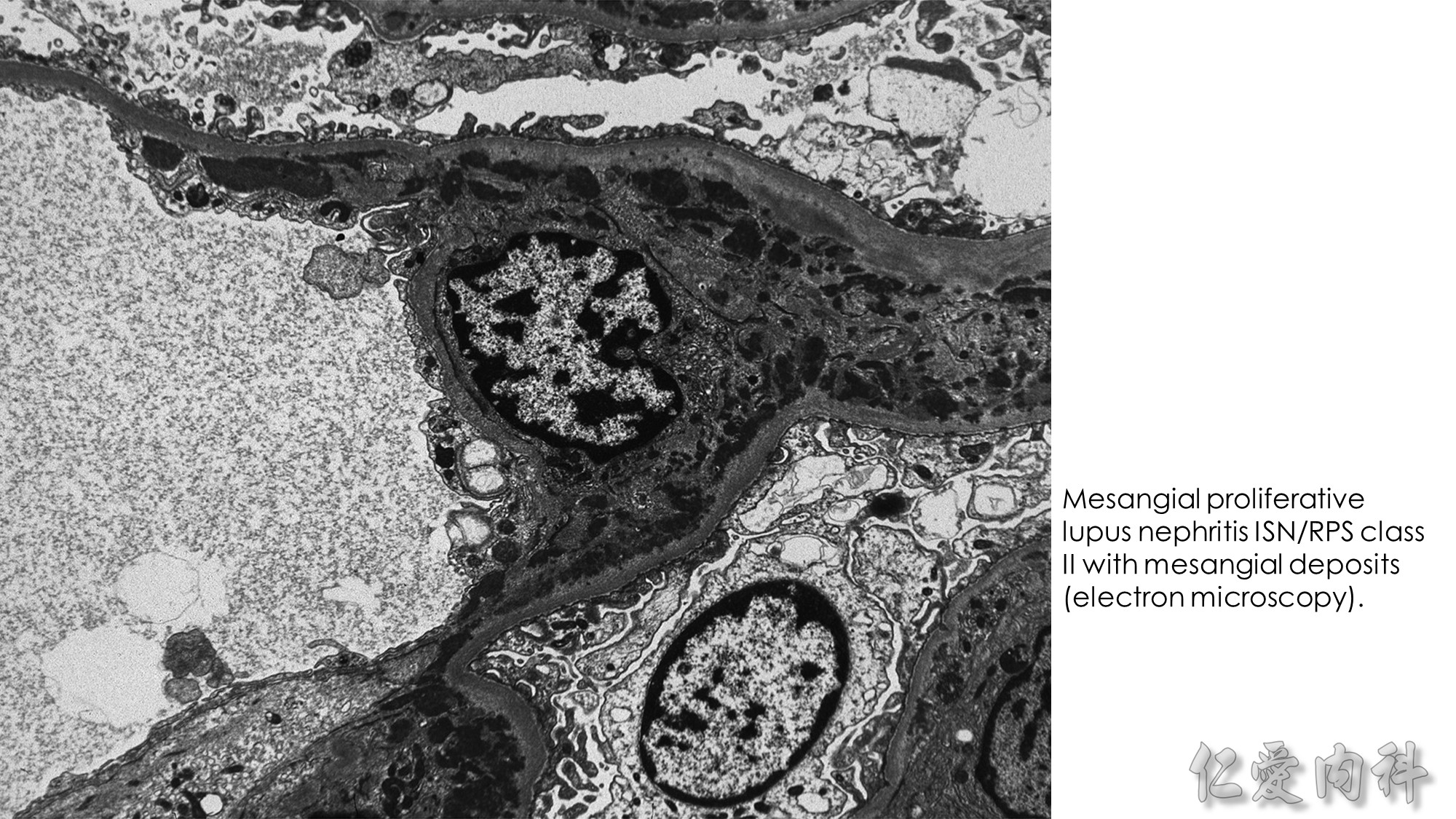
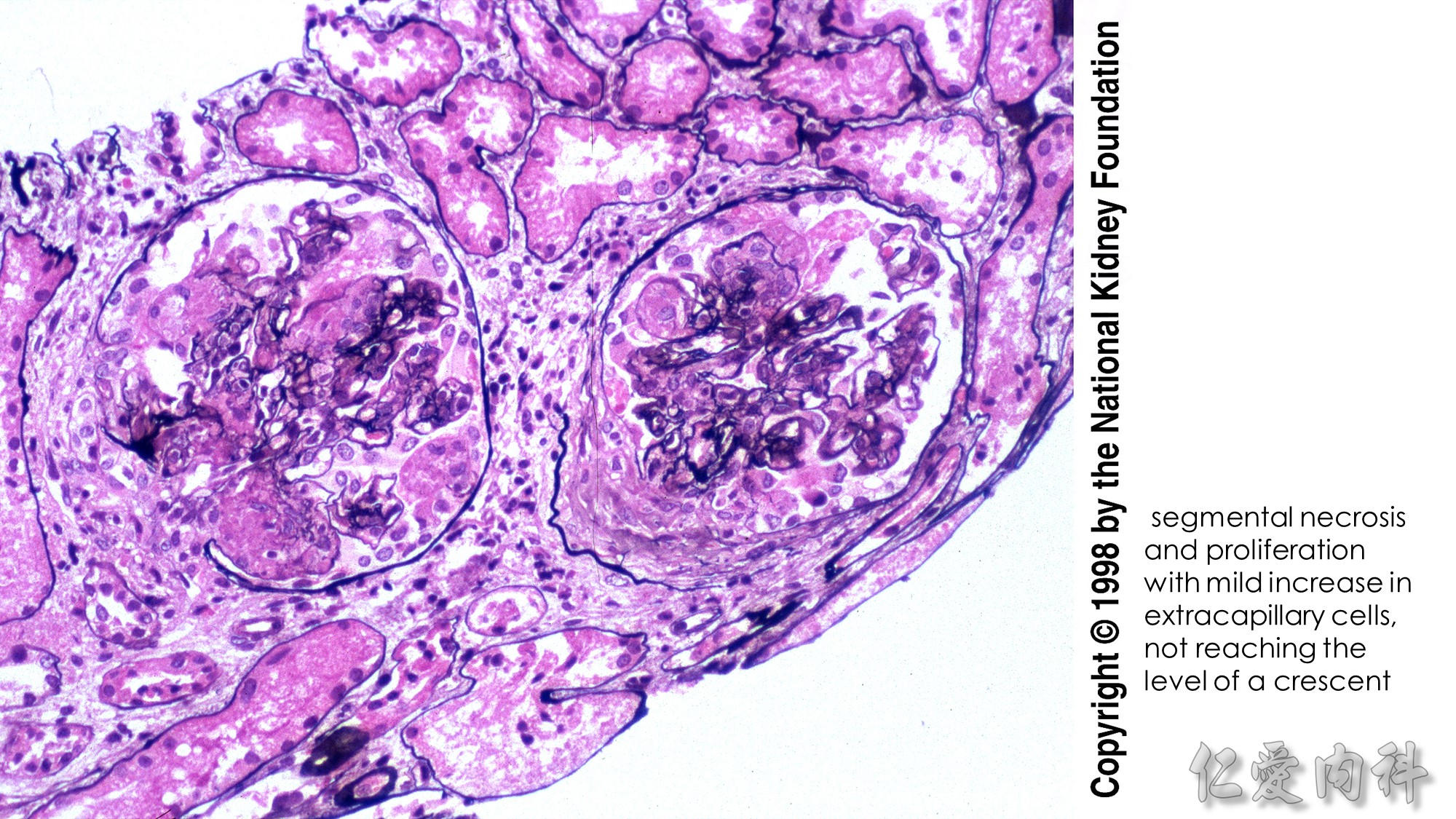
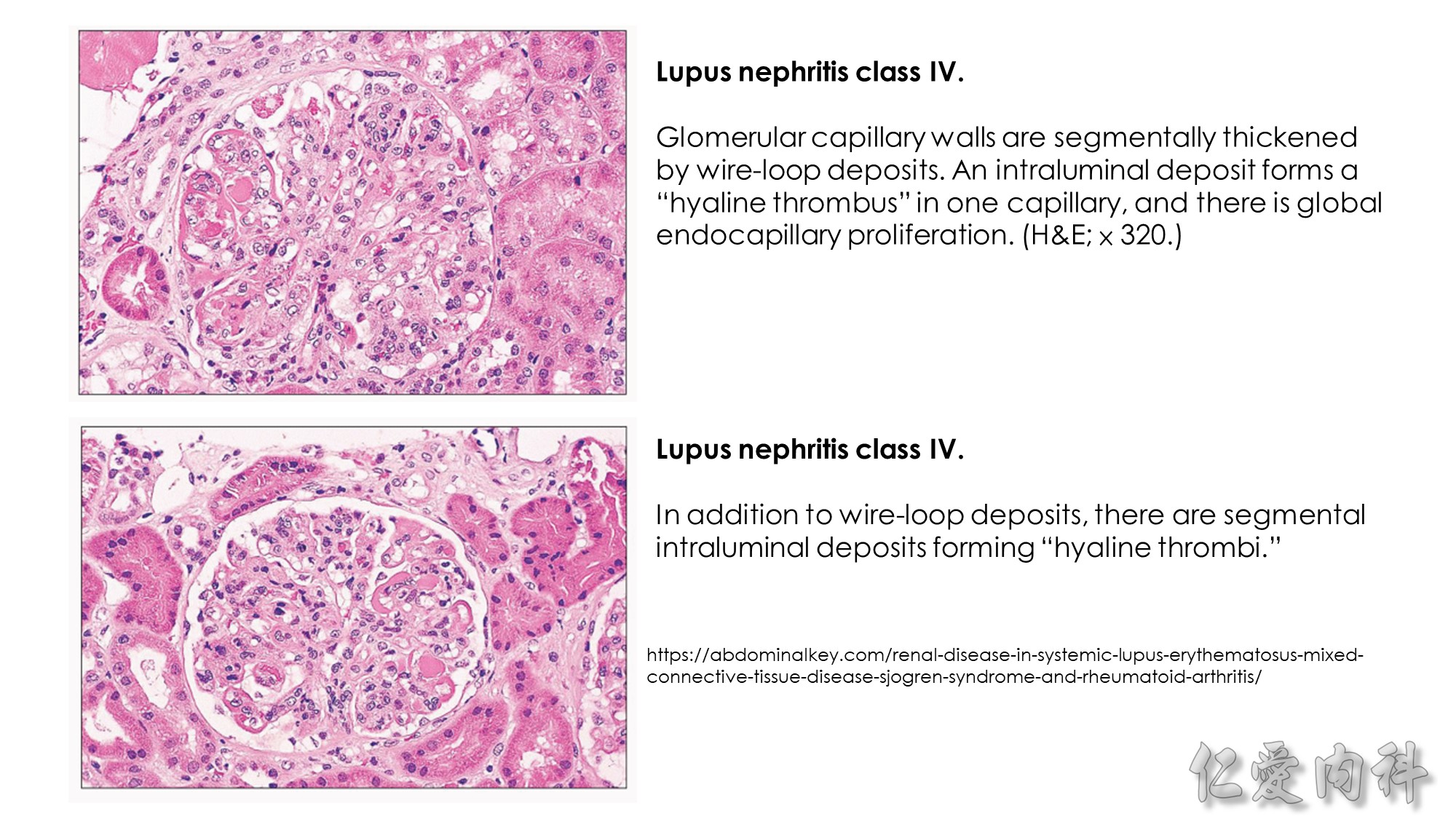
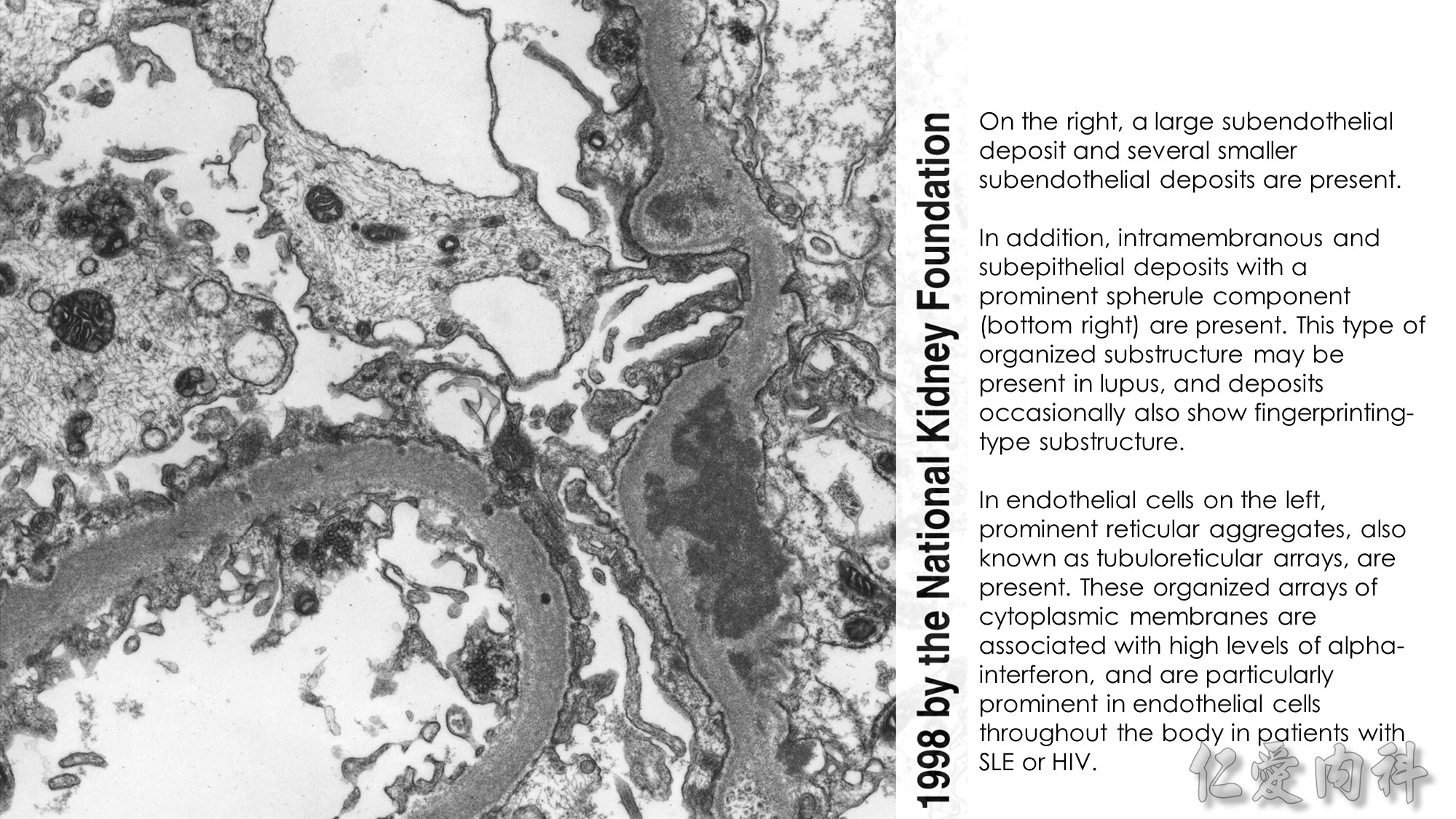
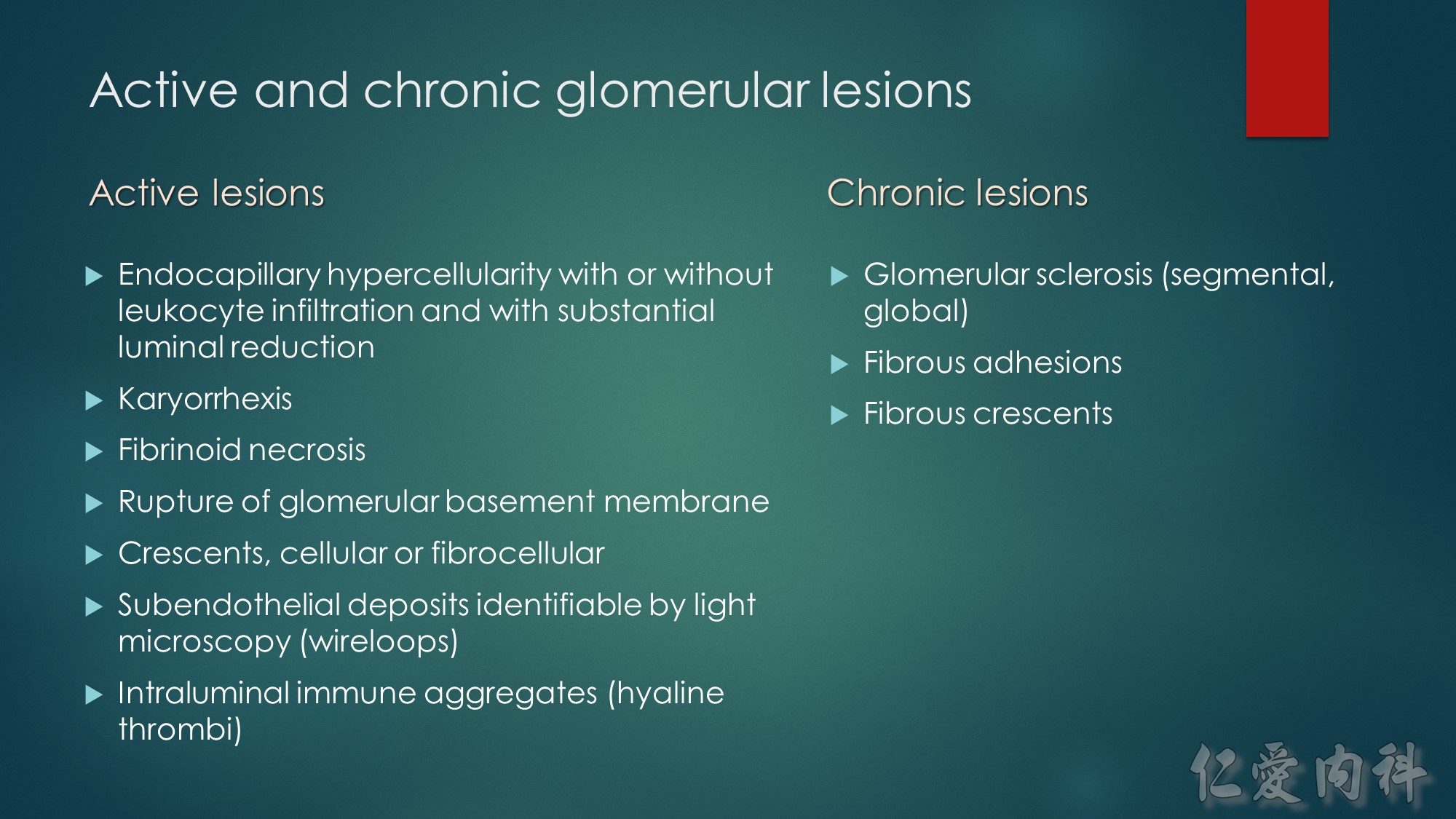
Drawings depicting the ultrastructural features of a single glomerular capillary affected by lupus glomerulonephritis: class I with mesangial immune deposits (black) but no mesangial cell (red) hypercellularity or influx of leukocytes; class II with mesangial immune deposits and mesangial cell hypercellularity but no influx of leukocytes; class III/IV (upper right) with mesangial and capillary influx of leukocytes; class III/IV (lower right) with subendothelial capillary wall immune deposits that can be seen by LM and mesangial but no capillary influx of leukocytes (dark green neutrophils and light green monocytes/macrophages); class III/IV D V with an influx of leukocytes and numerous subepithelial immune deposits in addition to subendothelial deposits; and class V with numerous subepithelial immune deposits but no influx of leukocytes (podocyte = outer green cell, endothelial cell =yellow cell, mesangial cell = red cell, neutrophil = green cell with segmented nucleus, monocyte/macrophage=light green cell)
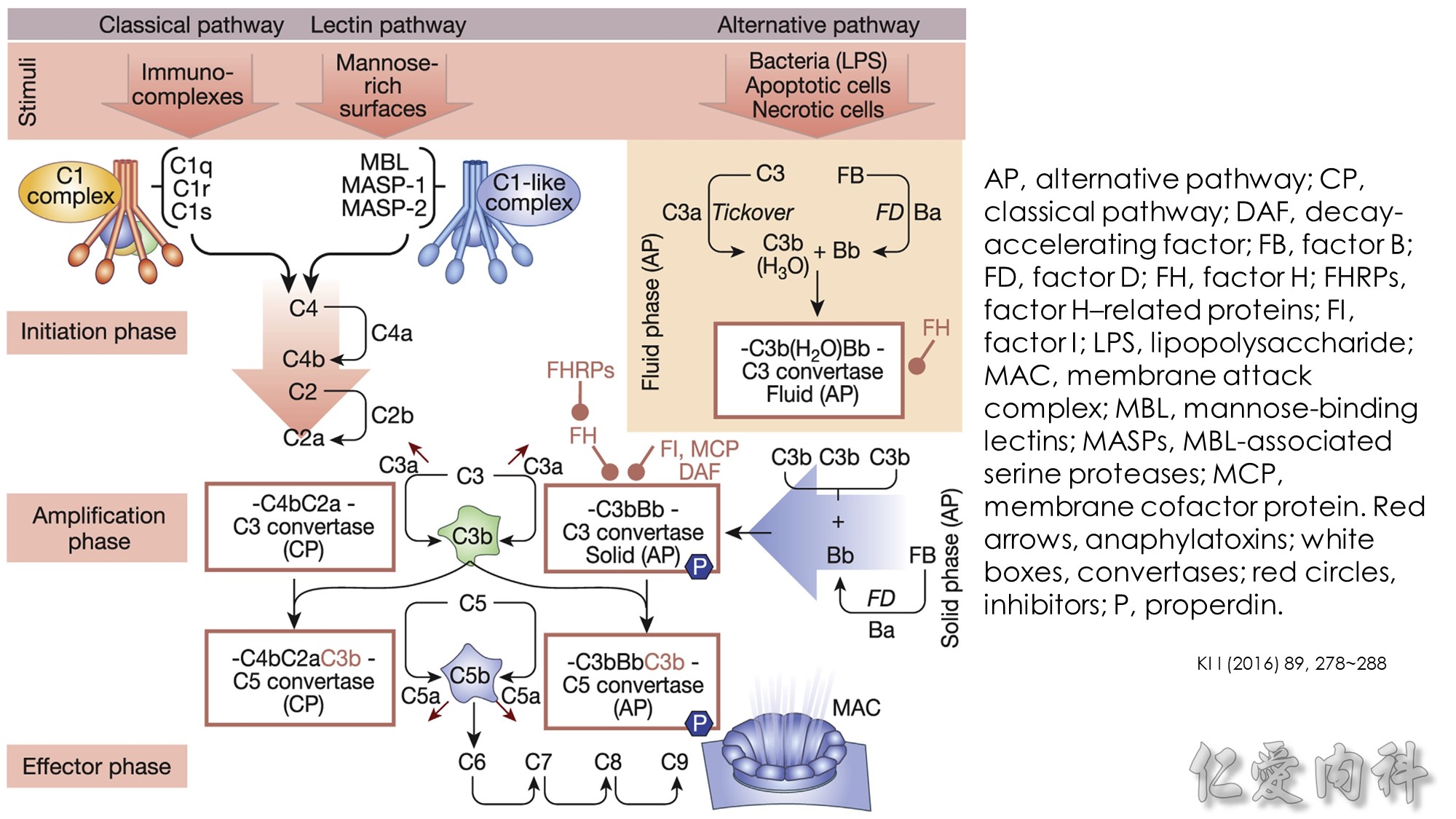
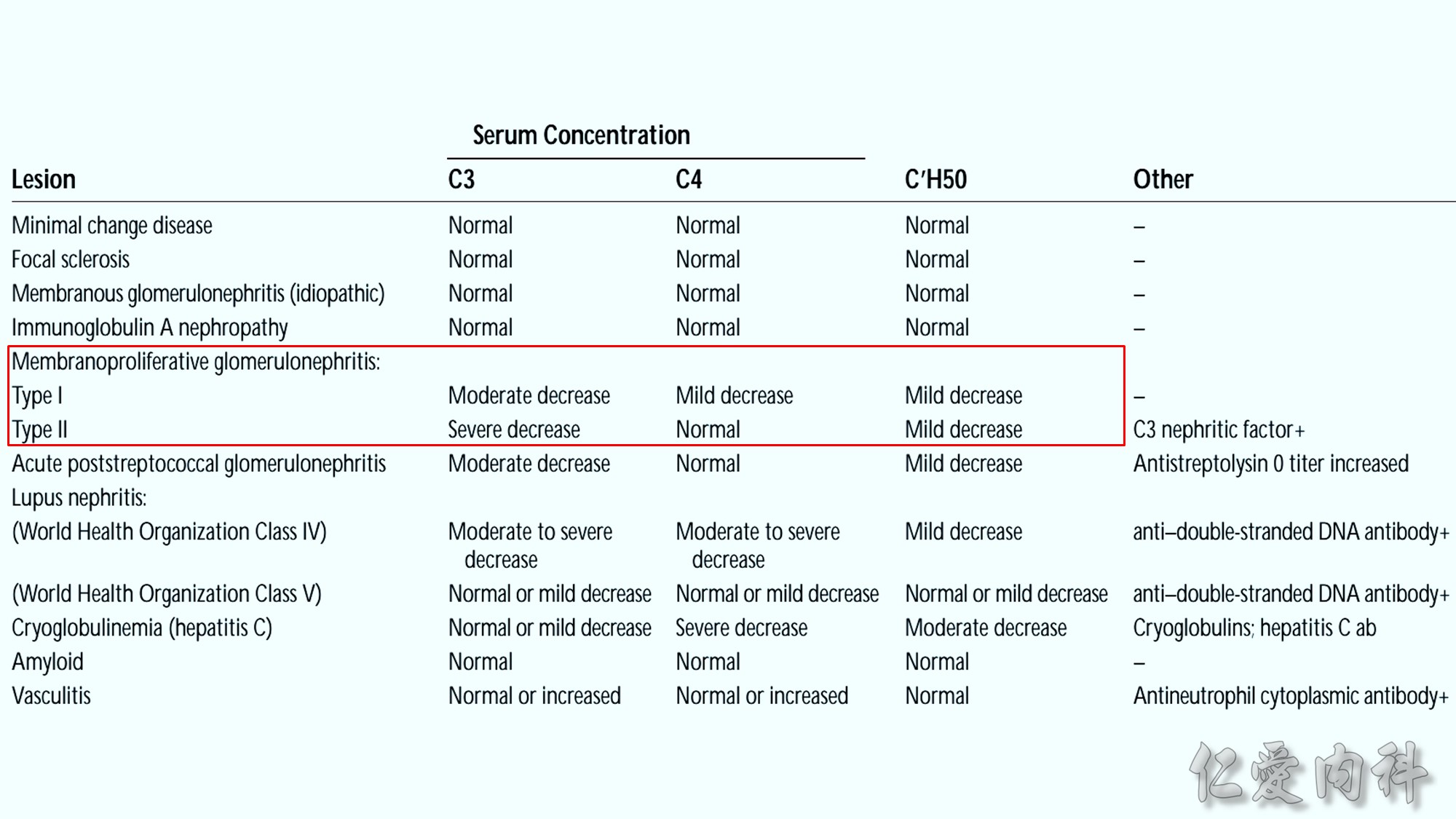
CH50 是先測定需要多少患者的血清才能令定量的綿羊血溶血 50%,藉此回推患者的補體活性。若需要的血清愈多,代表患者血清所含的補體量愈少 (或活性愈差)。
CH50 的評估範圍包括標準路徑 (Classical pathway; C1 ~ C4) 及終端路徑 (Terminal pathway; C5 ~ C9) 的所有補體及輔助蛋白。若先天性缺乏 C1 ~ C9 及其控制蛋白,或是補體活性不足時,CH50 的測定結果皆偏低。
自體免疫疾病、感染過程、惡性腫瘤等,會引發體內的免疫反應,而在抗原抗體的結合過程中消秏掉補體,導致 CH50 降低。例如紅斑性狼瘡患者的CH50 都偏低,就是典型常見的例子。
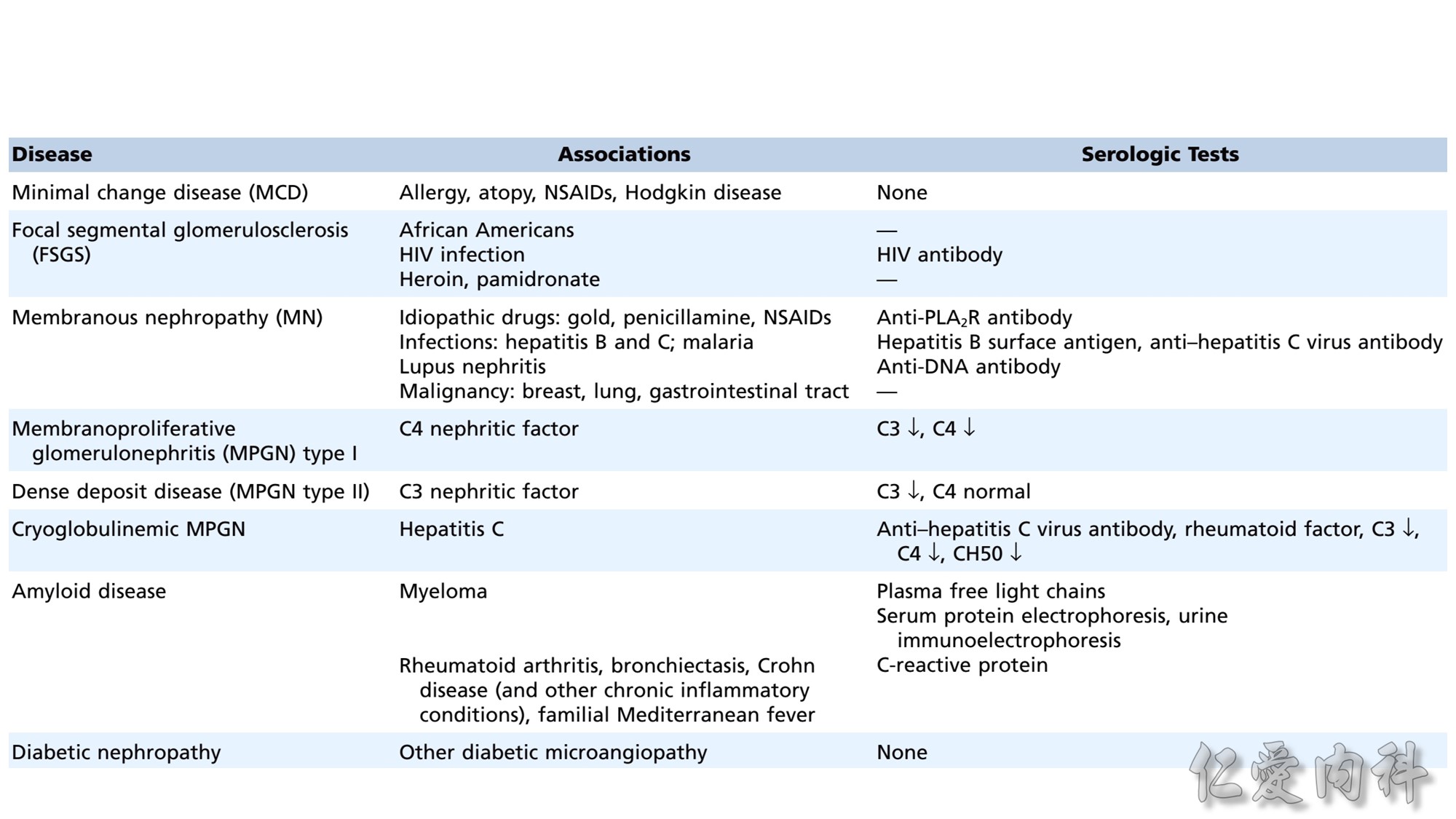
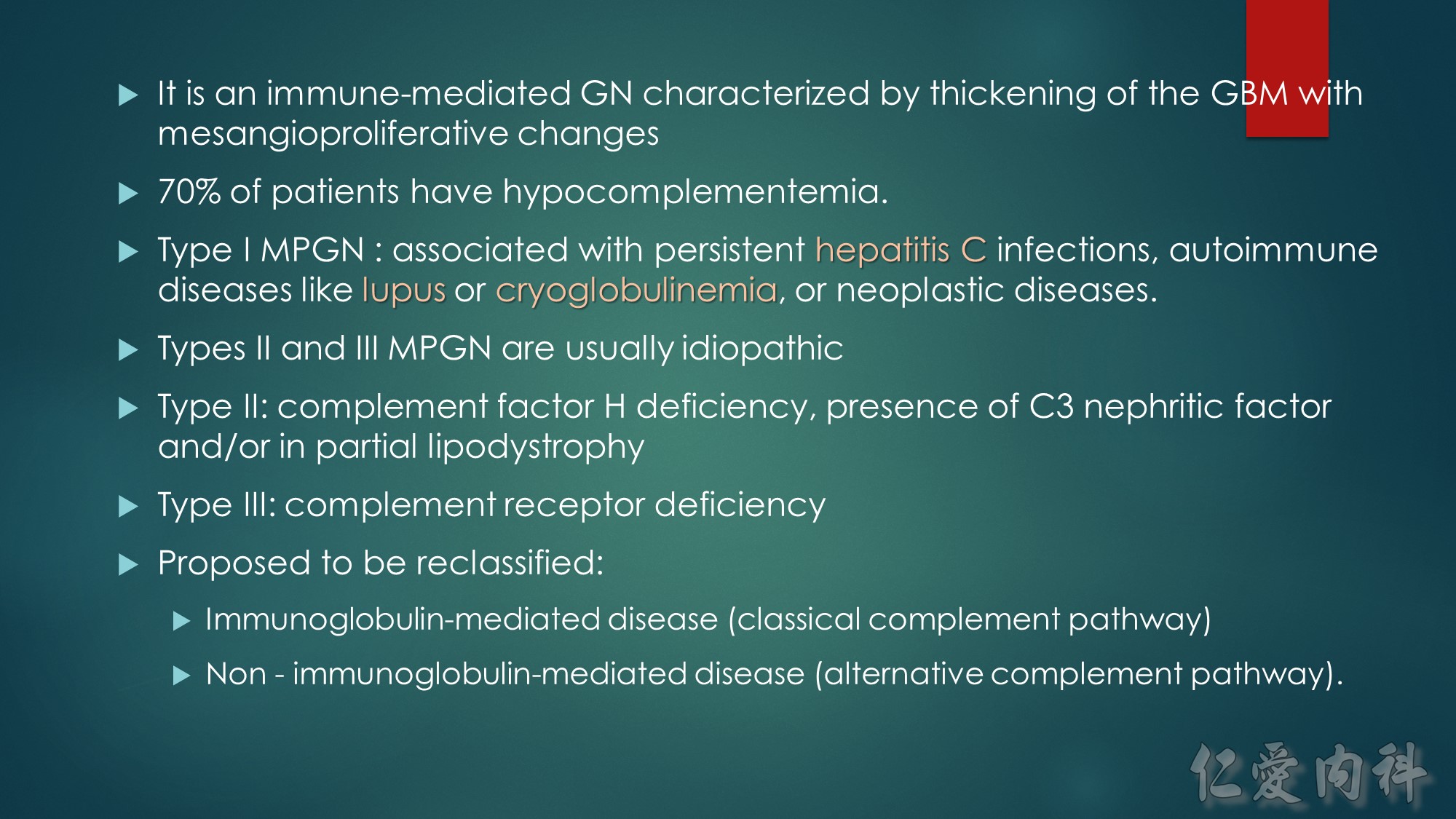
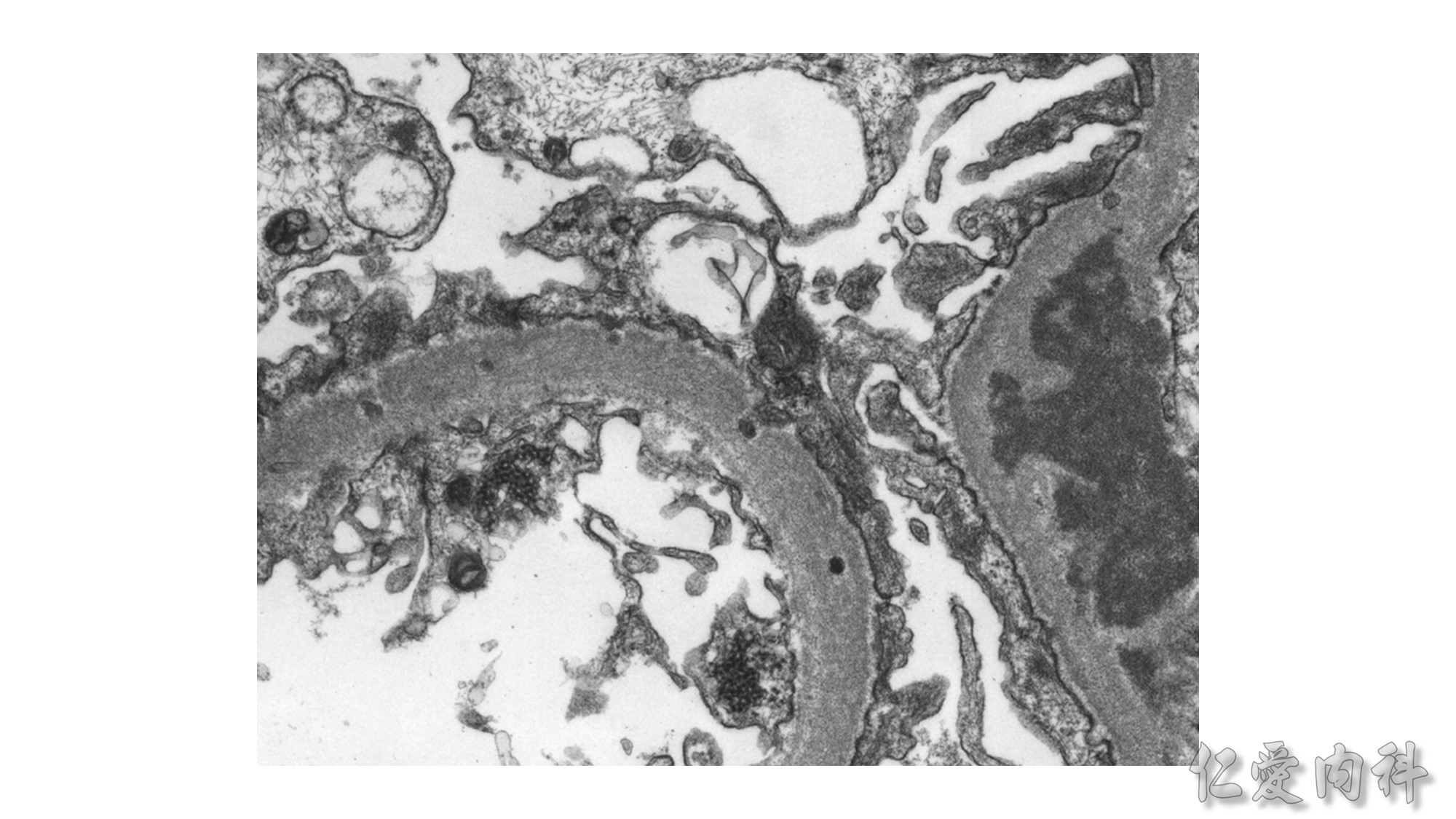
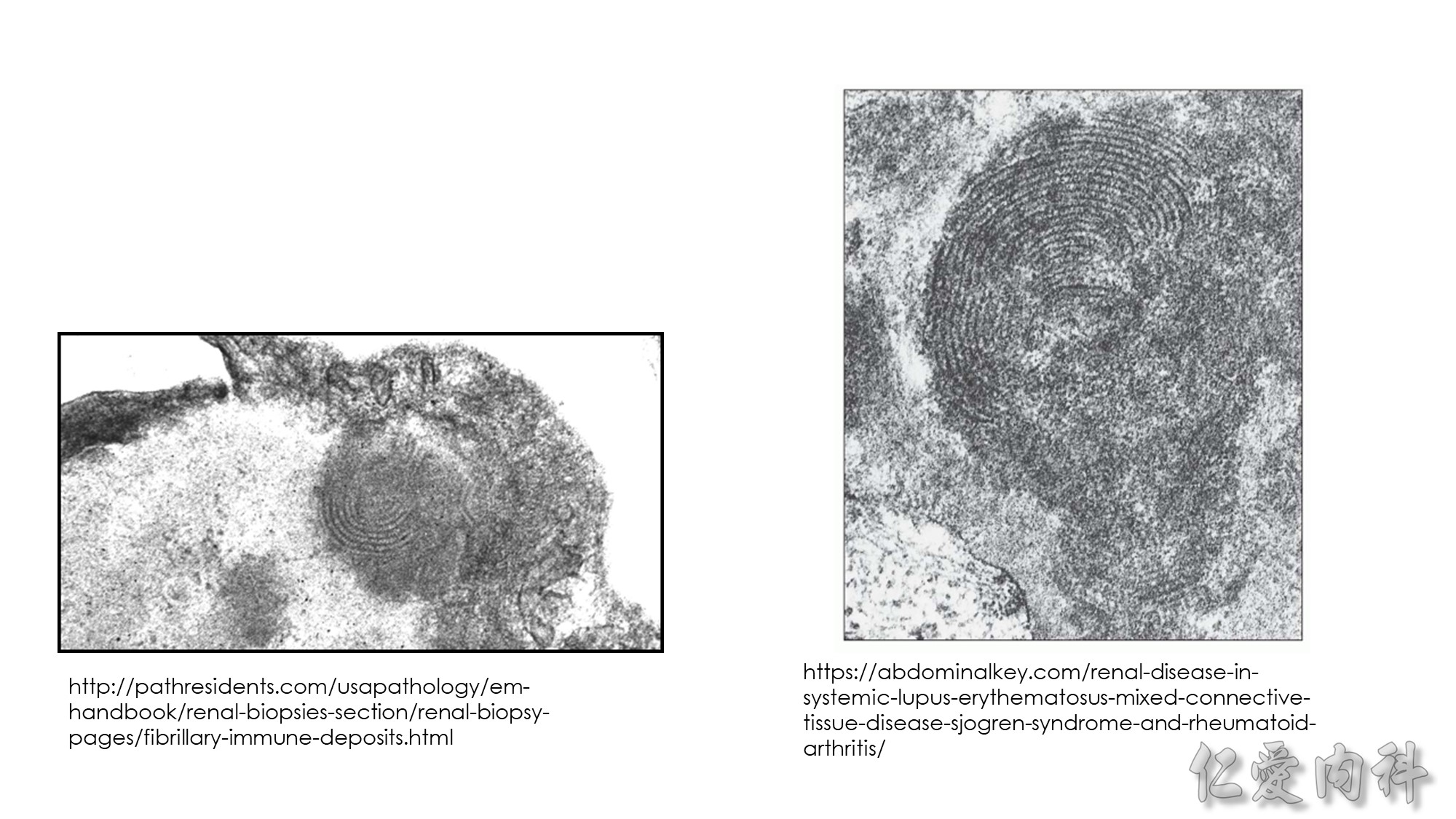
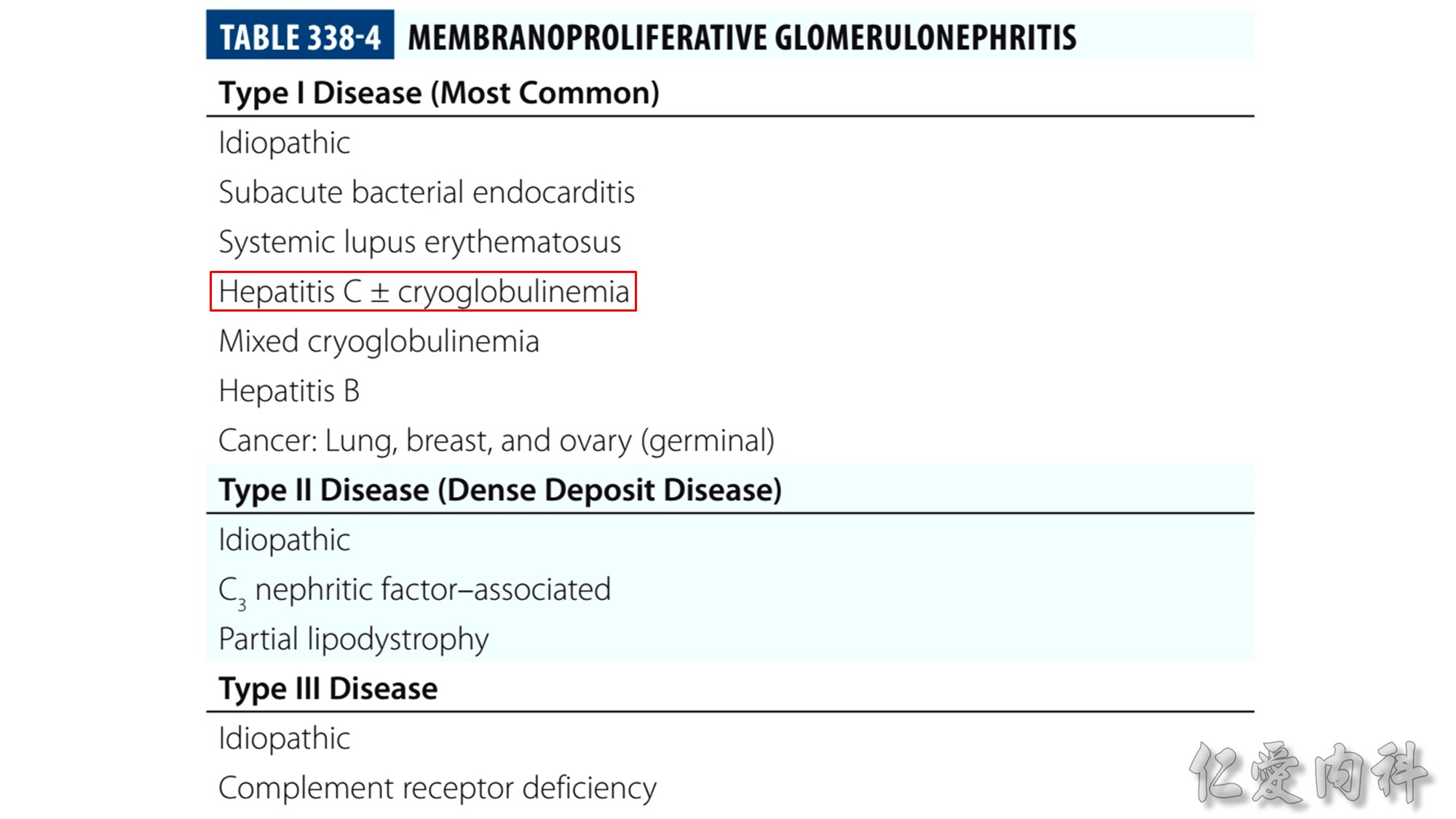
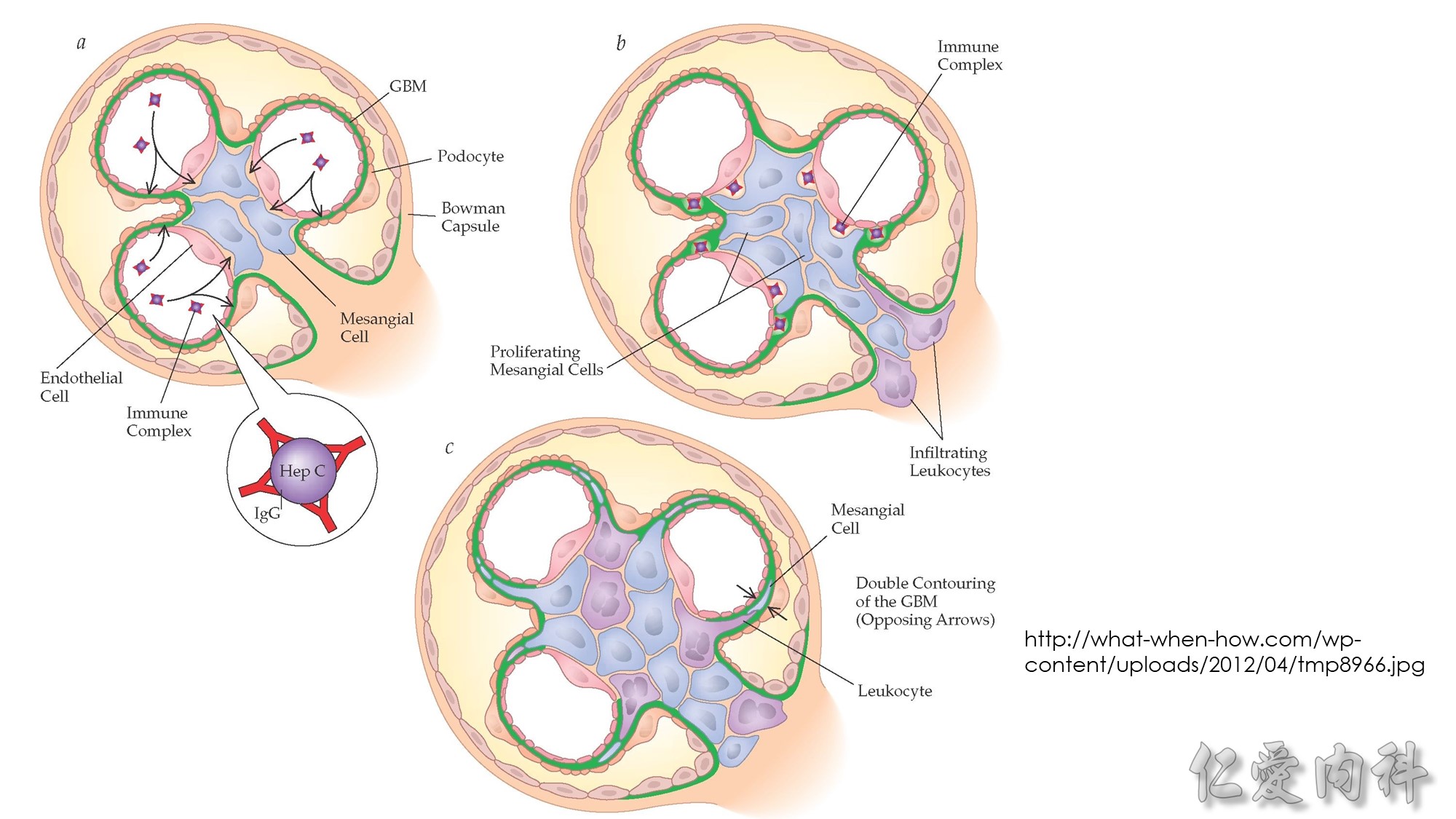
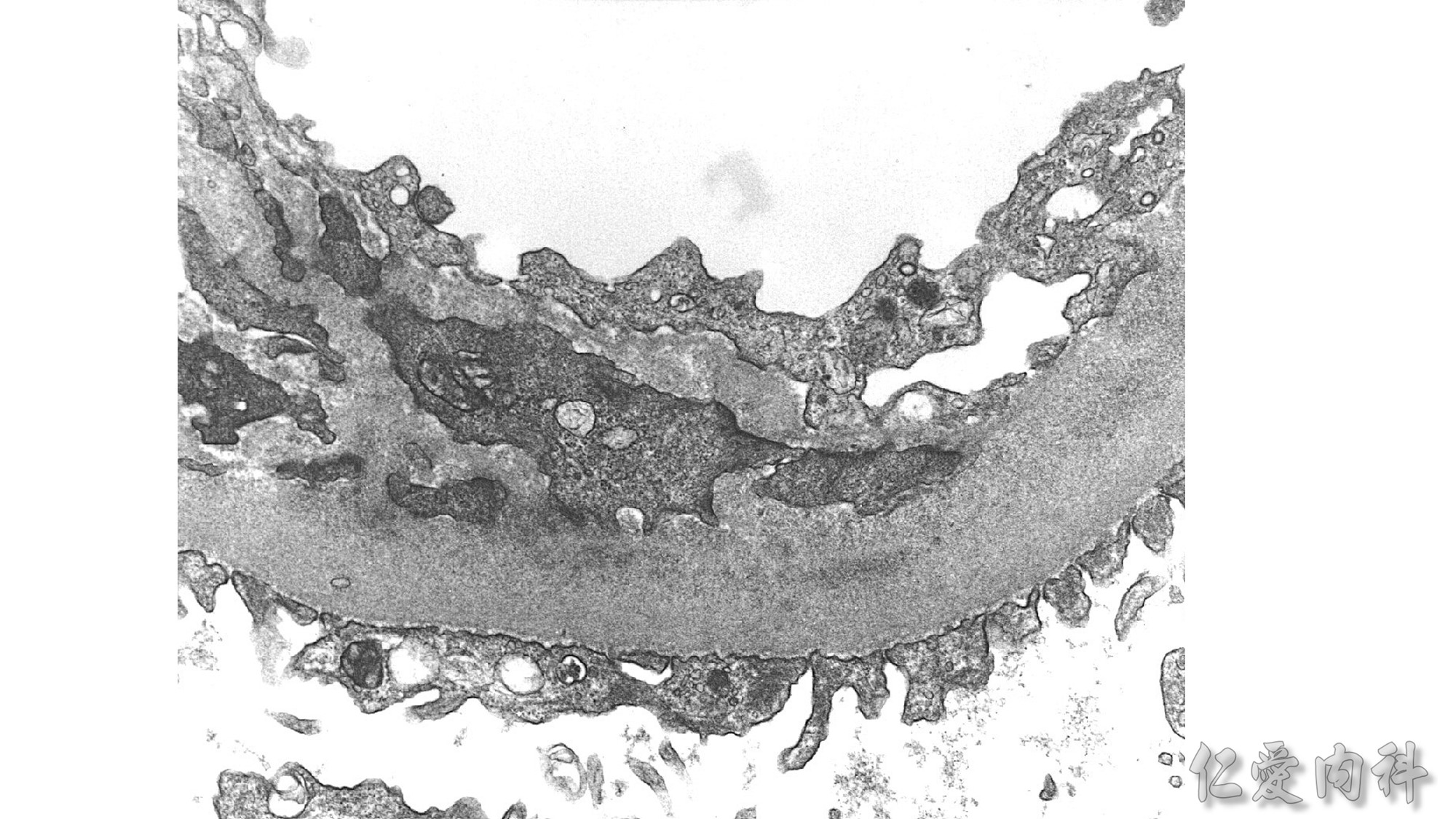
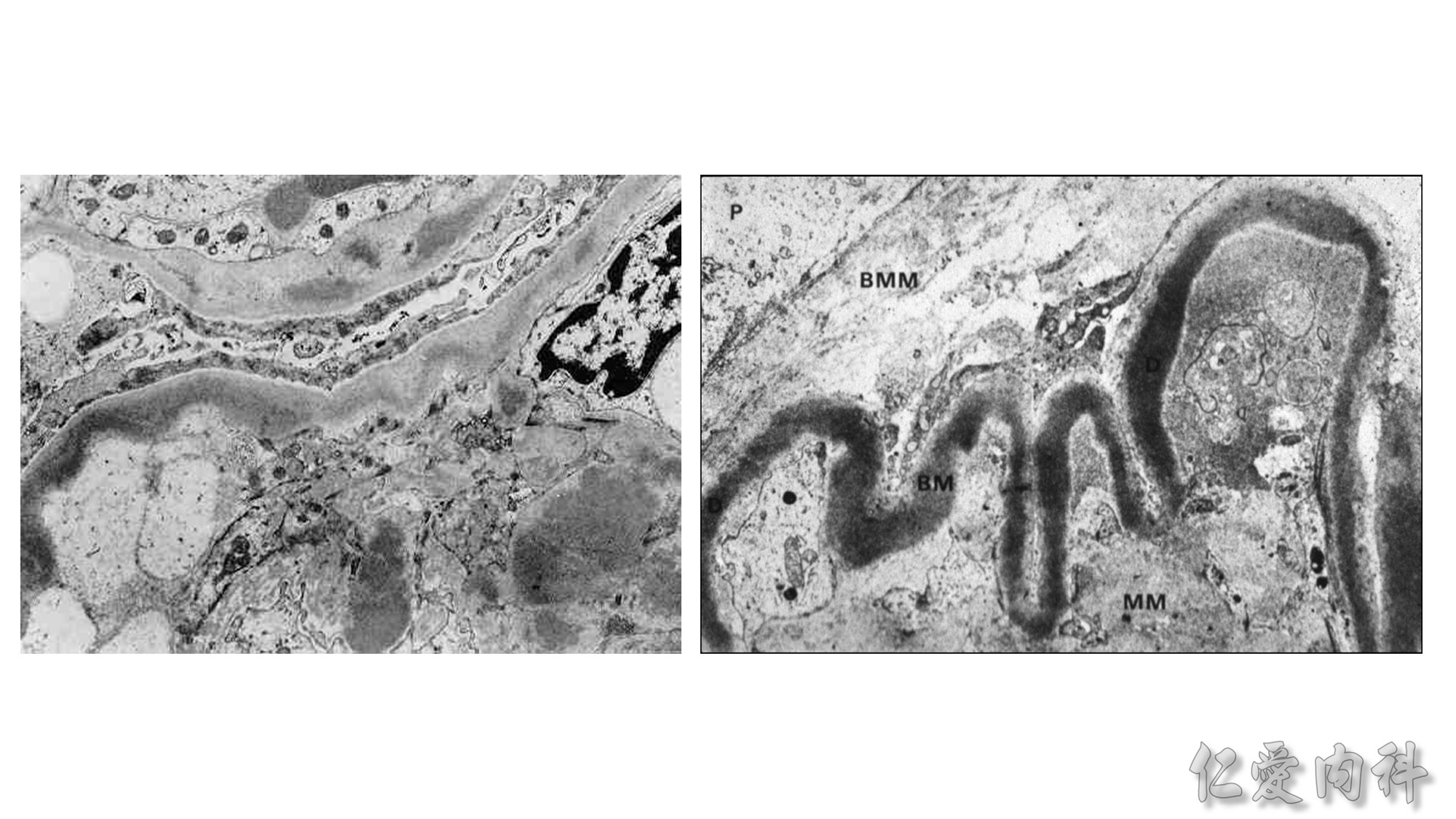
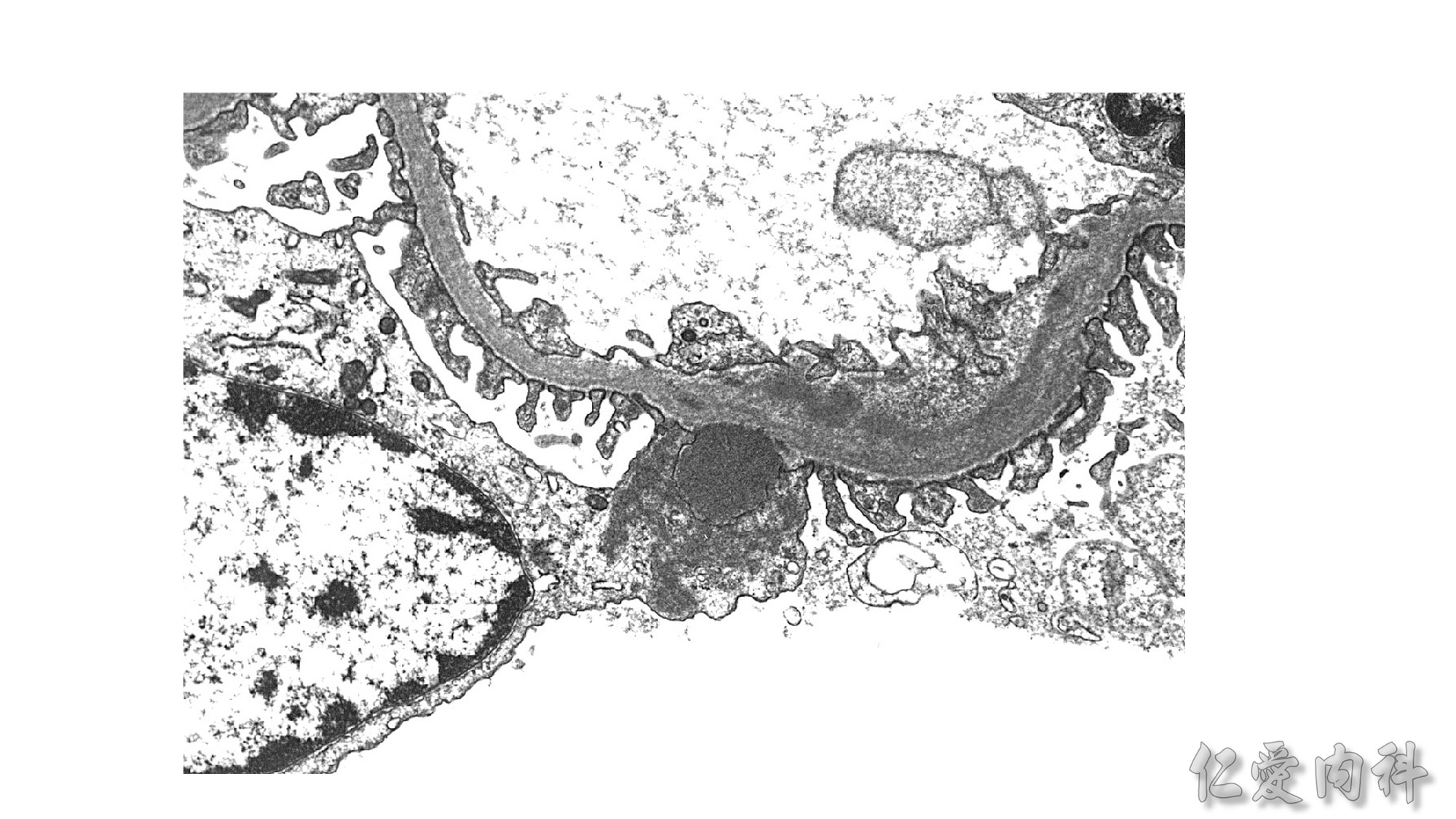
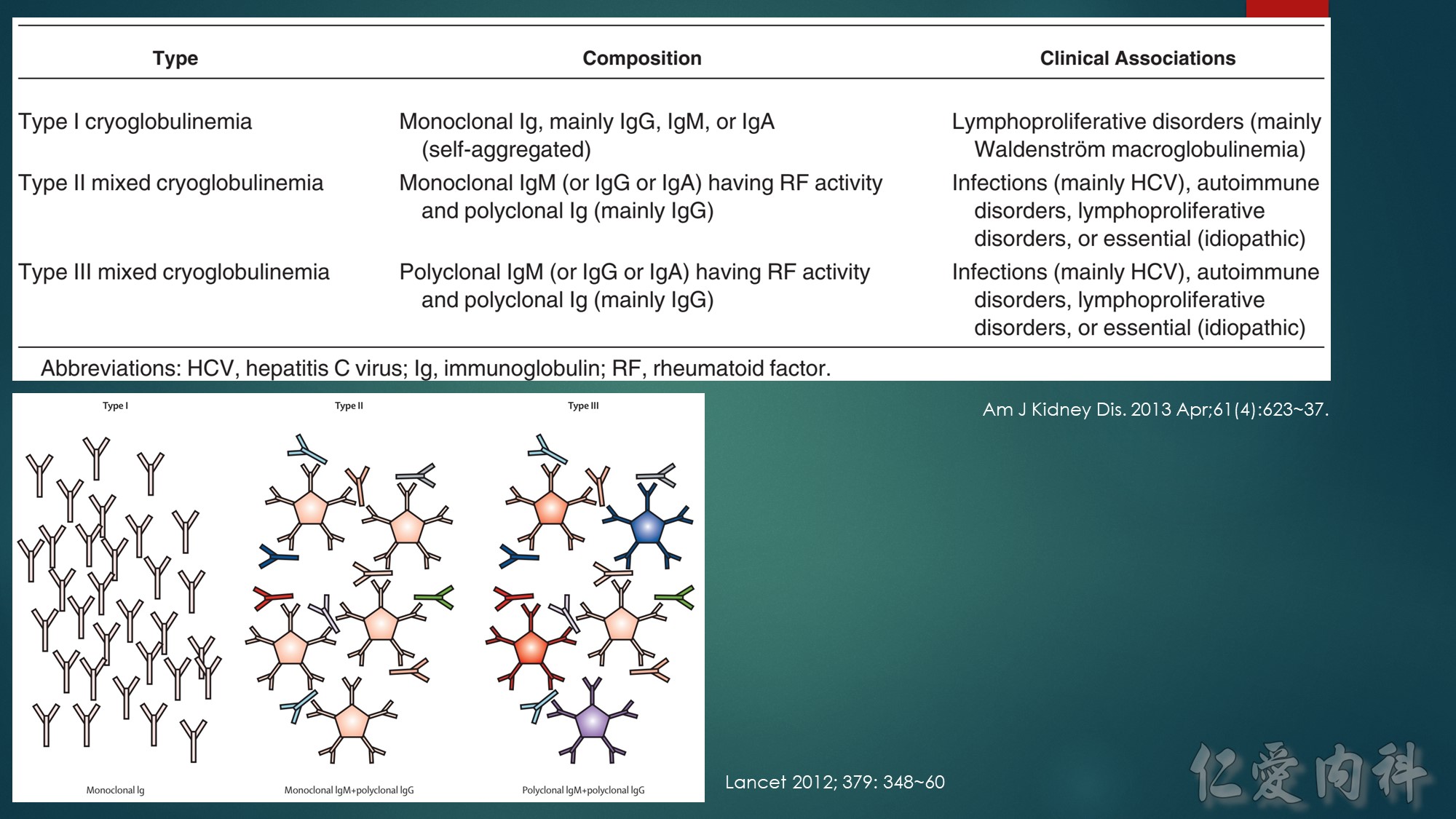
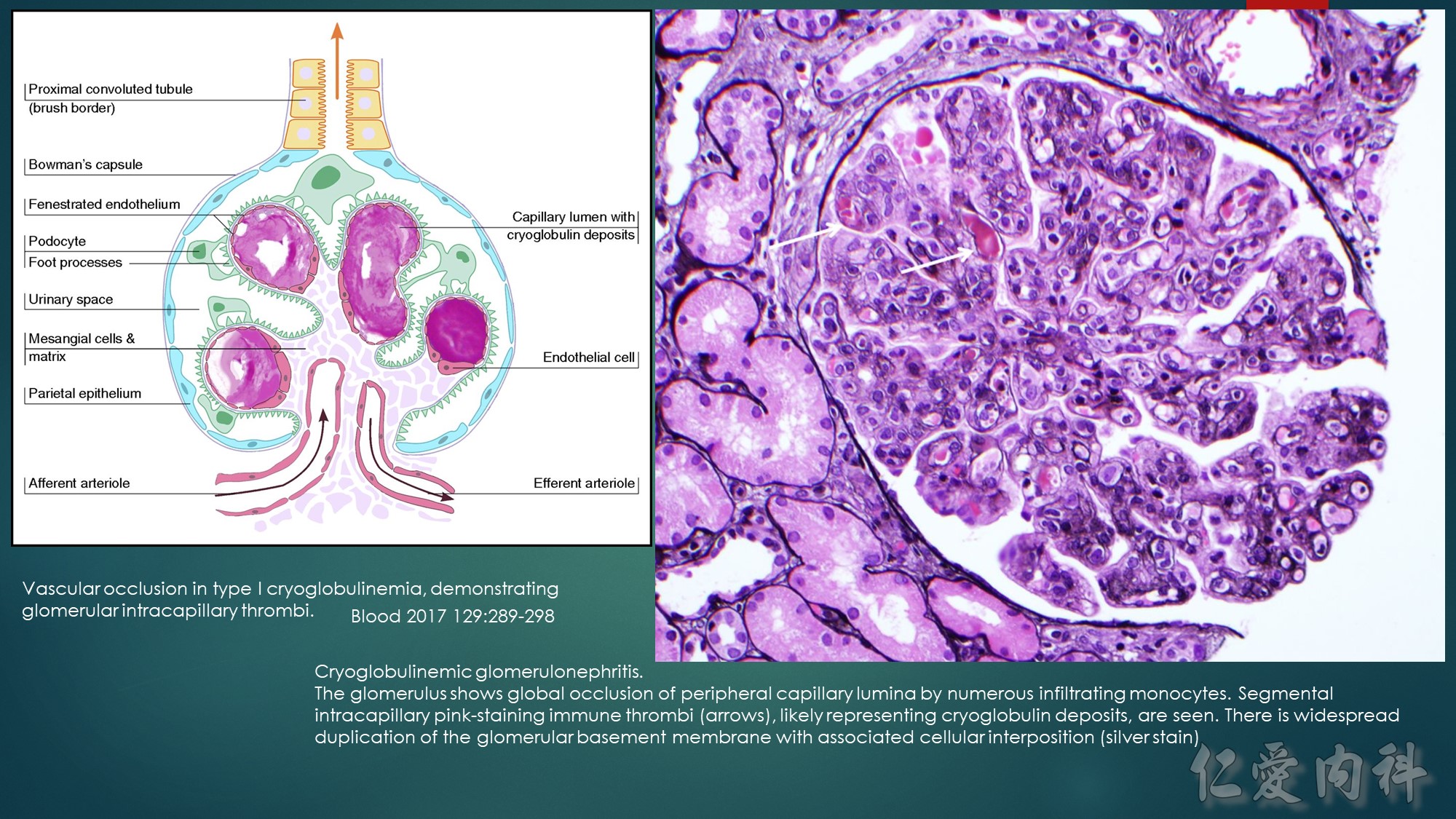
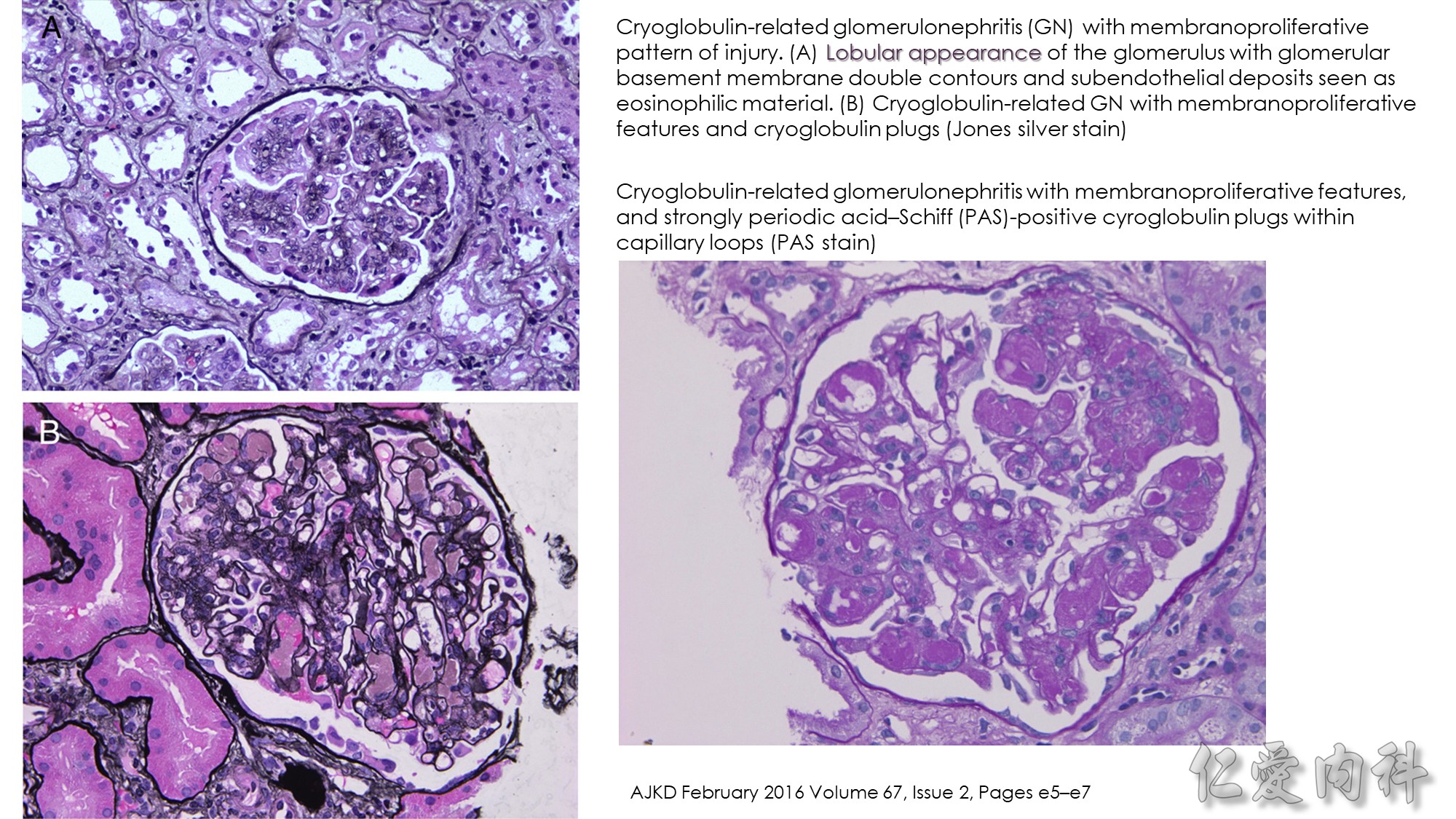
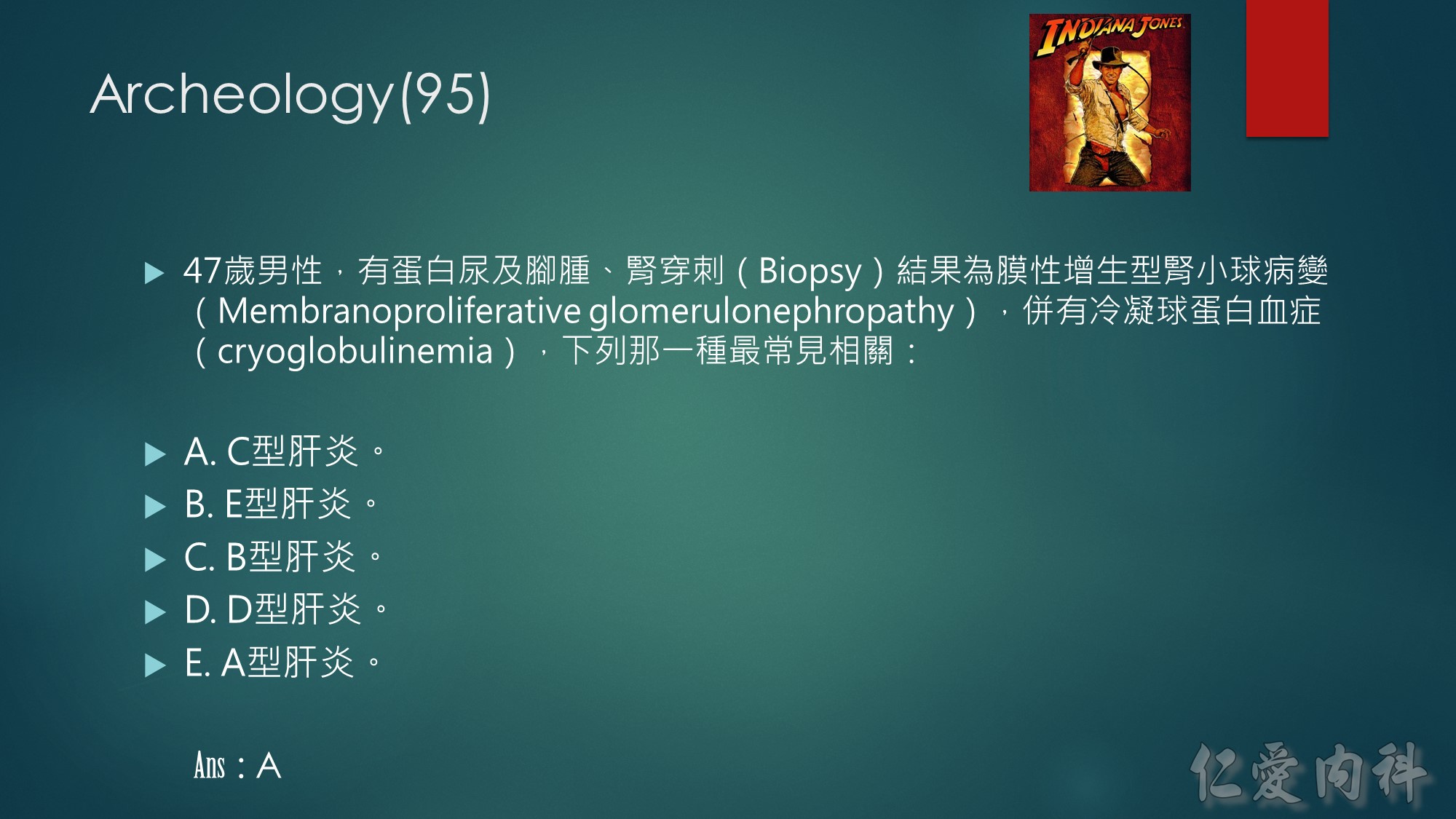
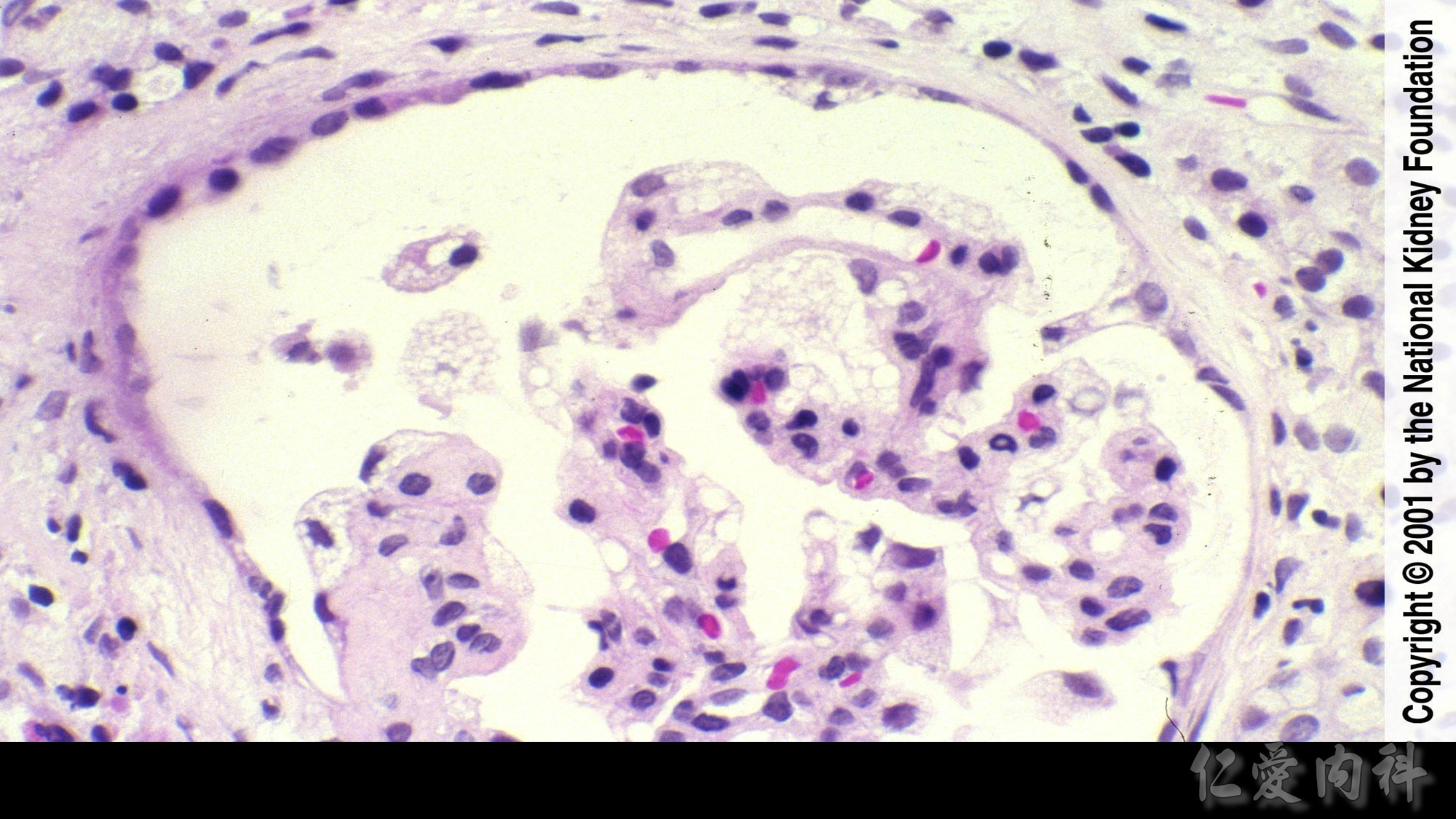
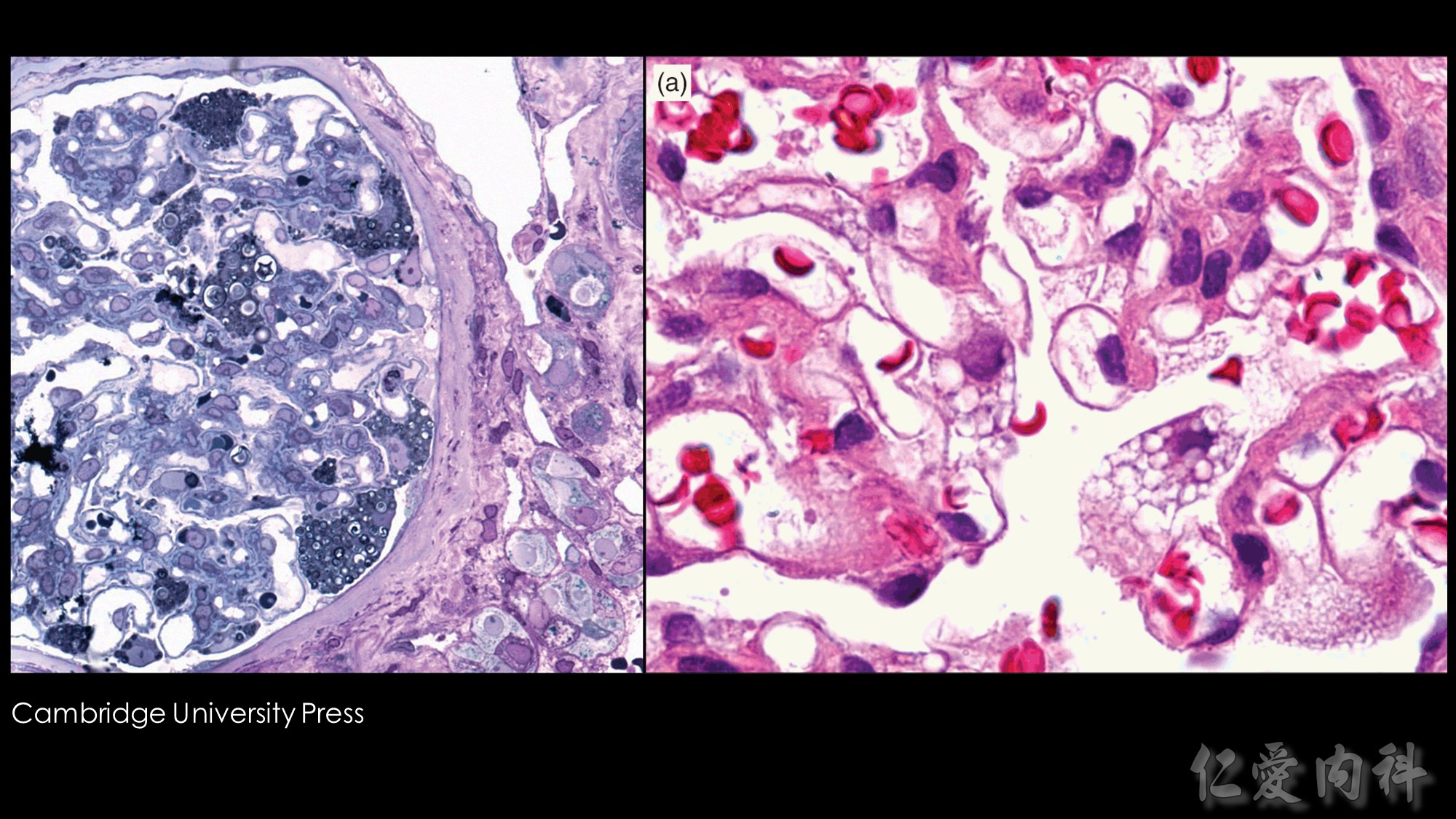
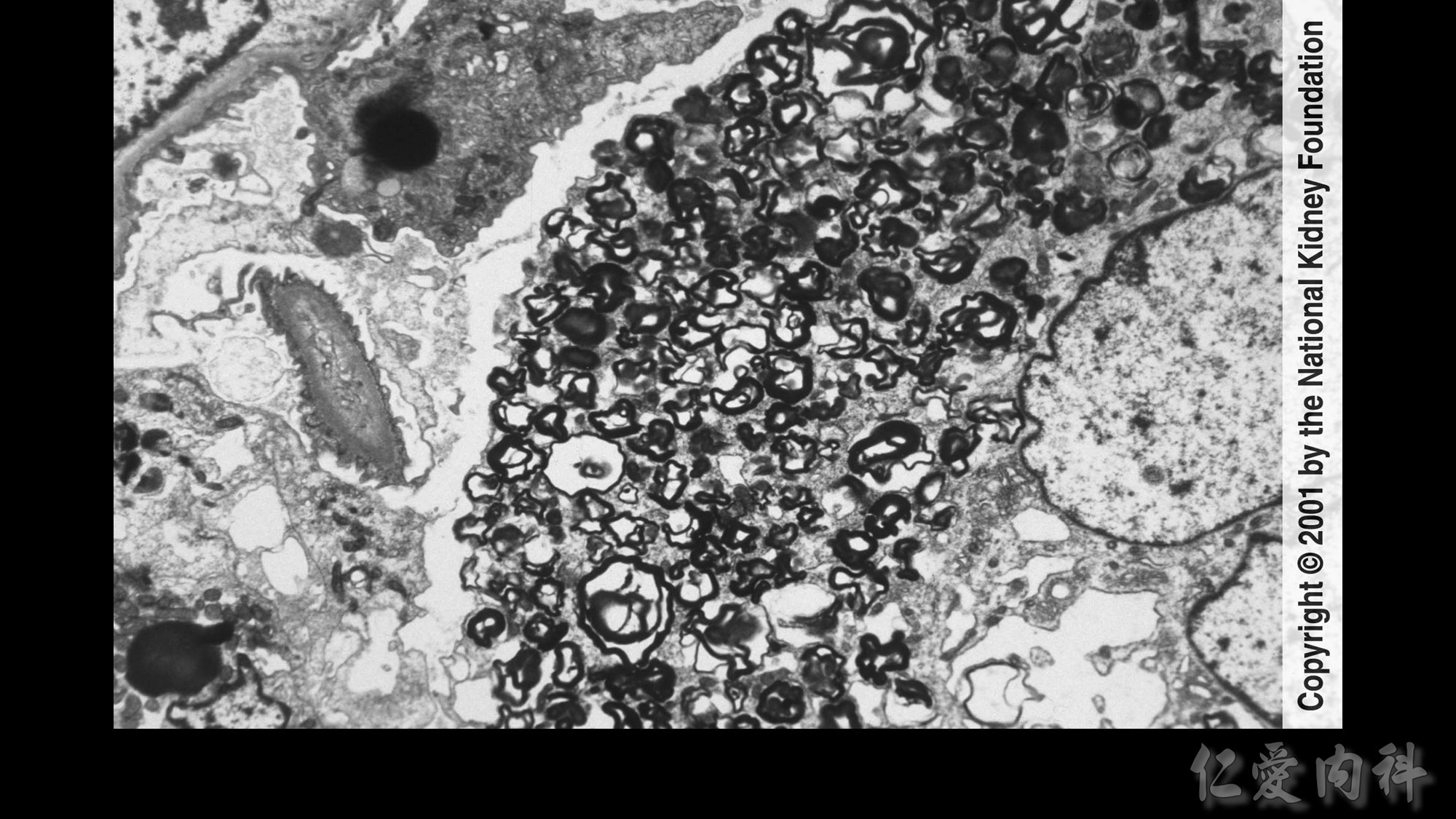
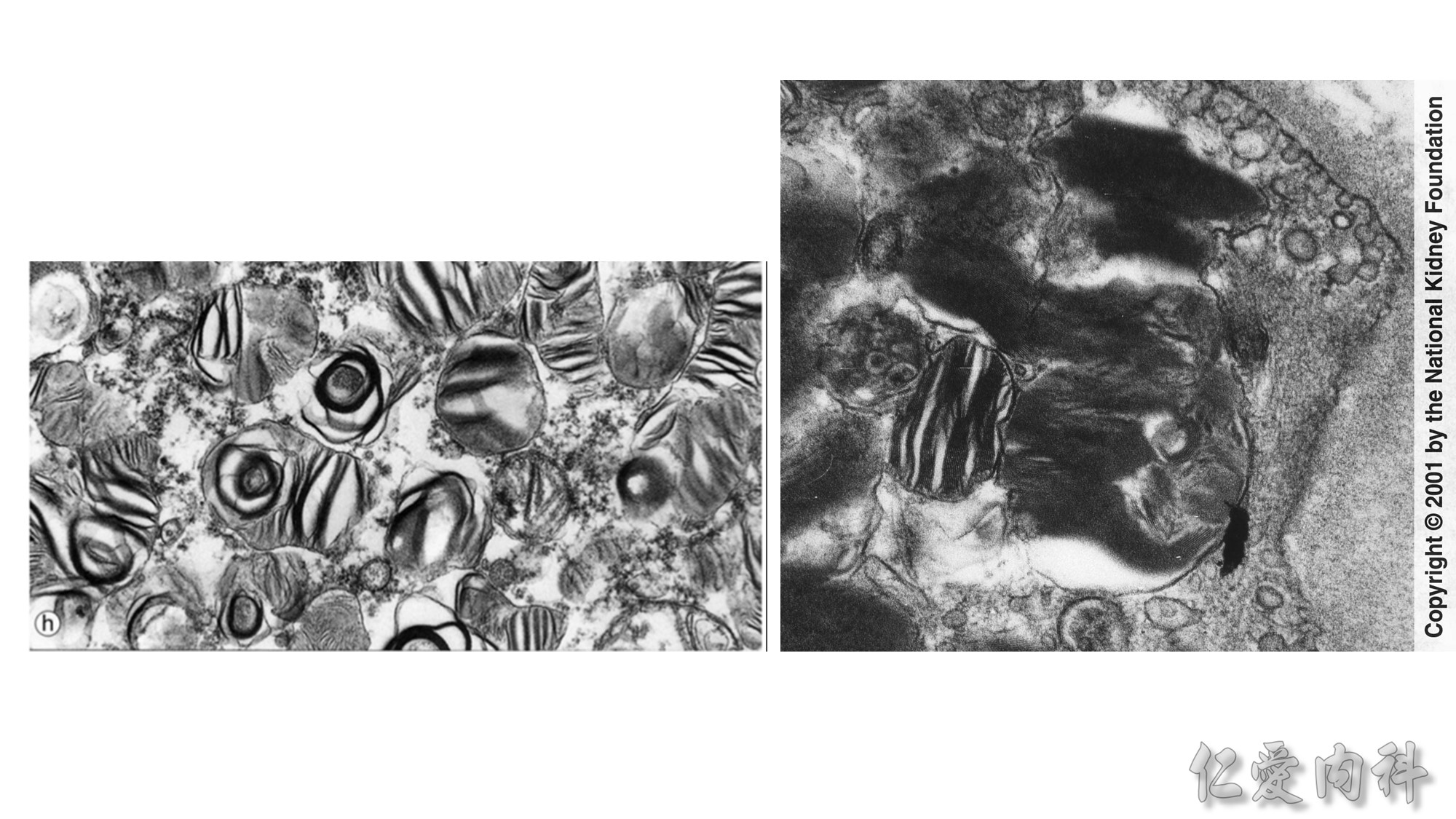
Cryoglobulinemic MPGN may appear histologically identical to
MPGN type I. However, the cryoprecipitates can occasionally be
observed by light microscopy as intracapillary hyaline-like globules, and there is often a more pronounced infiltration of
macrophages within capillary lumina. EM may also show highly
organized microtubular or finely fibrillar structures consisting of the
precipitated cryoglobulins

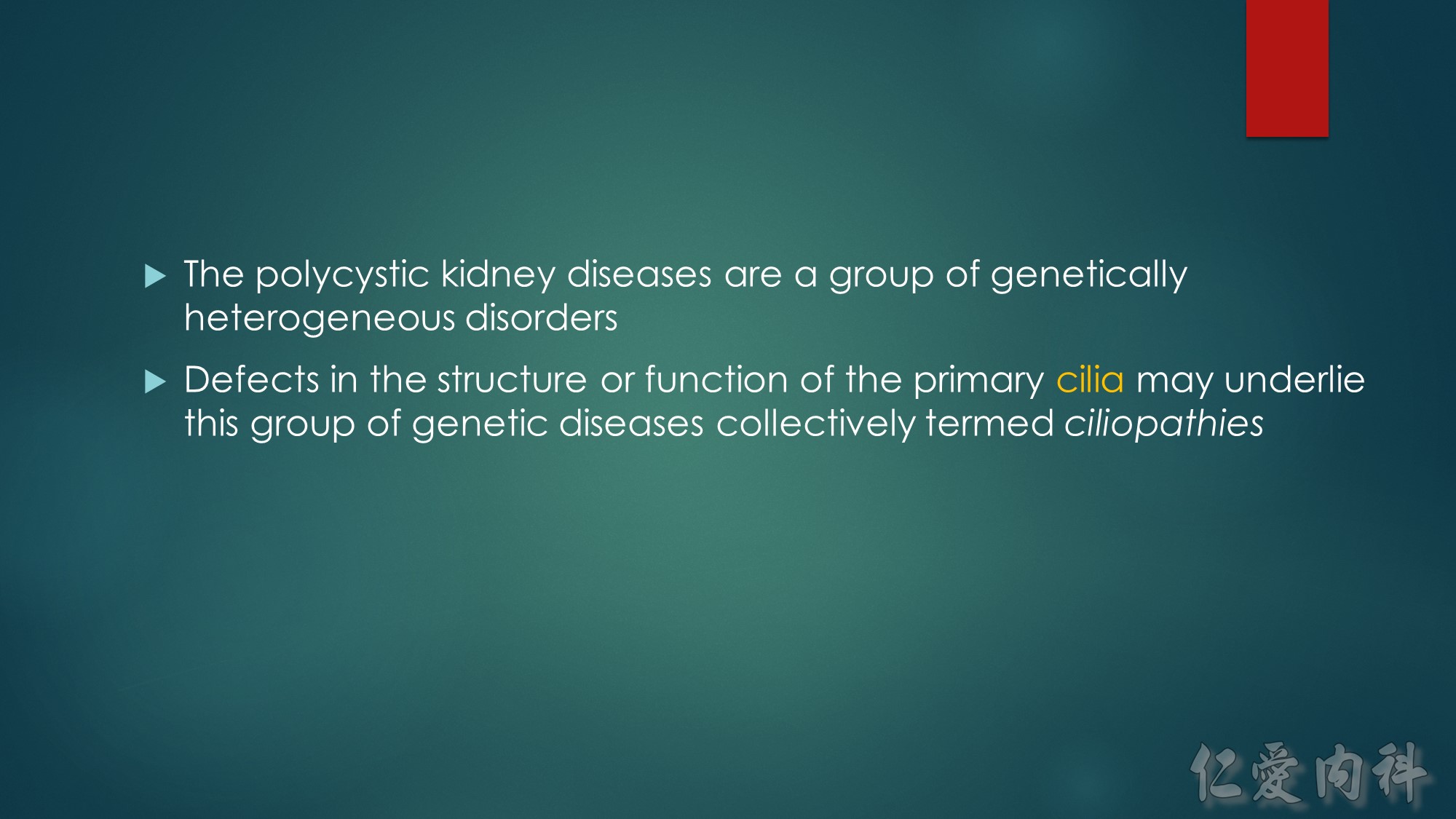
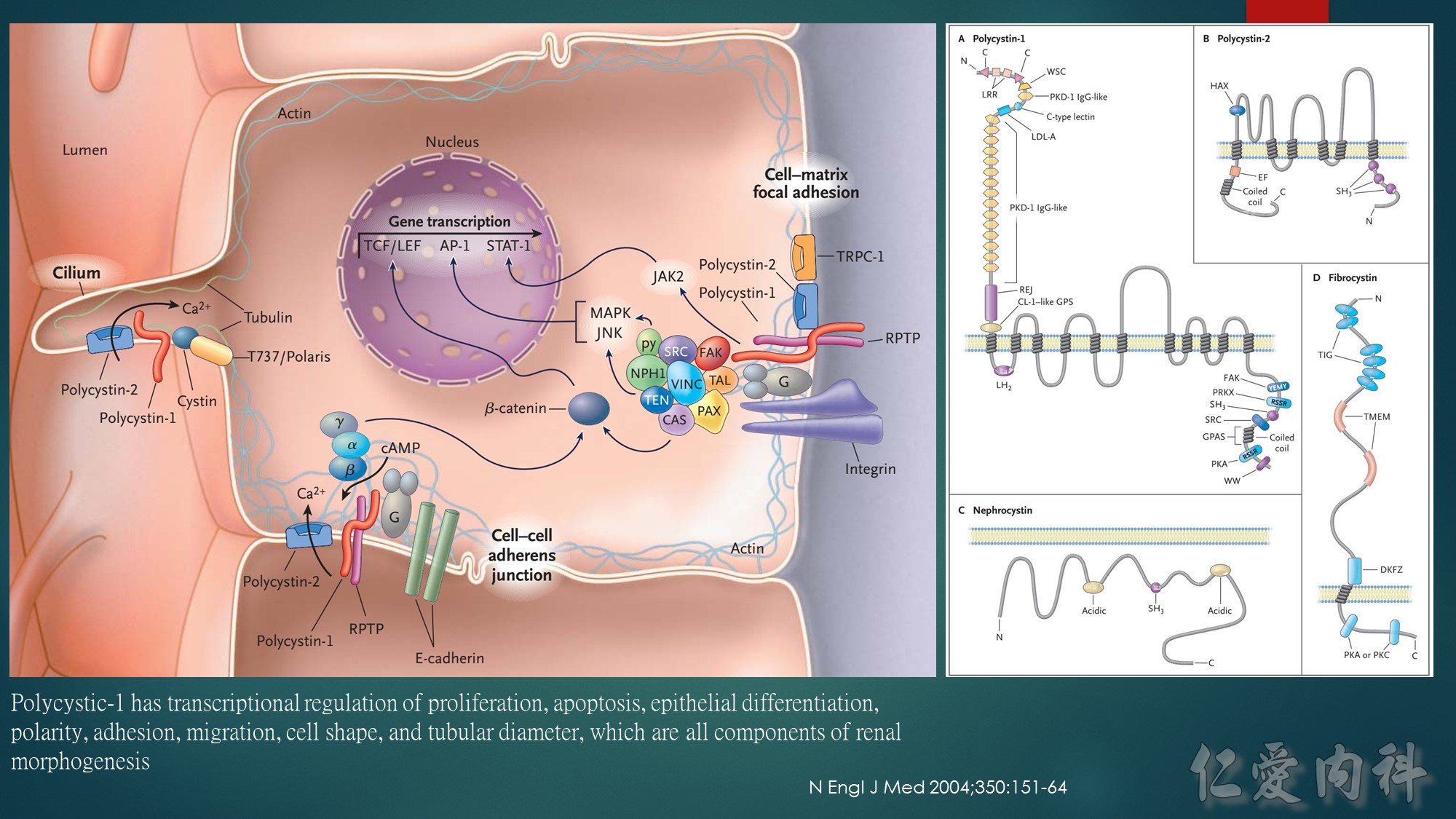
Left. A scheme of the primary cilium. Primary cilia share a “9+0” organization of microtubule doublets. Proteins are transported into the cilium by motor protein kinesin 2 and transported out of the cilium by dynein. The cilium is connected to the basal body through the transition zone. Middle. Topology of autosomal dominant polycystic kidney disease (ADPKD) and autosomal recessive polycystic kidney disease (ARPKD) proteins polycystin-1, polycystin-2, and fibrocystin/polyductin (FPC) are shown. PC1 also interacts with other proteins such as components of the BBSome and NPHP1. PC2 and FPC both interact with kinesin 2 (KIF 3A/B). Localization of disease proteins in the cilium, the transition zone, and the basal body is color coded. Right. Potential disease mechanisms due to cilium-mediated signaling events.
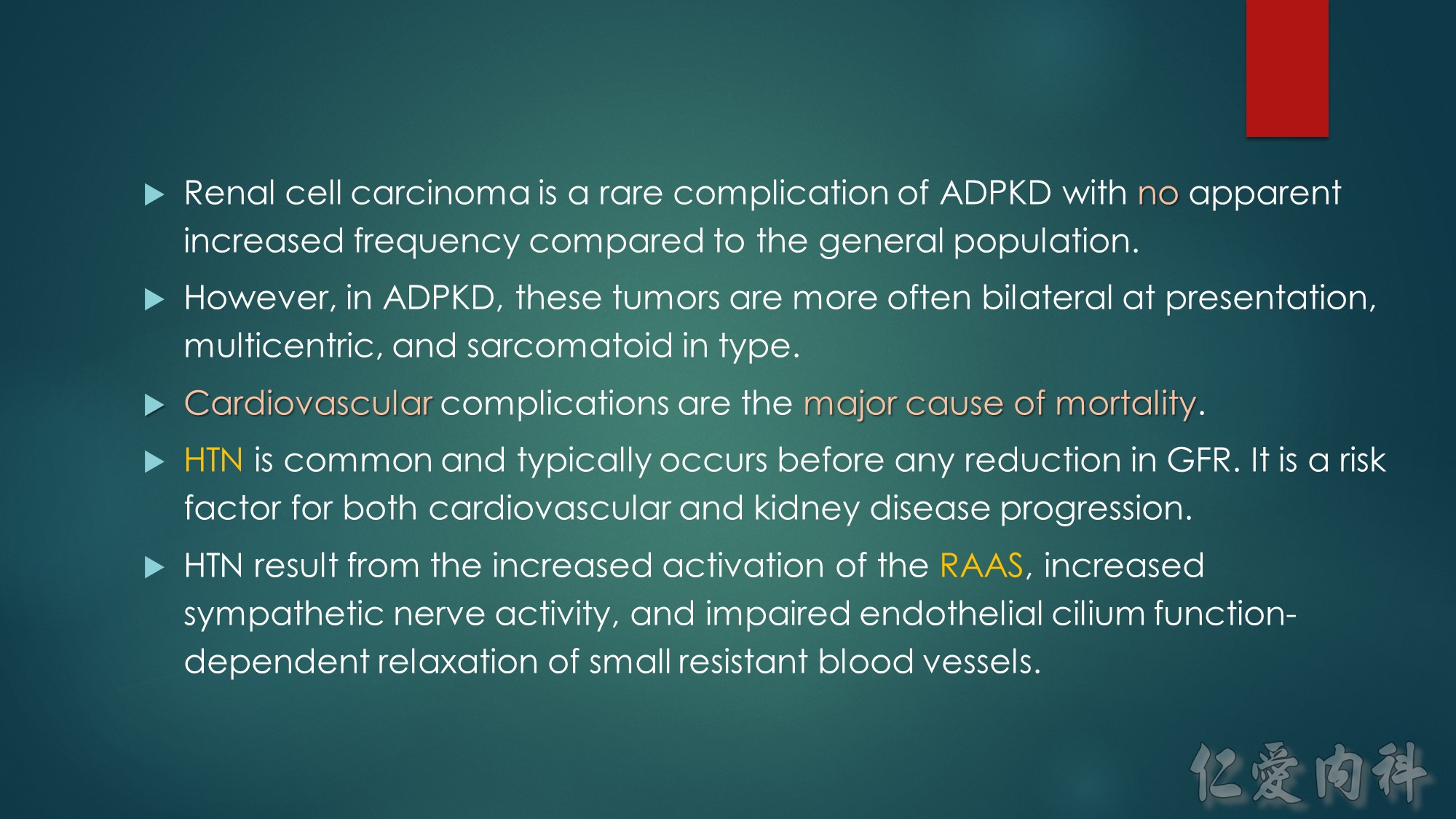
The most common cause of death before 1975 was infection (30%), followed by uremia (28%) and cardiac disease (21%); after 1975, these were cardiac disease (36%) and infection (24%).
Underlying factors for cardiac death were cardiac hypertrophy, seen in 89% of all autopsied patients, and coronary artery disease, seen in 81%.
J Am Soc Nephrol. 1995 Jun;5(12):2048-56

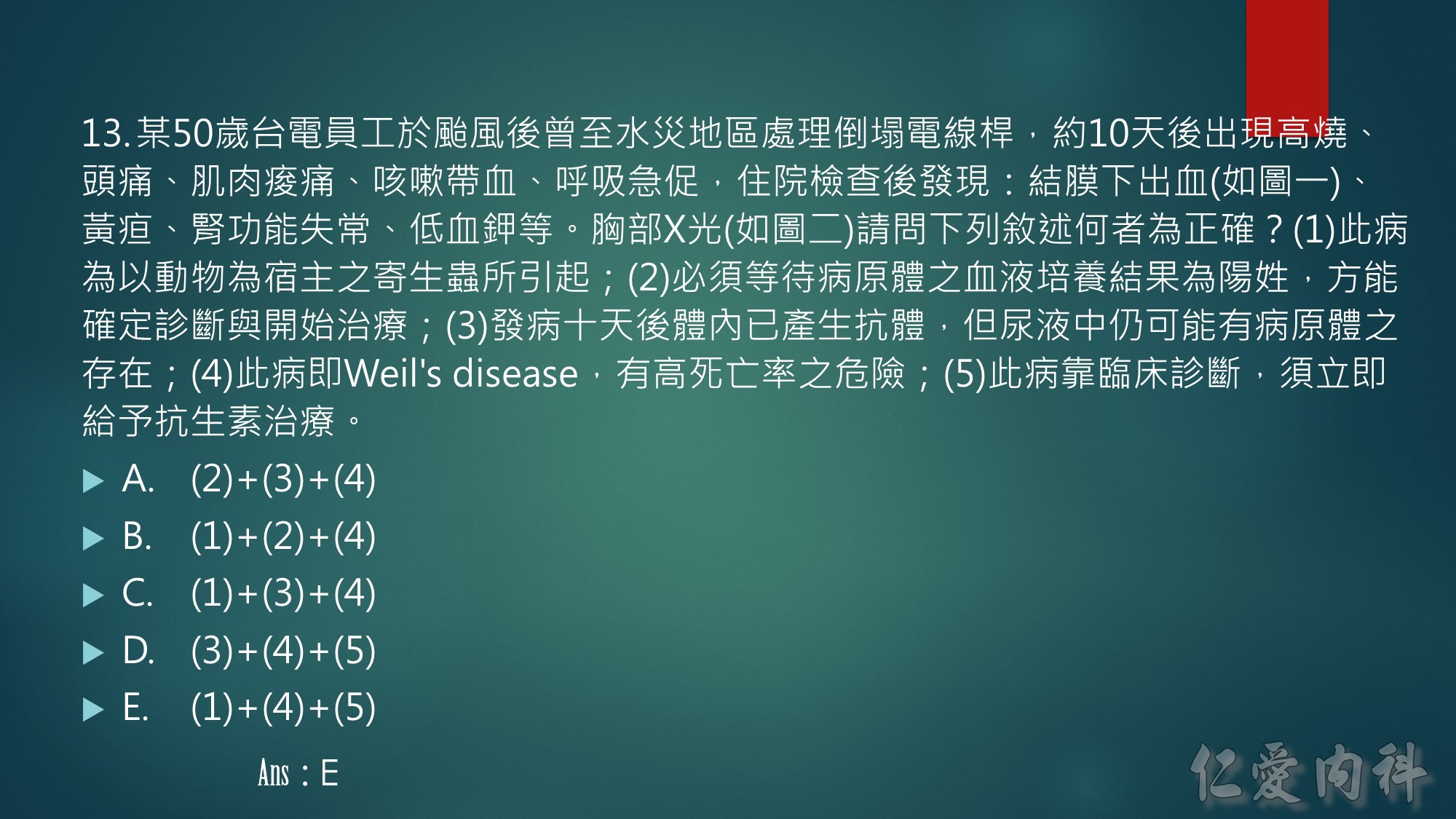 13題: 更正解答:D
13題: 更正解答:D




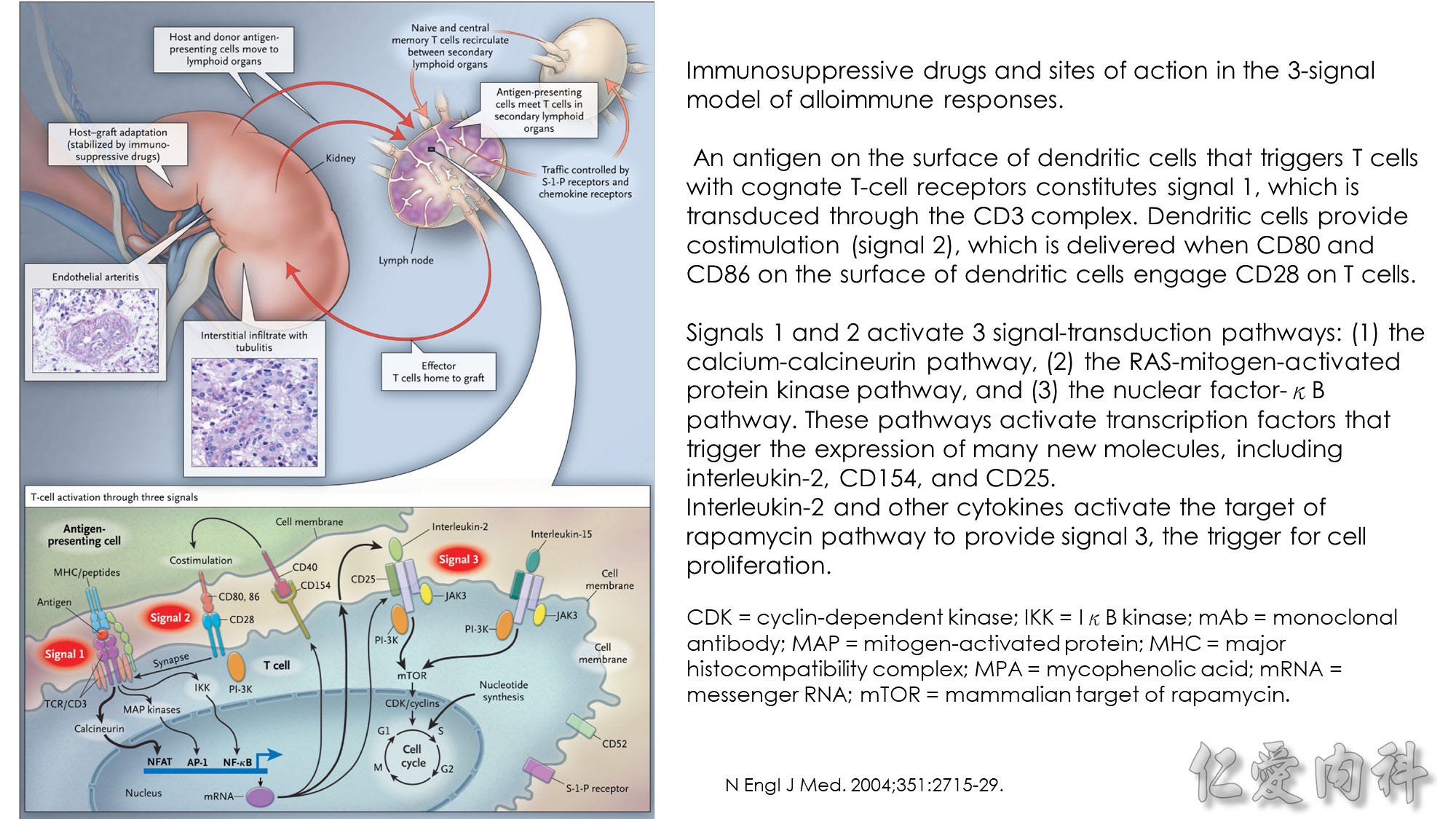
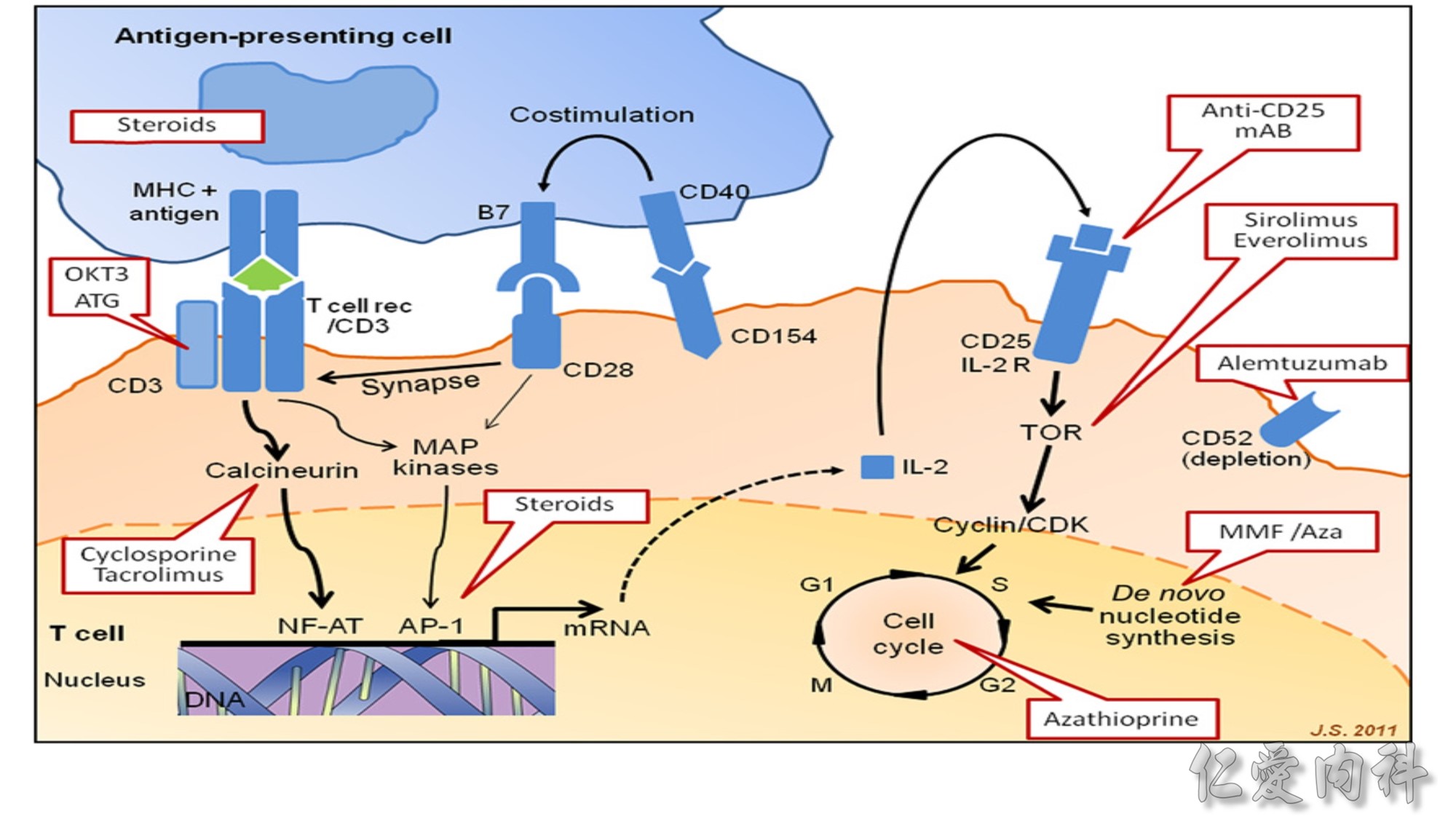
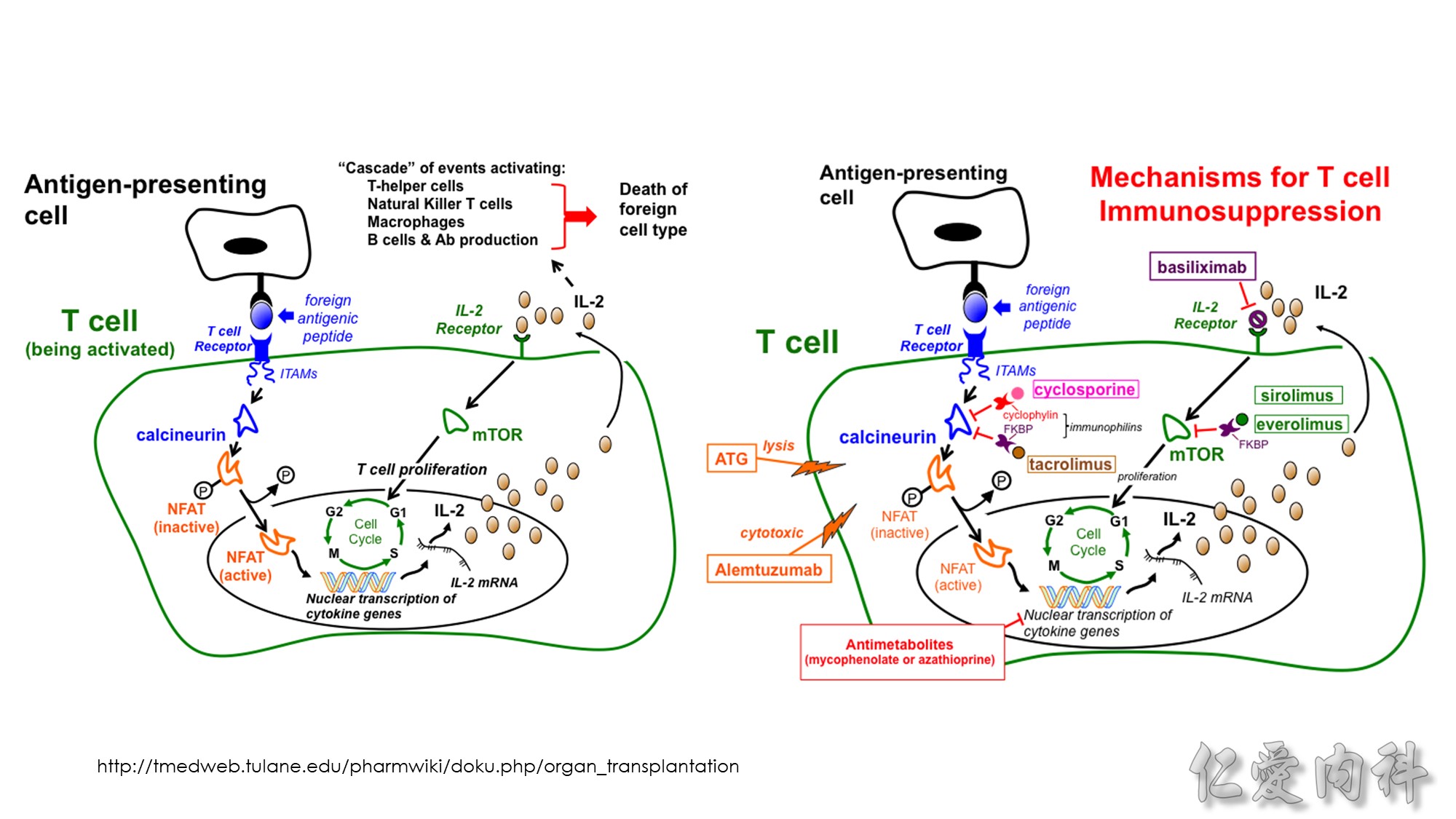
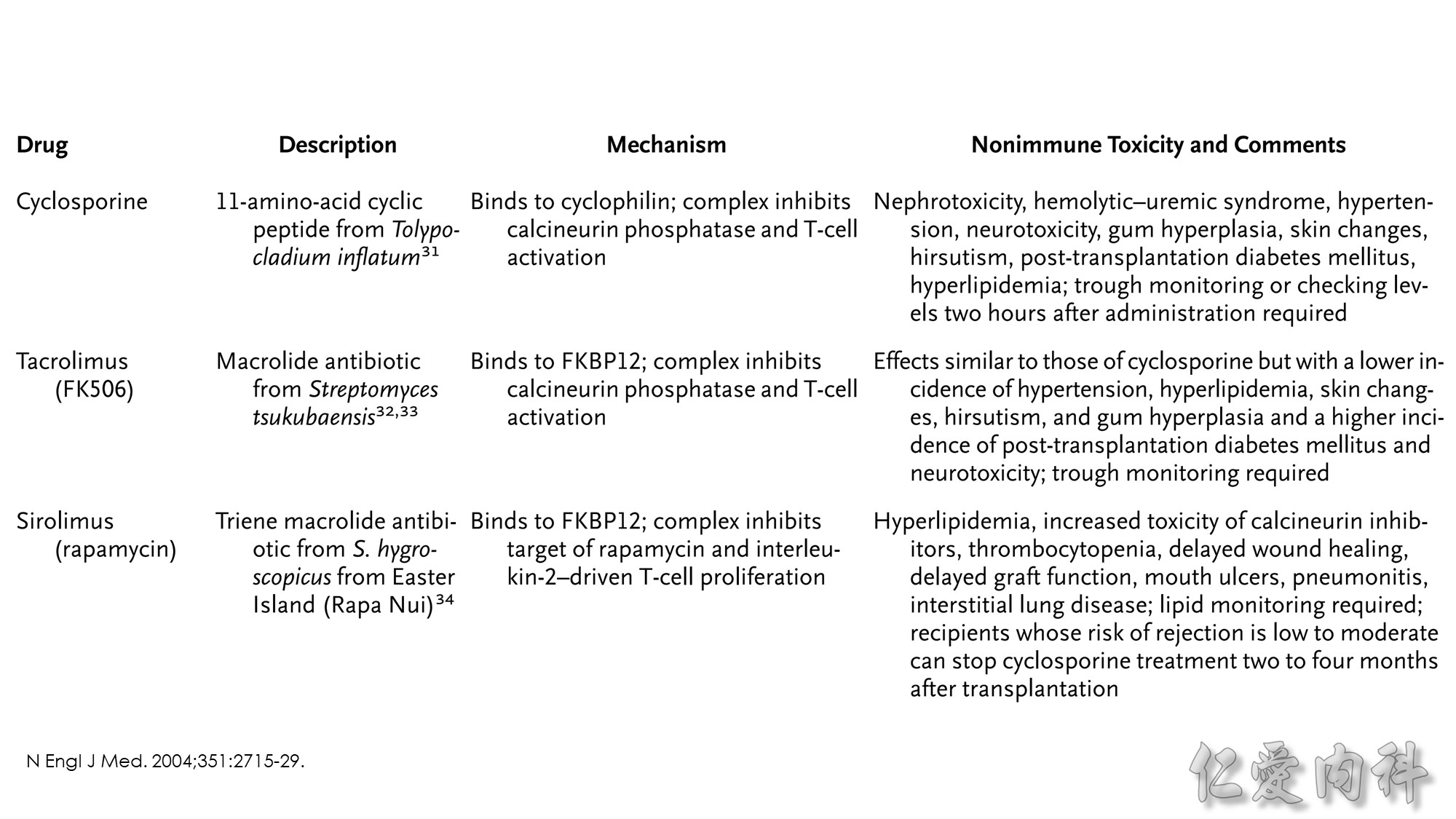
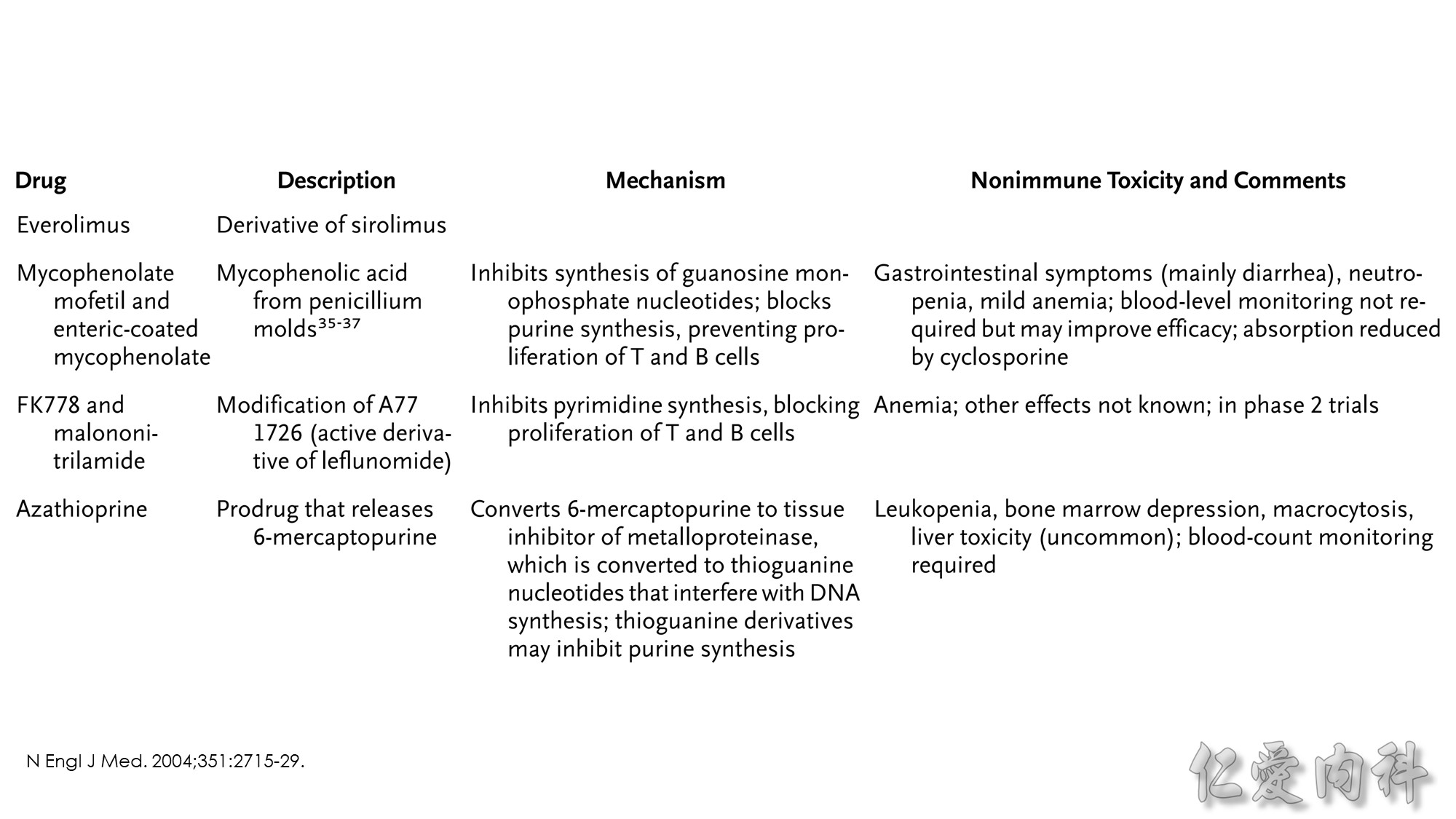
Steps in T-Cell–Mediated Rejection.
Antigen-presenting cells of host or donor origin migrate to T-cell areas of secondary lymphoid organs. These T cells ordinarily circulate between lymphoid tissues, regulated by chemokine and sphingosine-1-phosphate (S-1-P) receptors. APCs present donor antigen to naïve and central memory T cells.
Some presentation of antigen by donor cells in the graft cannot be excluded (e.g., endothelial cells that activate antigen-experienced T cells).
T cells are activated and undergo clonal expansion and differentiation to express effector functions. Antigen triggers T-cell receptors (TCRs) (signal 1) and synapse formation. CD80 (B7-1) and CD86 (B7-2) on the APC engage CD28 on the T cell to provide signal . These signals activate three signal-transduction pathways — the calcium–calcineurin pathway, the mitogen-activated protein (MAP) kinase pathway, and the protein kinase C–nuclear factorkB (NF-kB) pathway — which activate transcription factors nuclear factor of activated T cells (NFAT), activating protein 1 (AP-1), and NF-kB, respectively.
The result is expression of CD154 (which further activates APCs), interleukin-2 receptor a chain (CD25), and interleukin-2.
Receptors for a number of cytokines (interleukin-2, 4, 7, 15, and 21) share the common g chain, which binds Janus kinase 3 (JAK3).
Interleukin-2 and interleukin-15 deliver growth signals (signal 3) through the phosphoinositide-3-kinase (PI-3K) pathway and the molecular-target of-rapamycin (mTOR) pathway, which initiates the cell cycle.
Lymphocytes require synthesis of purine and pyrimidine nucleotides for replication, regulated by inosine monophosphate dehydrogenase (IMPDH) and dihydroorotate dehydrogenase (DHODH), respectively.
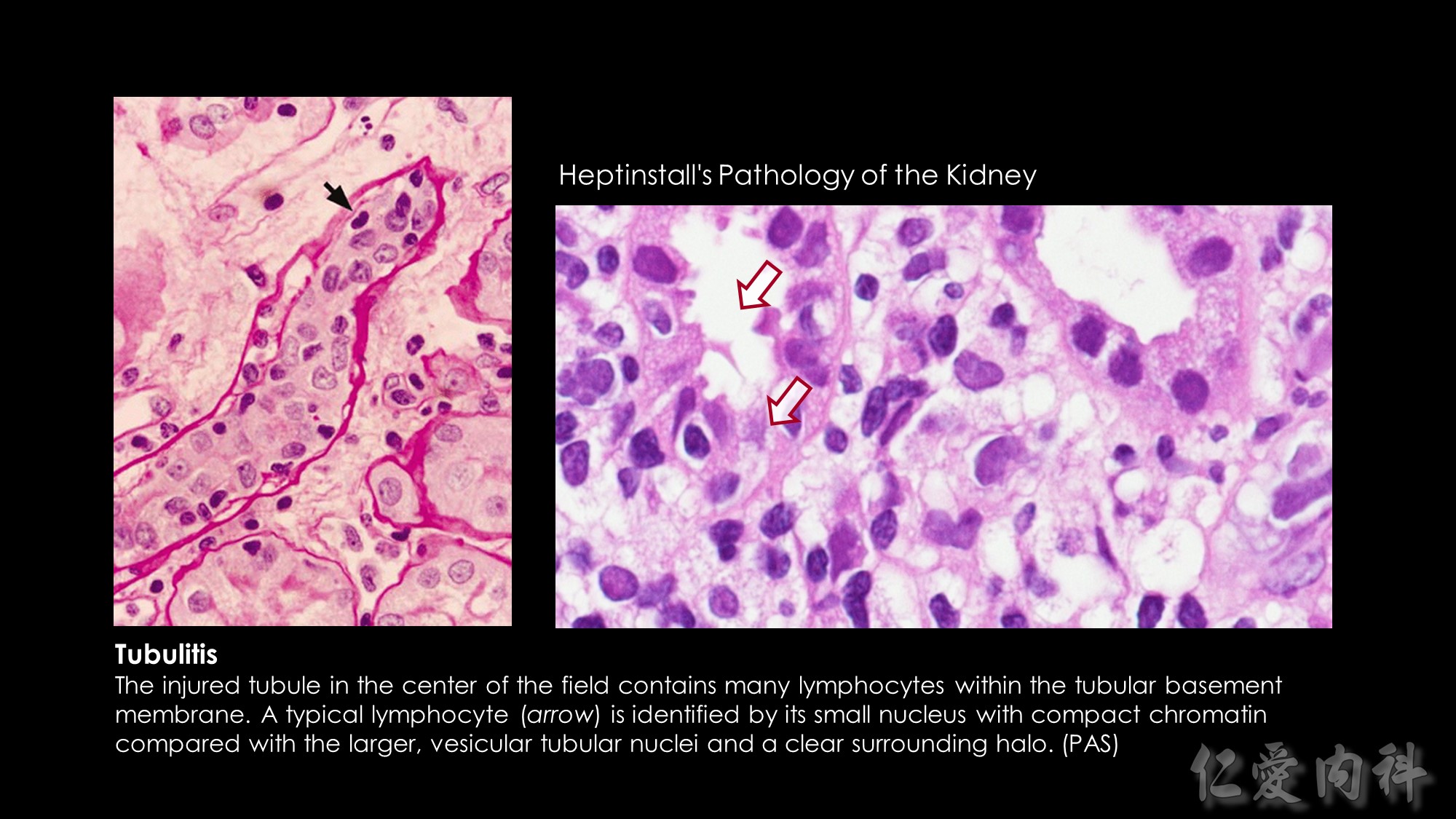
Antigen experienced T cells home to and infiltrate the graft and engage the parenchyma to create typical rejection lesions such as tubulitis and, in more advanced rejection, endothelial arteritis. However, if the rejection does not destroy the graft, adaptation occurs and is stabilized by immunosuppressive drugs.
The photomicrographs of tubulitis and endothelial arteritis are taken from a mouse model in which these lesions are T-cell–dependent but independent of perforin, granzymes, and antibody.
IKK denotes inhibitor of nuclear factor-kB kinase , CDK cyclin-dependent kinase, and MHC major histocompatibility complex
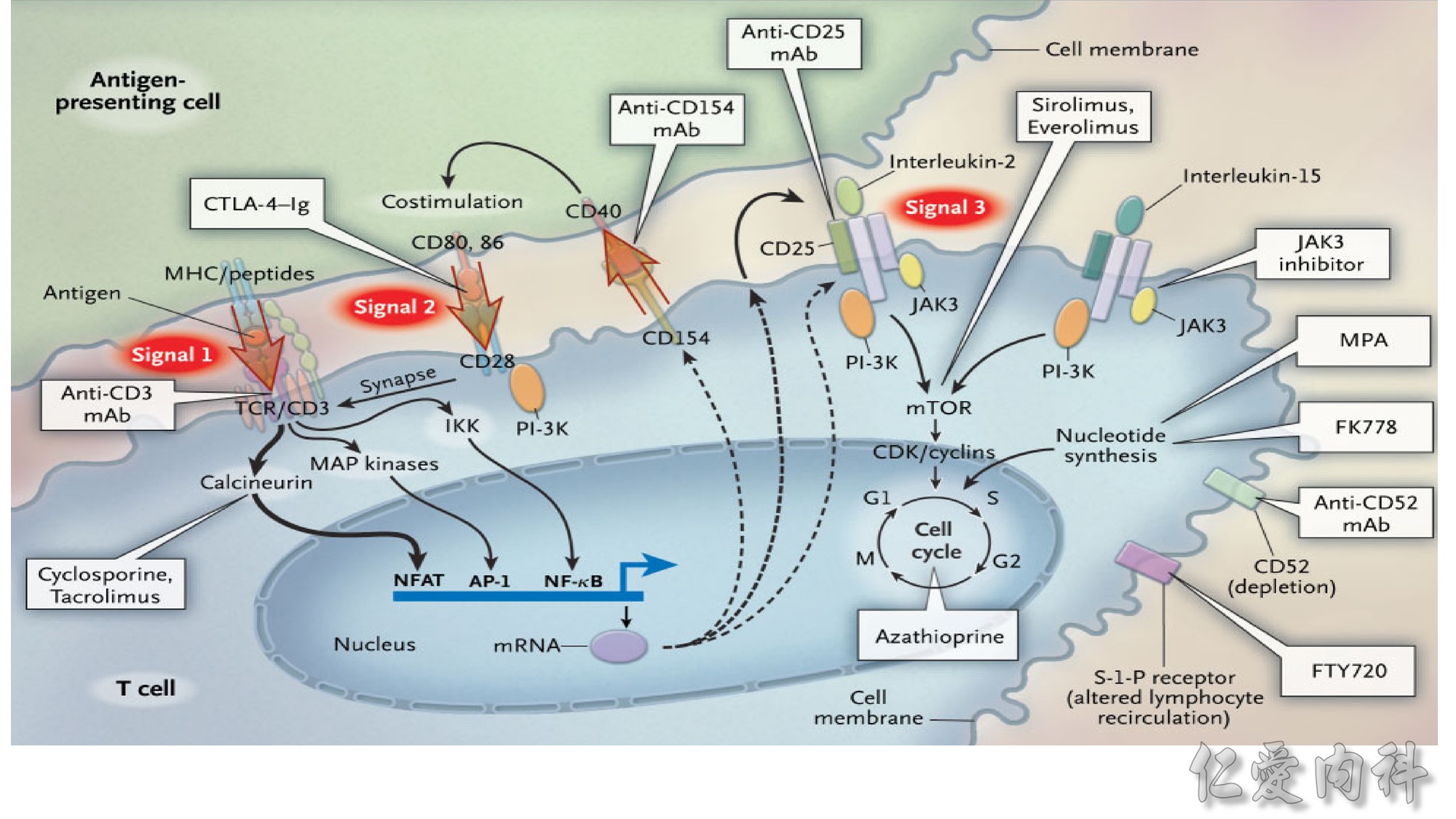
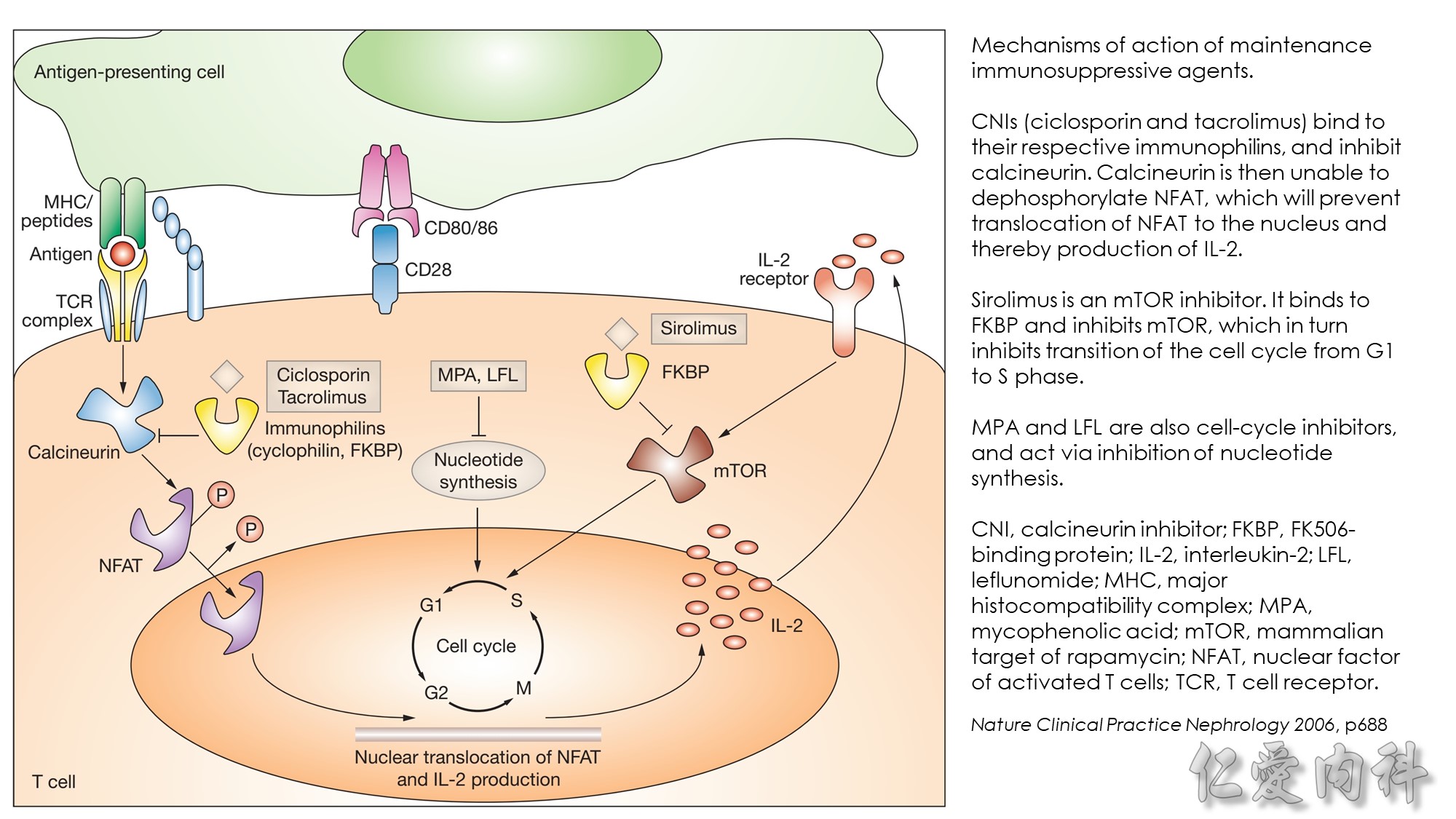
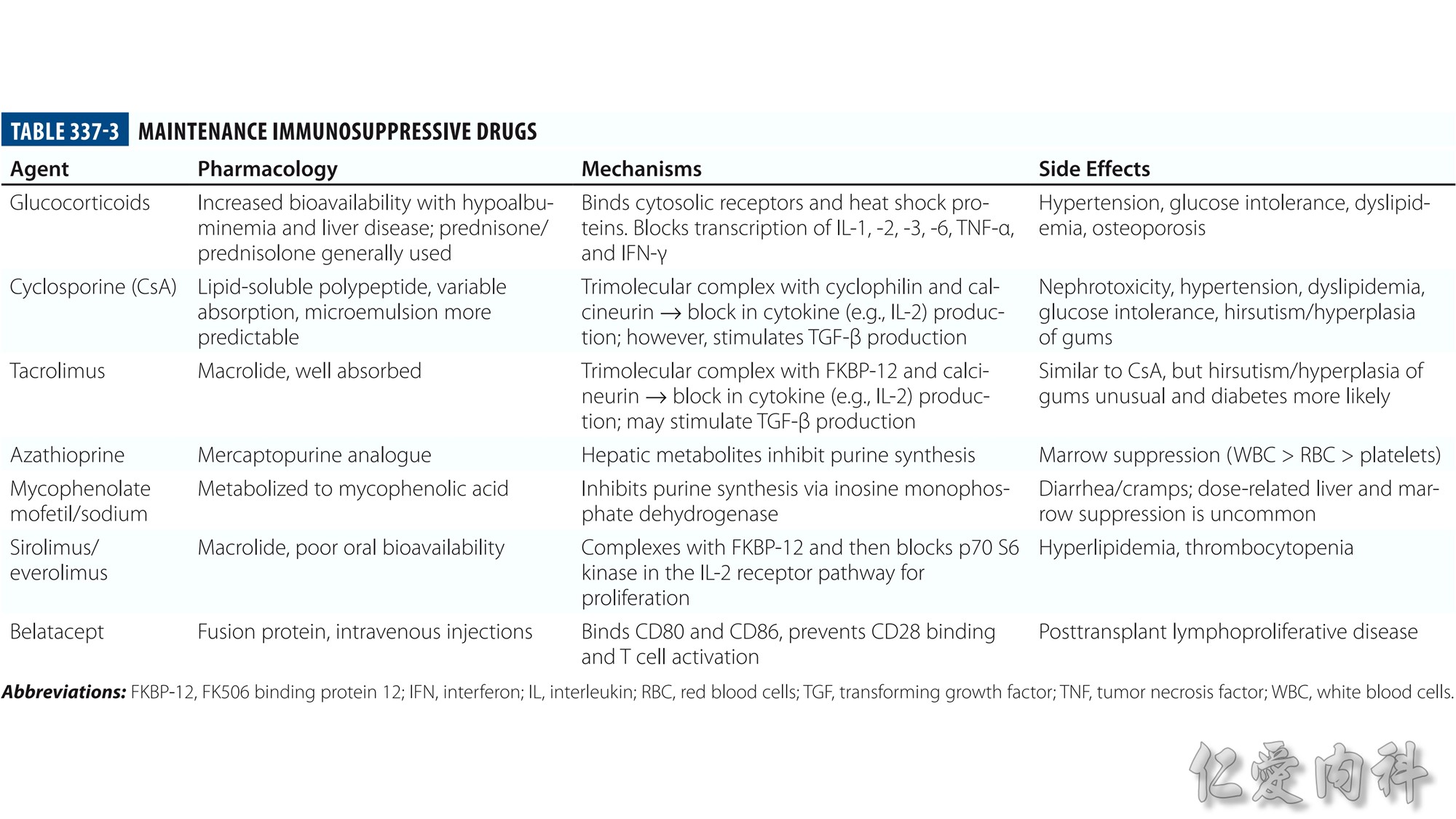
Immunosuppressive drugs and sites of action in the 3-signal model of alloimmune responses.
An antigen on the surface of dendritic cells that triggers T cells with cognate T-cell receptors constitutes signal 1, which is transduced through the CD3 complex. Dendritic cells provide costimulation (signal 2), which is delivered when CD80 and CD86 on the surface of dendritic cells engage CD28 on T cells.
Signals 1 and 2 activate 3 signal-transduction pathways: (1) the calcium-calcineurin pathway, (2) the RAS-mitogen-activated protein kinase pathway, and (3) the nuclear factor-κB pathway. These pathways activate transcription factors that trigger the expression of many new molecules, including interleukin-2, CD154, and CD25.
Interleukin-2 and other cytokines activate the target of rapamycin pathway to provide signal 3, the trigger for cell proliferation. CDK = cyclin-dependent kinase; IKK = IκB kinase; mAb = monoclonal antibody; MAP = mitogen-activated protein; MHC = major histocompatibility complex; MPA = mycophenolic acid; mRNA = messenger RNA; mTOR = mammalian target of rapamycin.