








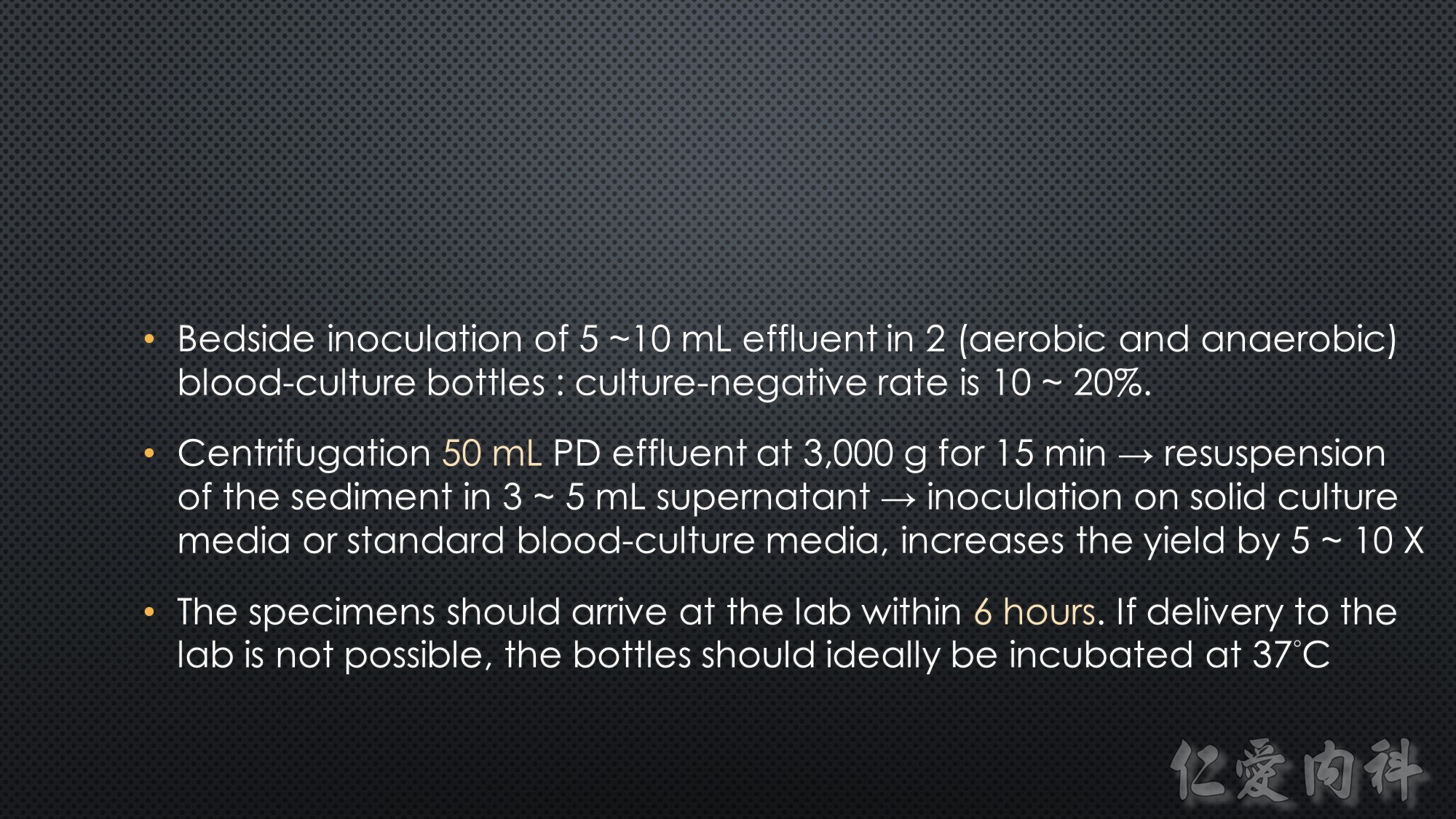



















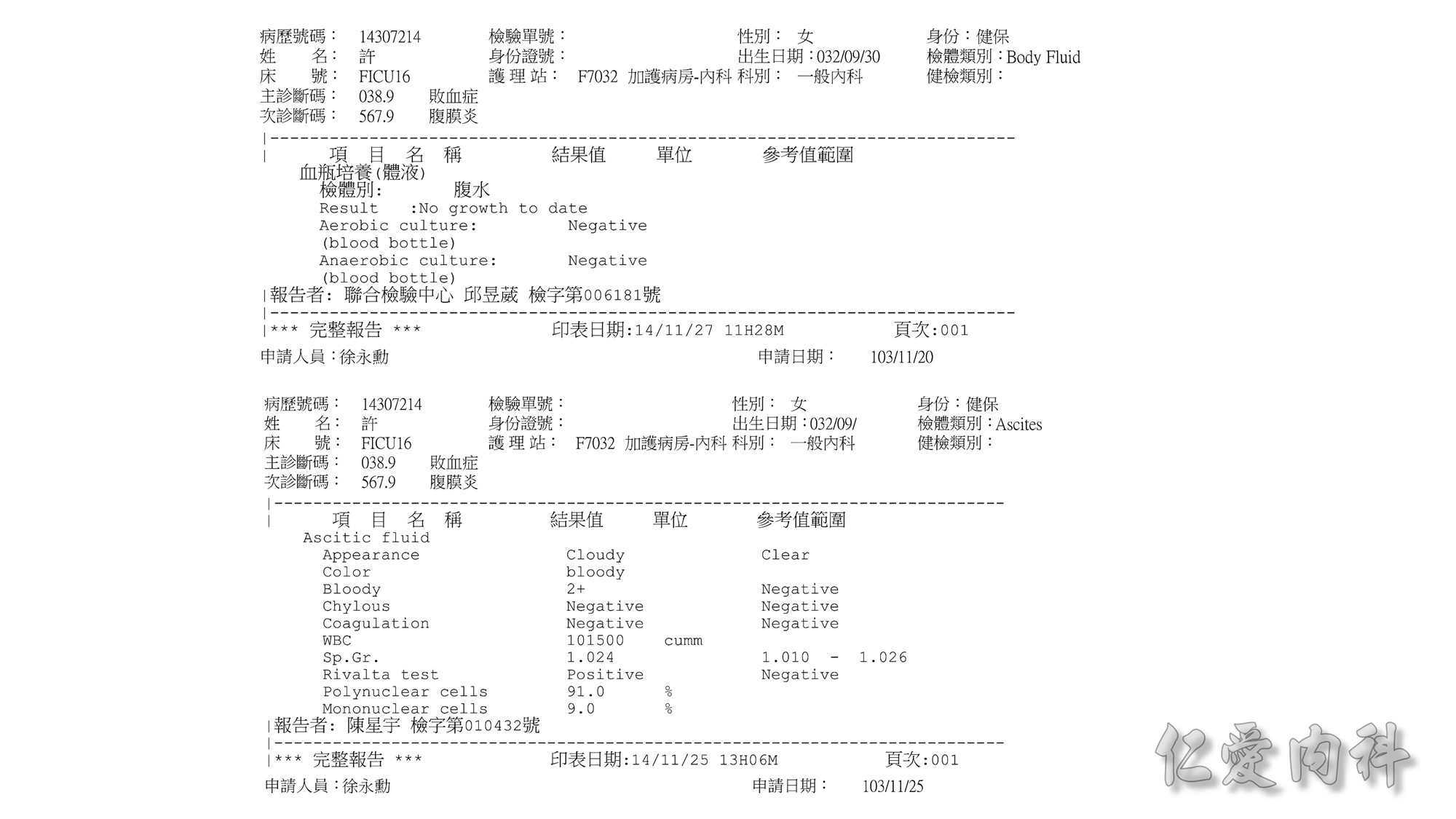
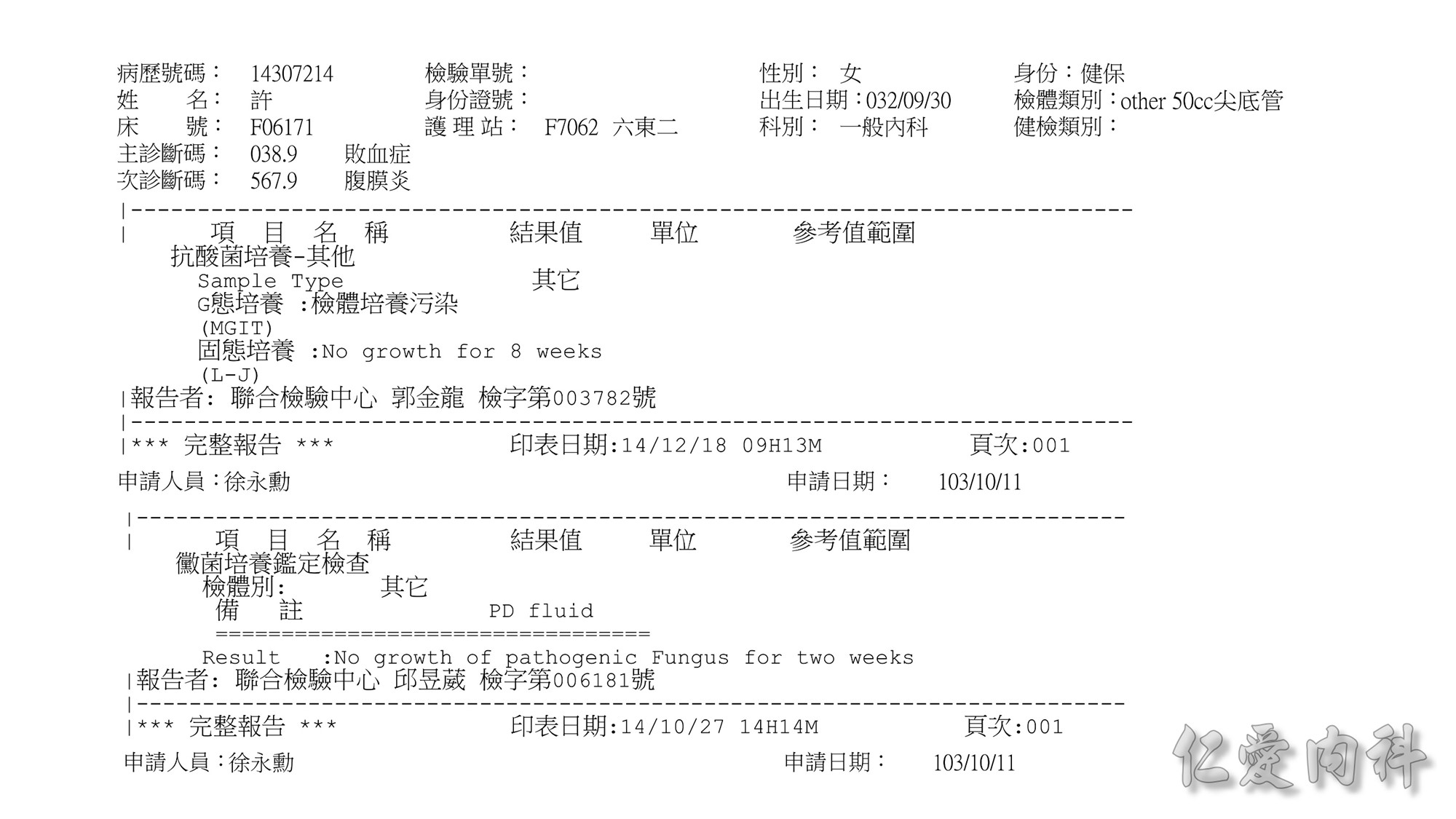
An optimal culture technique is the
combination of sediment culturing of 50 mL effluent and
bedside inoculation of 5 – 10 mL effluent in two bloodculture
bottles. The specimens should arrive within
6 hours at the laboratory. If immediate delivery to the
laboratory is not possible, the inoculated culture bottles
should ideally be incubated at 37°C. When the causative
micro-organism has been established, subsequent
cultures for monitoring may be performed by only inoculating
the effluent in blood-culture bottles. Centrifugation
of 50 mL peritoneal effluent at 3000g for 15 minutes,
followed by re suspension of the sediment in 3 – 5 mL of
sterile saline, and inoculation of this material both on
solid culture media and into a standard blood-culture
medium, is a sensitive method to identify the causative
organisms. With this method, less than 5% will be culture
negative.
















VGH + TMUH
Peritoneal Dialysis International,Vol. 28, pp. 340–342
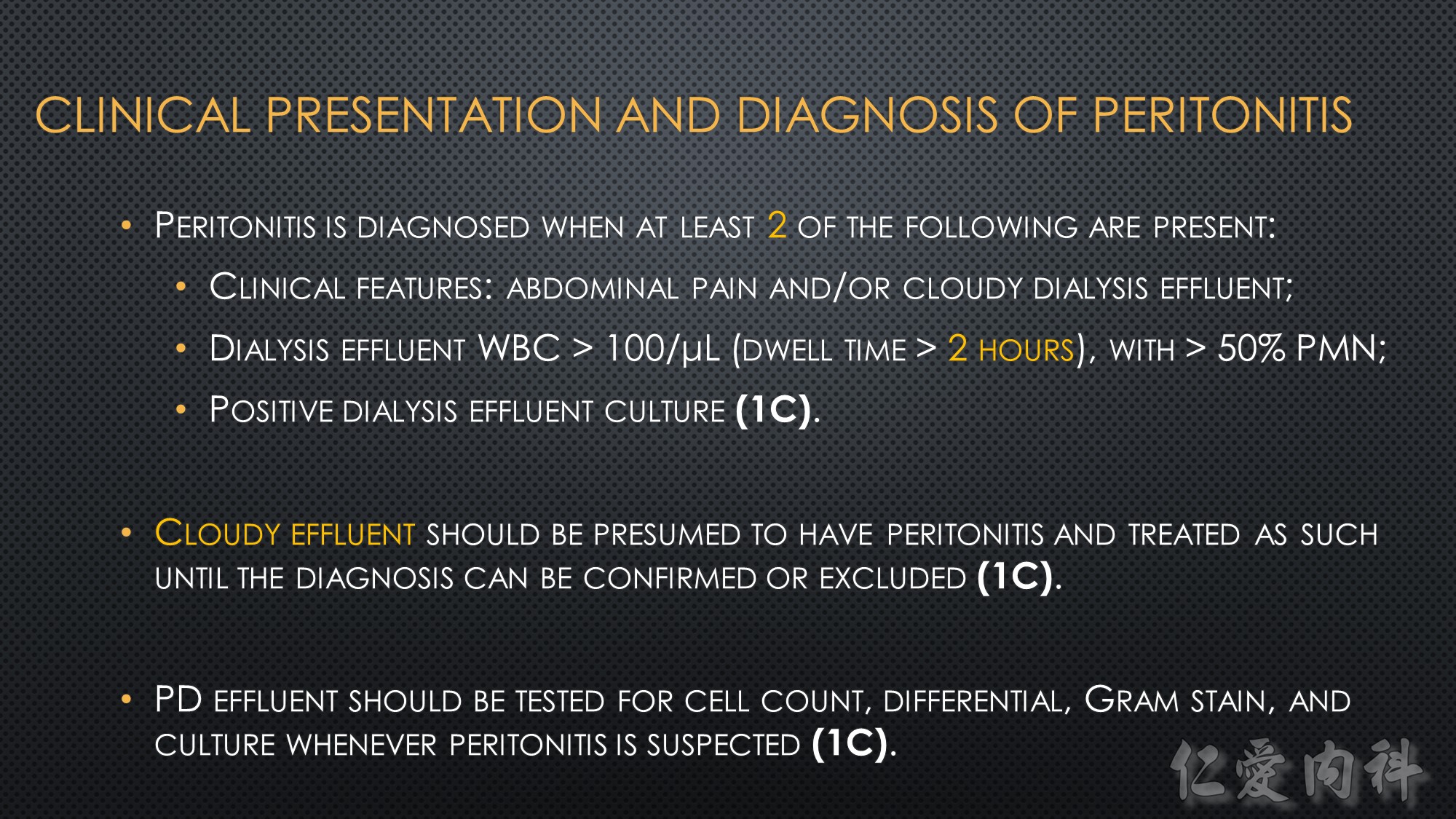
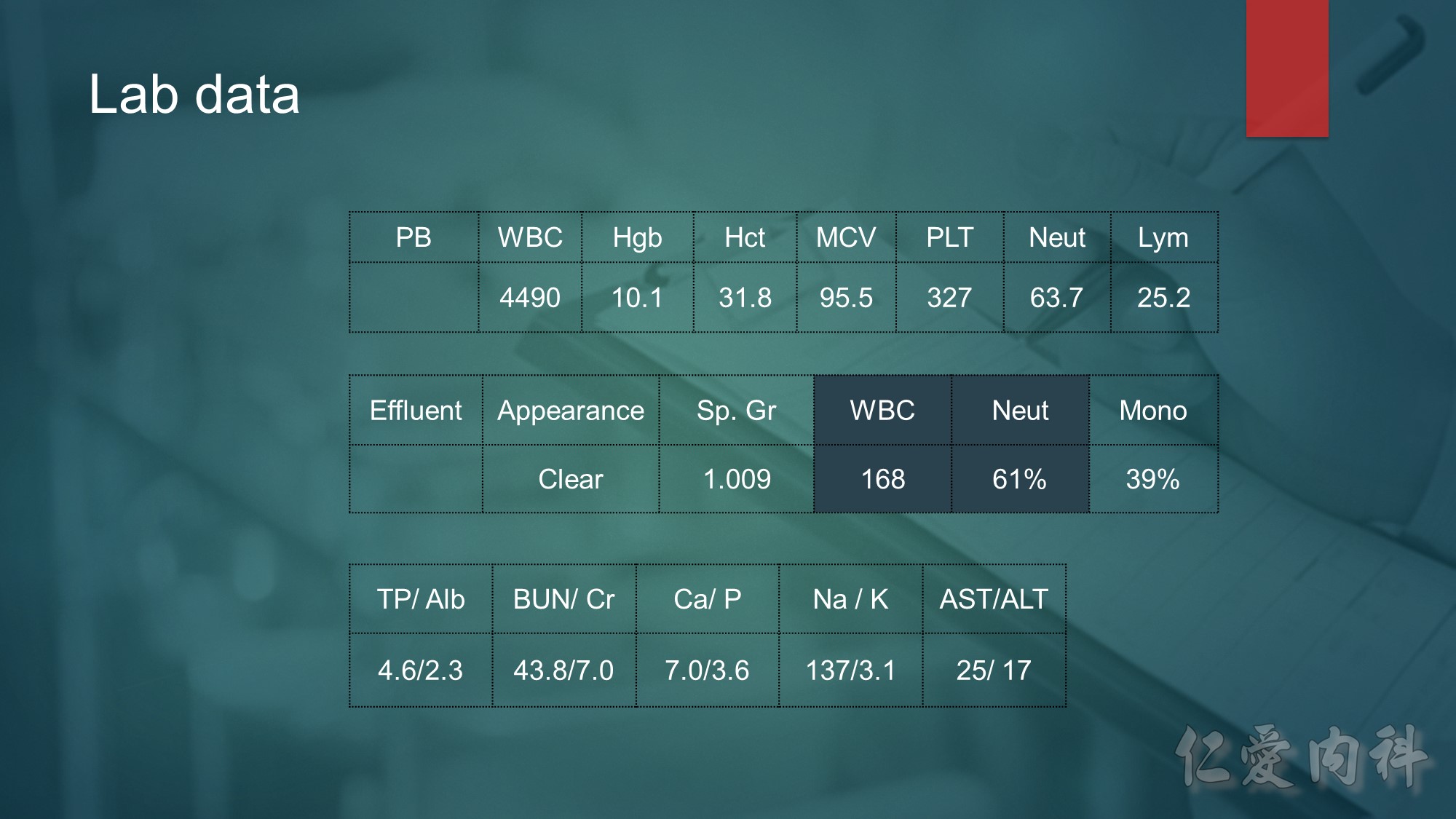
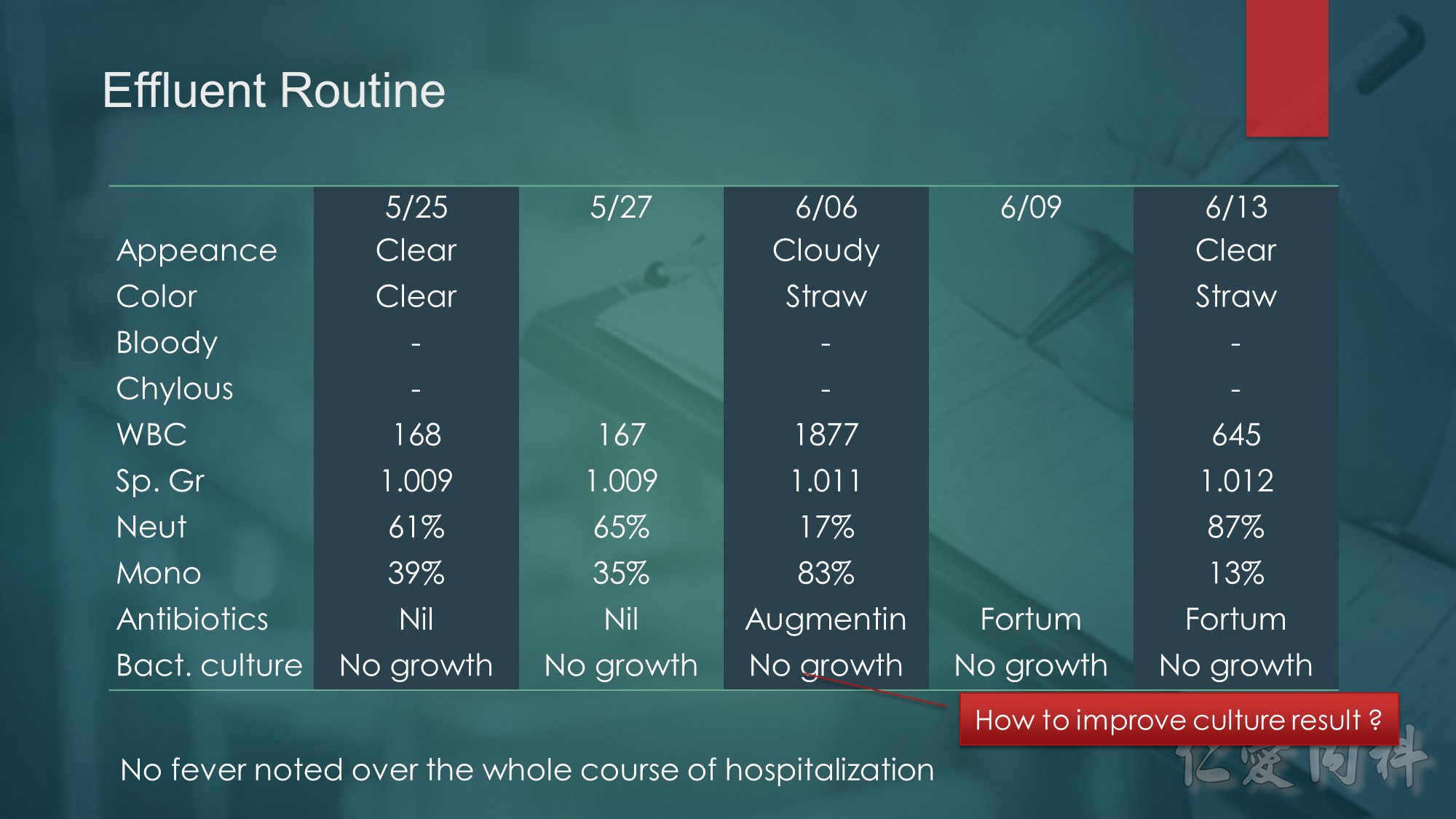
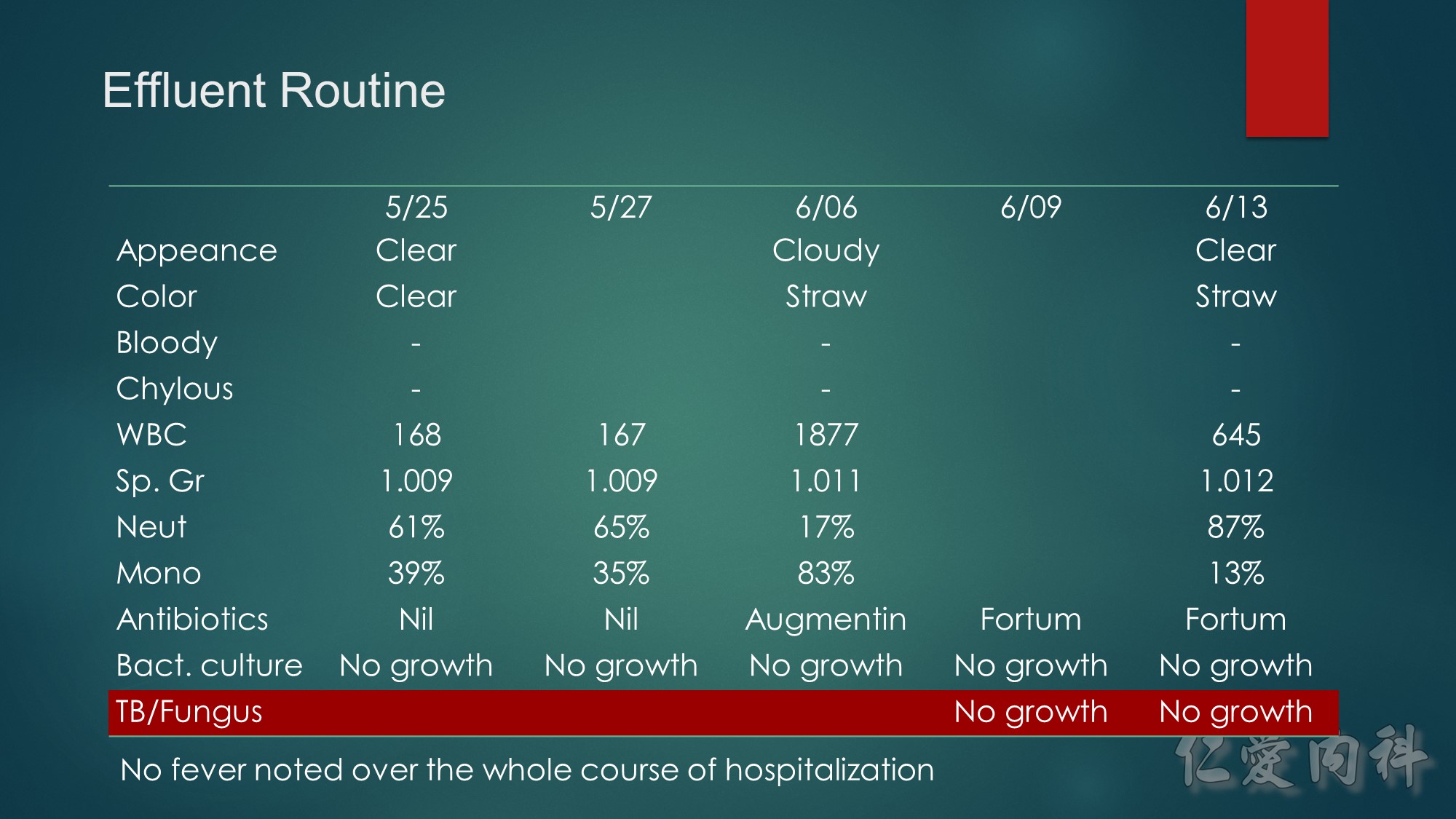
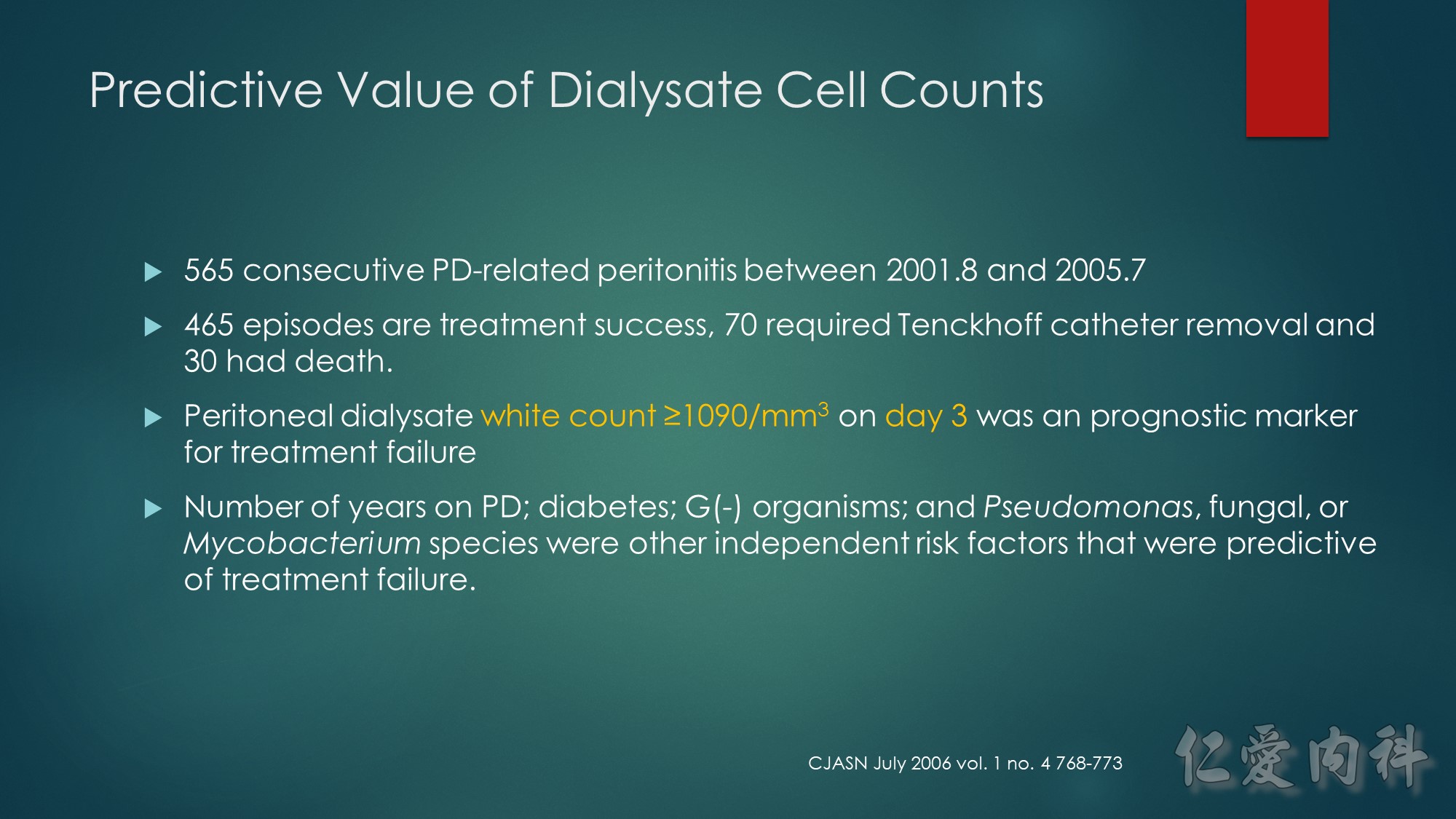
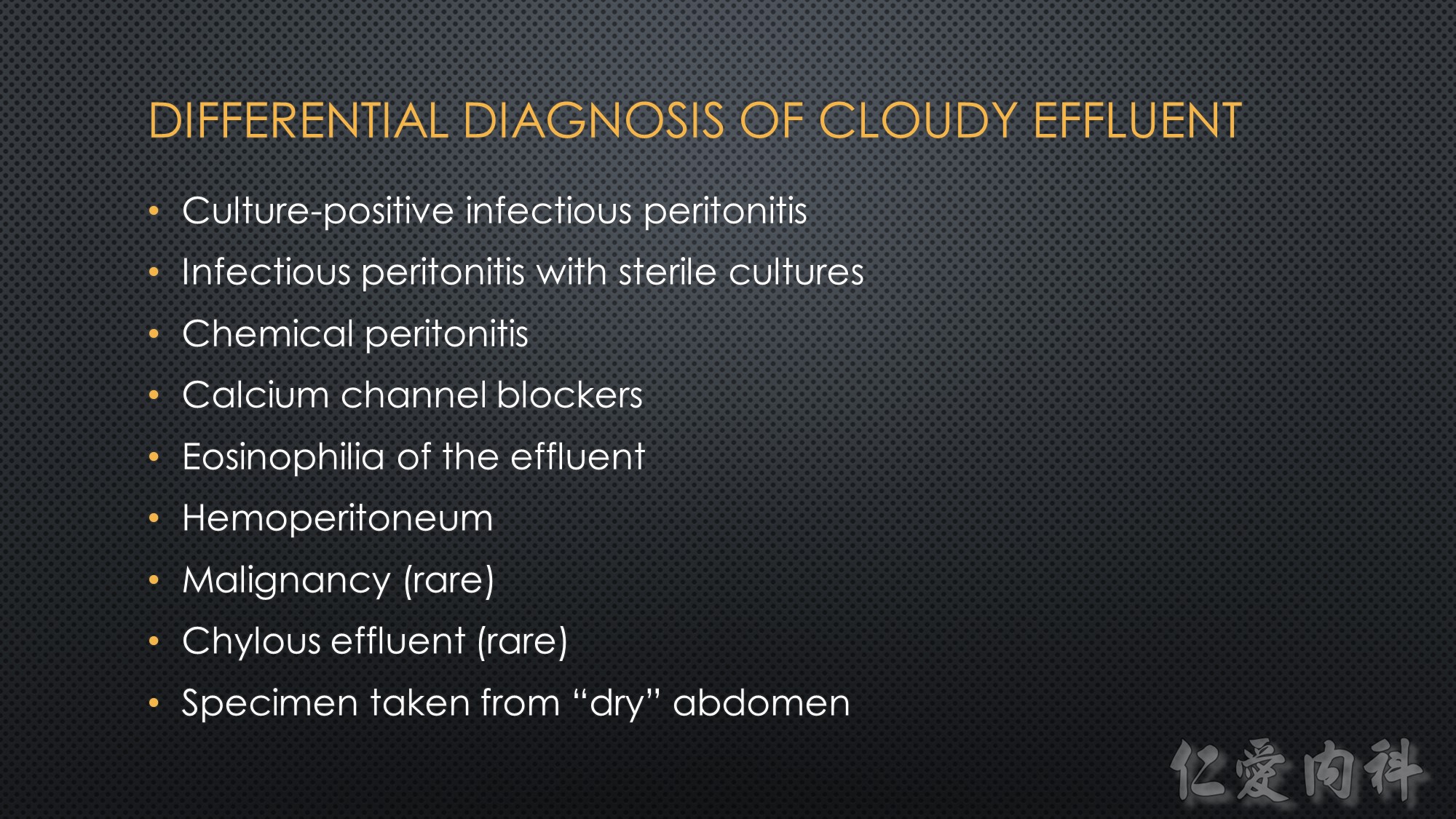
Why is the initial cell count of little
value? It is not much of a stretch to imagine why the ini-tial dialysate cell count might not predict peritonitis
outcome. One of the key issues relates to the timing of
initial dialysate effluent collection, which might not be
standardized enough upon first presentation of cloudy
effluent. The initial white cell counts, by definition, are
derived from samples collected at the time of presenta-tion to the dialysis unit, and the number of cells in the
peritoneal effluent also depends in part on the length
of the dwell (14). Such inherent propensity to random
measurement error for the initial white cell count can
thus lead to “noise” that gets in the way of our deriva-tion of prognostic information.

Trimethoprim/sulfamethoxazole is preferred for Stenotrophomonas species.



11/03 cefepime 12/19 tazocin 12/31 mepem
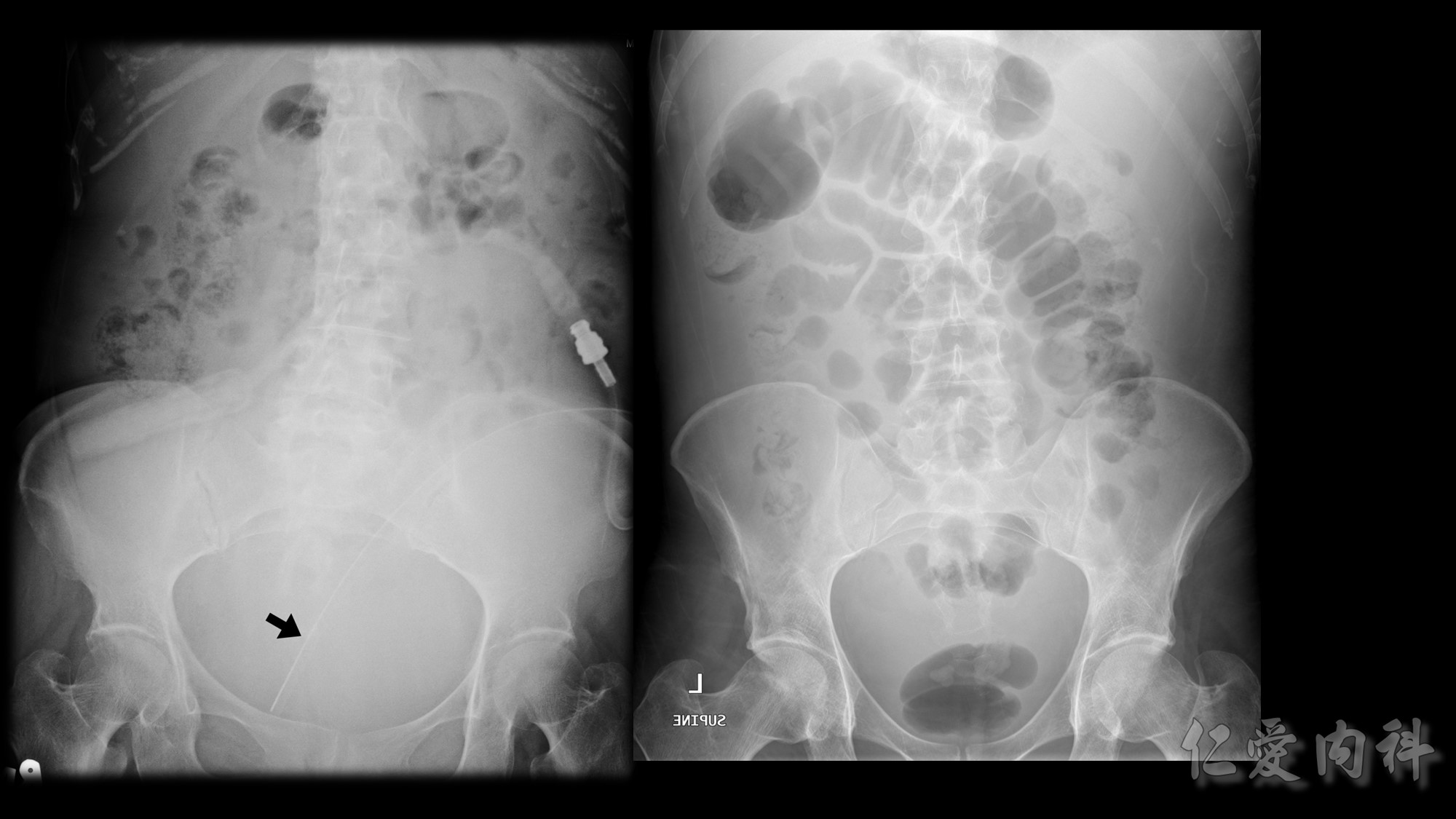
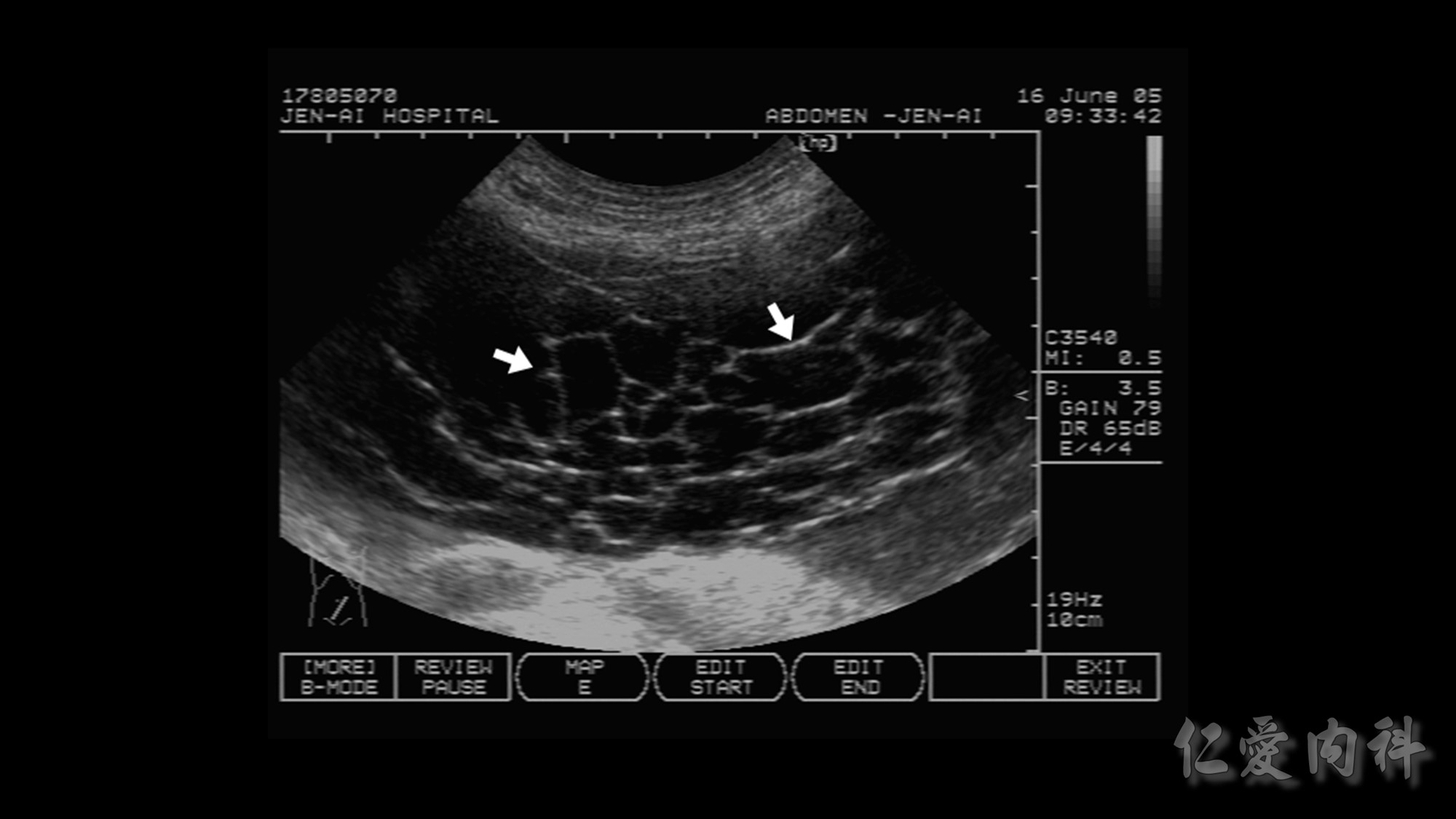
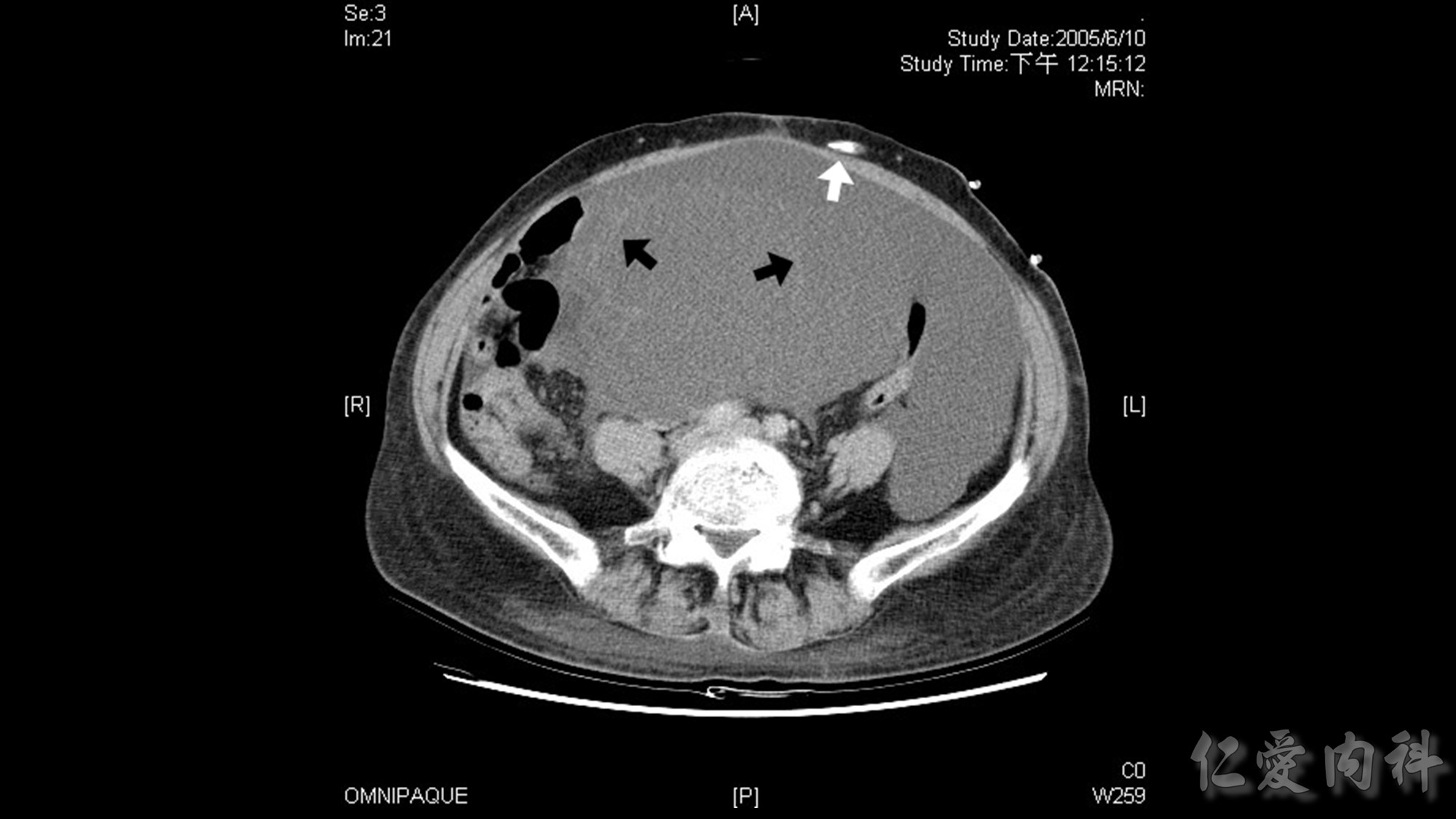
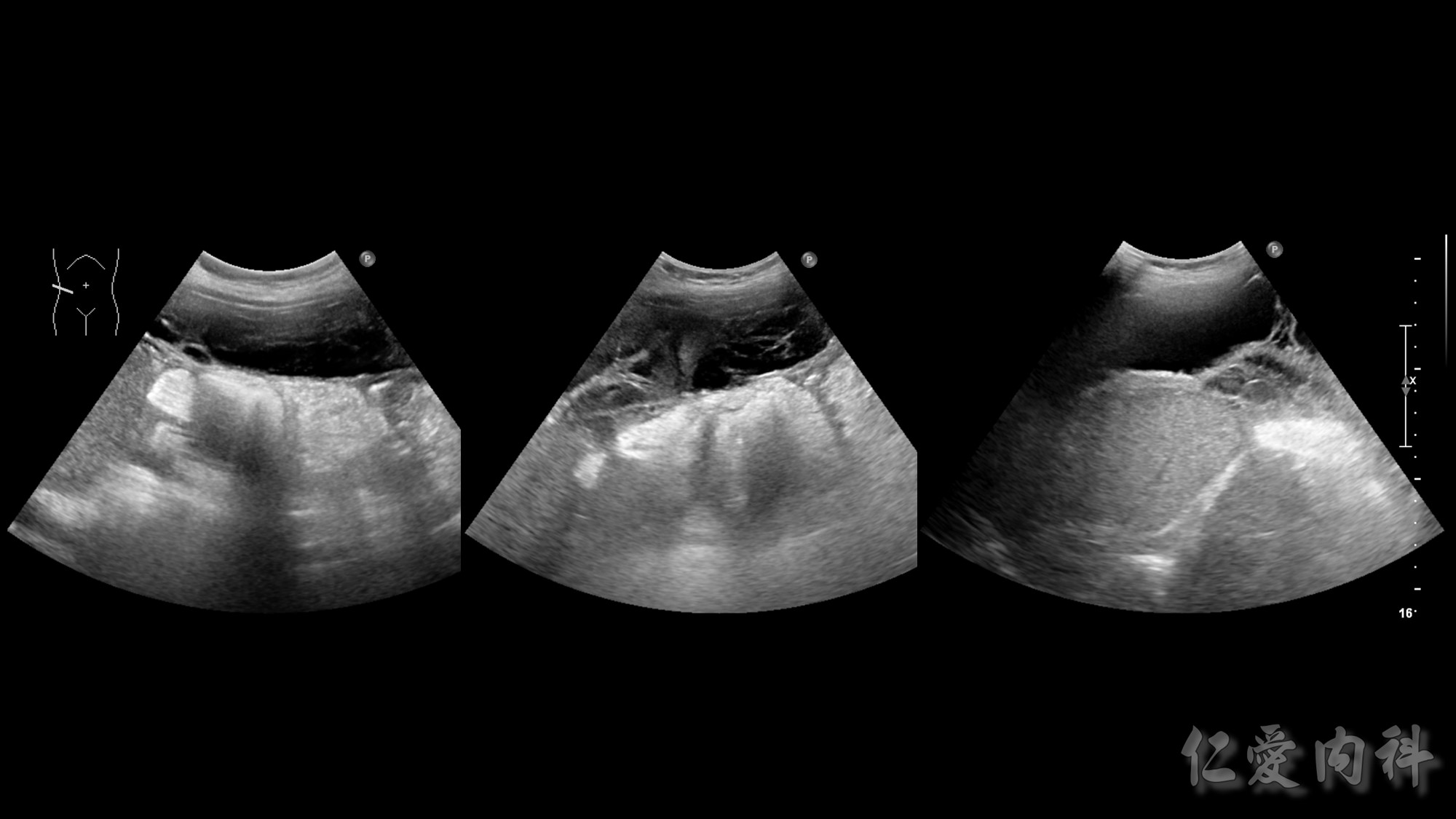
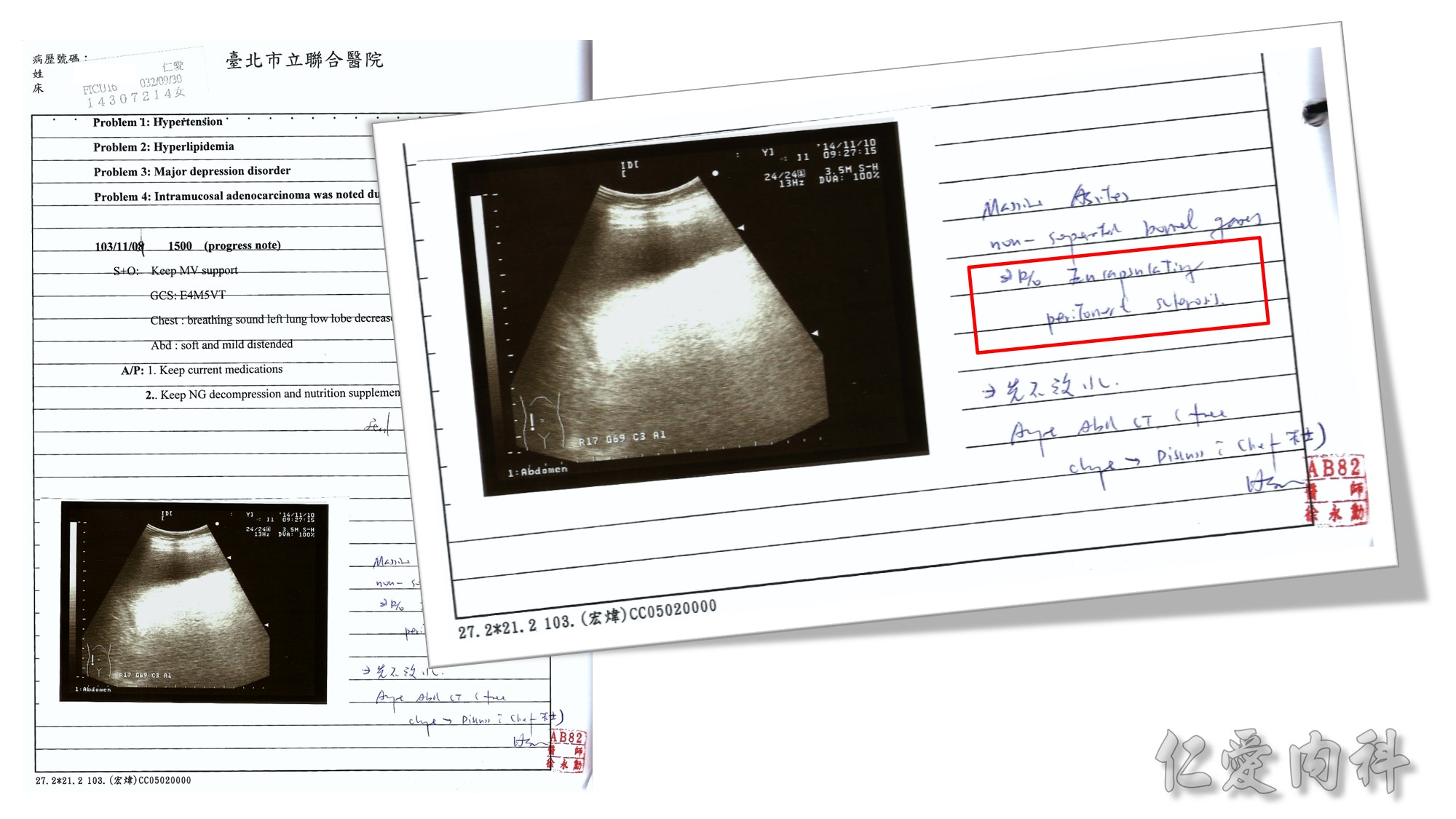
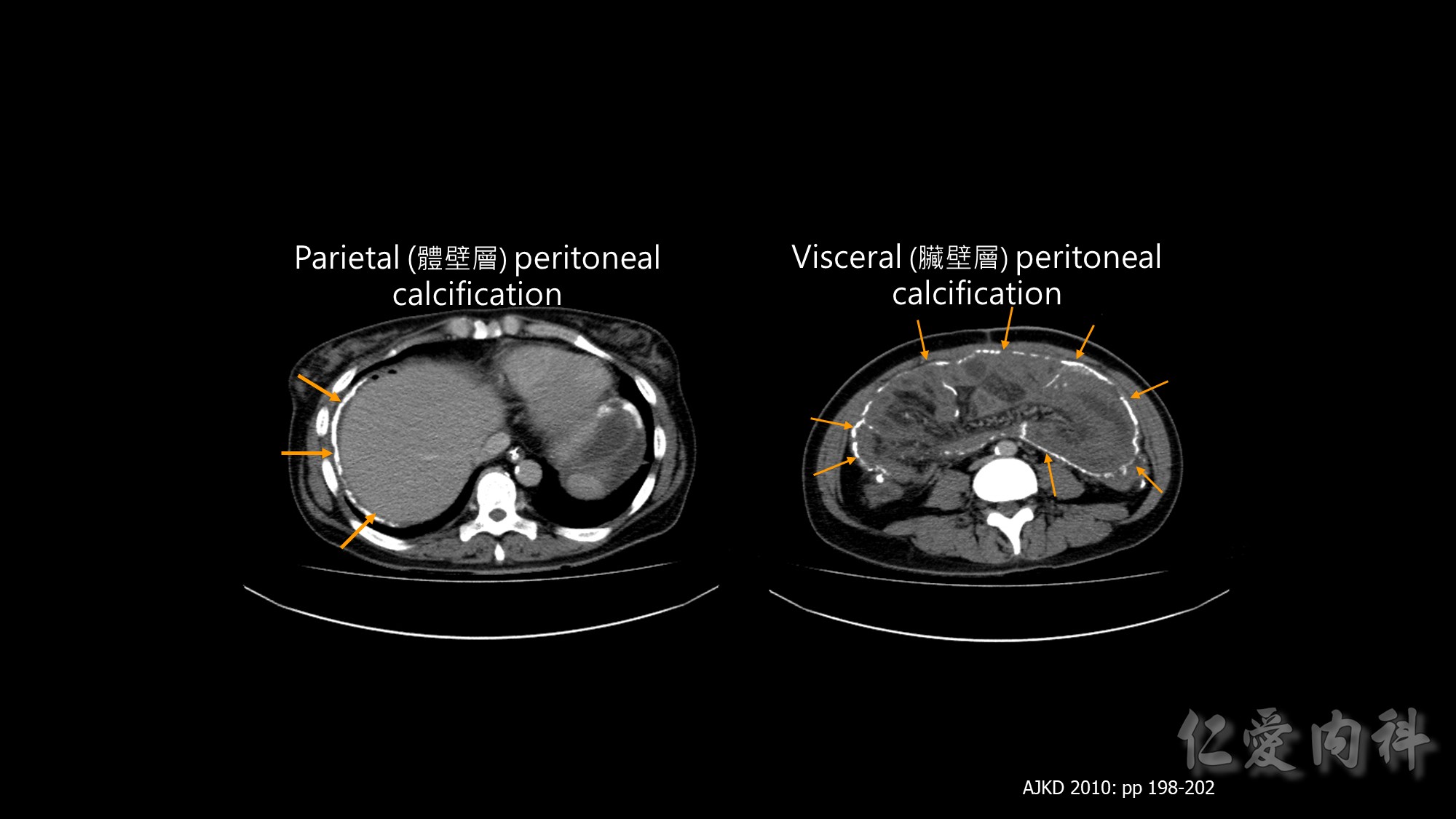
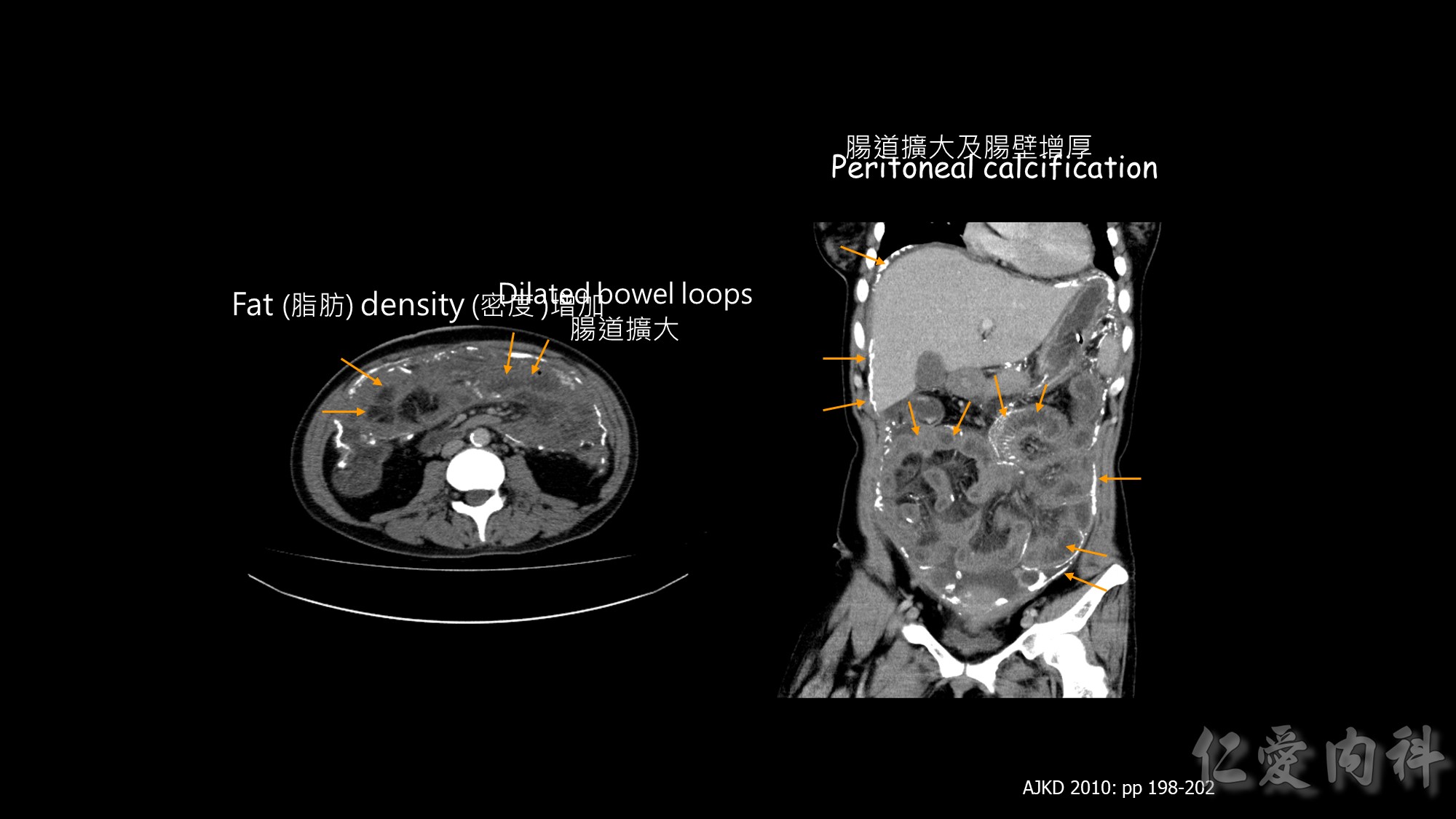
Loculated ascites and peritoneal thickening with diffusely minimally increased
tracer activity; sclerosing encapsulating peritonitis cannot be excluded. Note: The
gallium uptake could be suppressed under the treatment of systemic antibiotics.
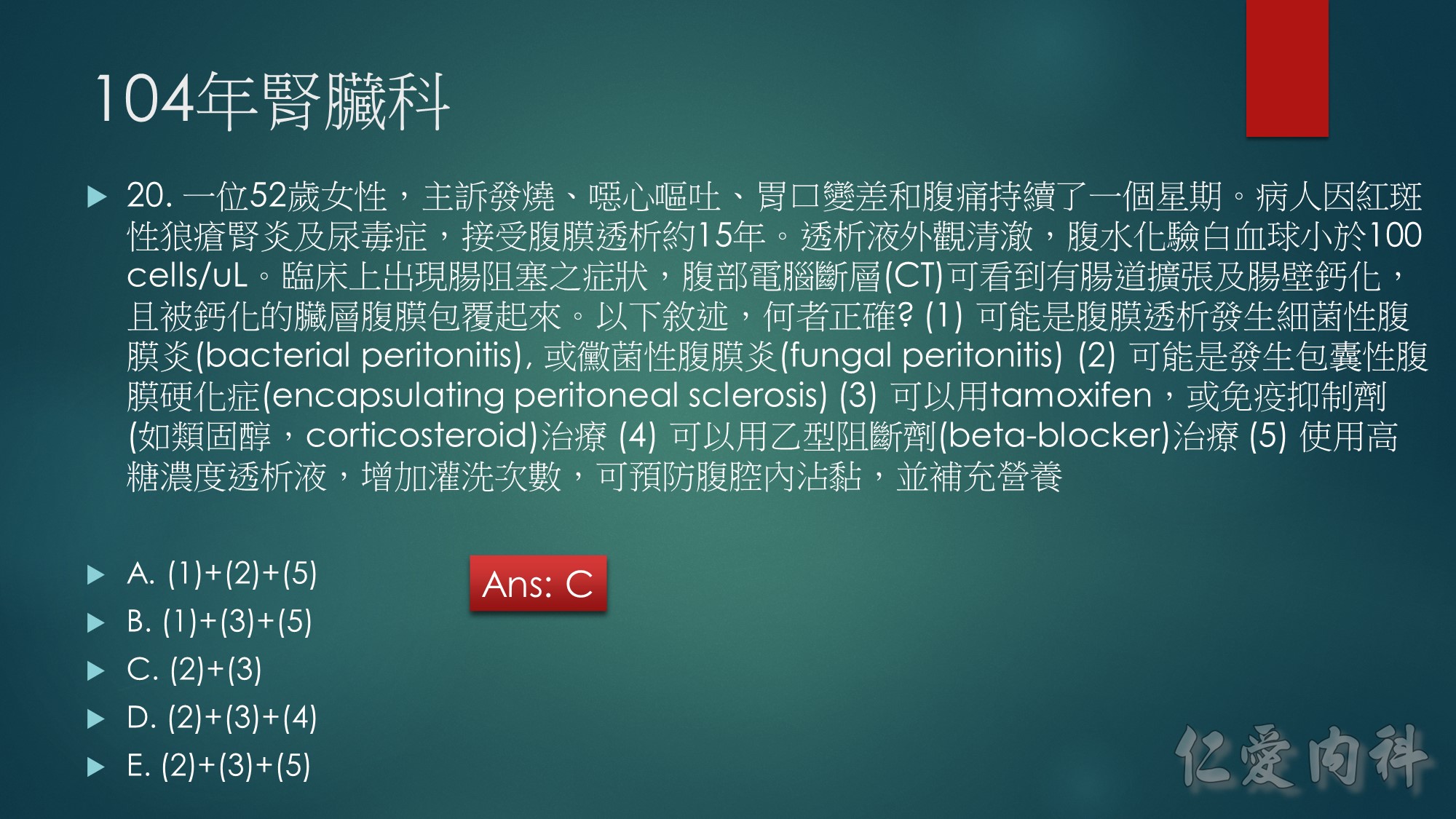
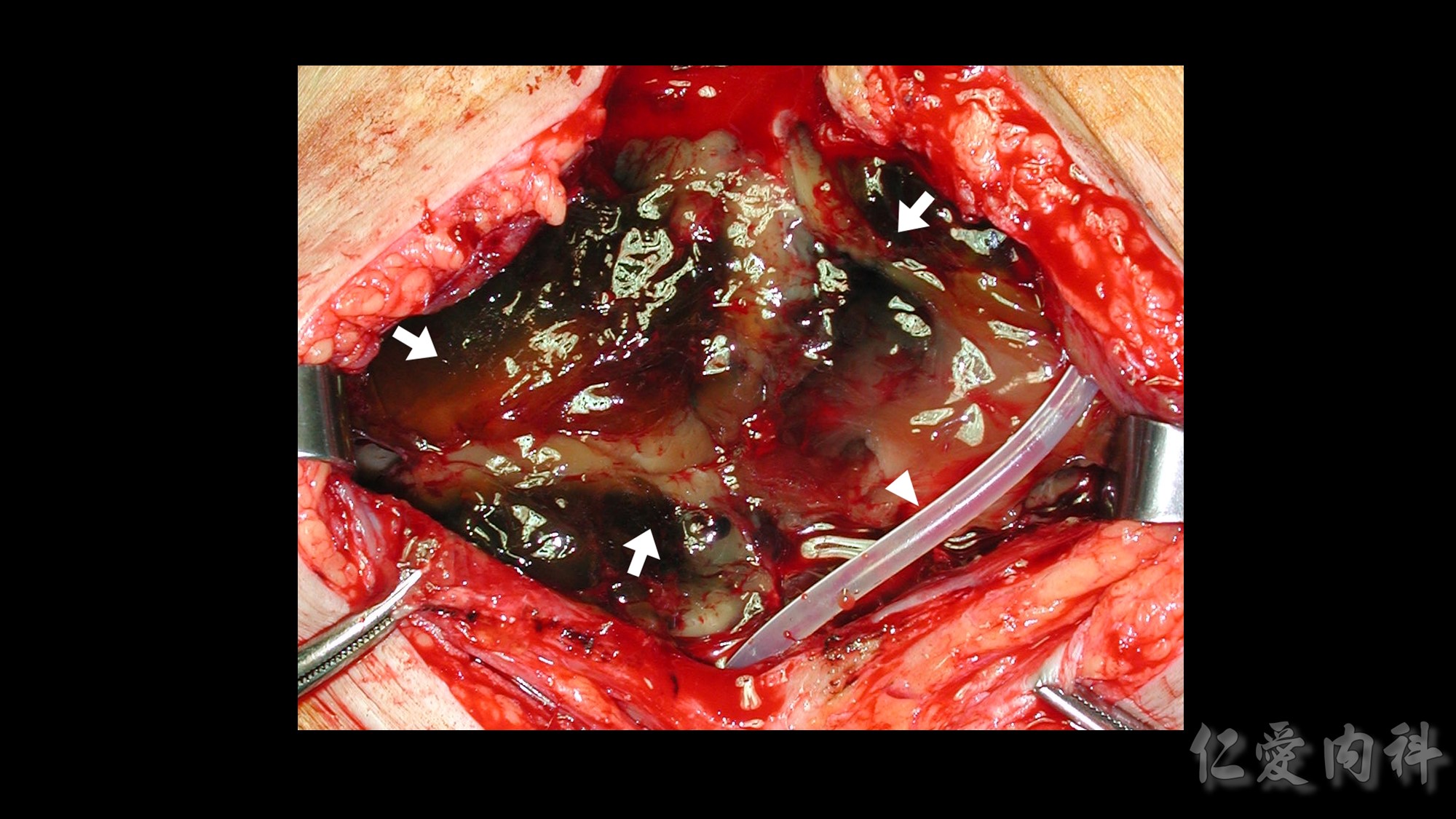
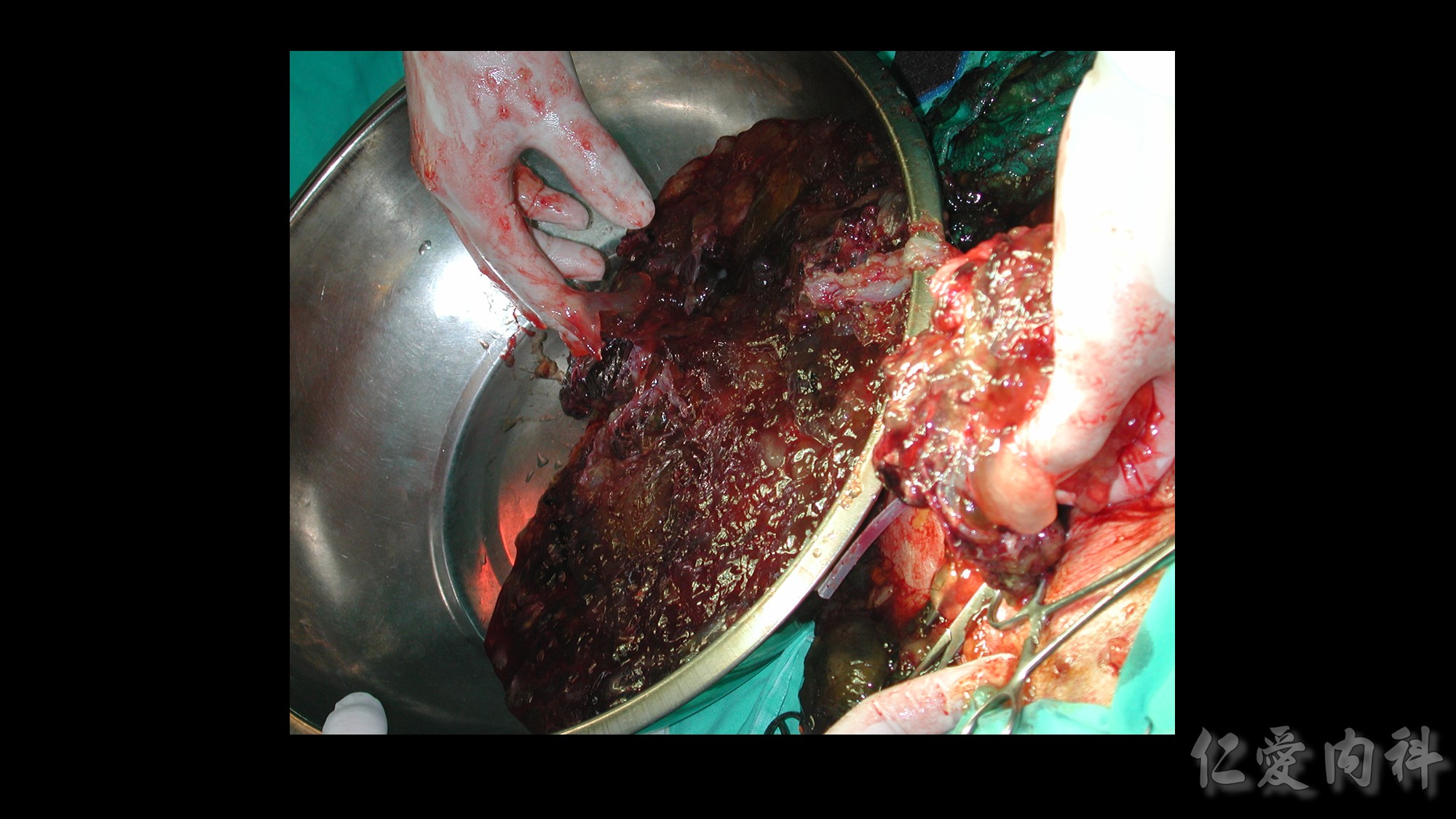
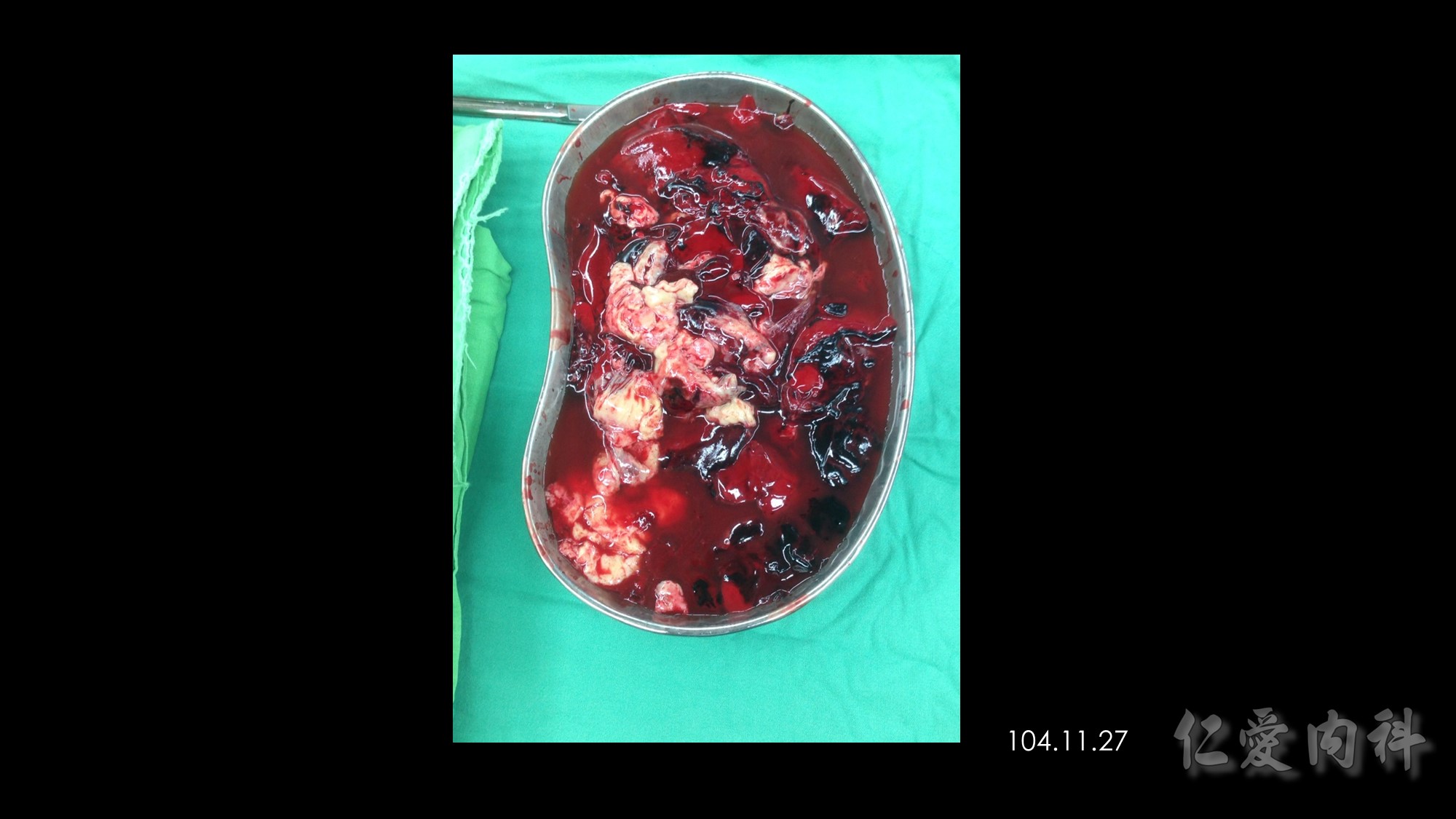
Diagnosis : encapsulating peritoneal sclerosis
following refractory bacterial peritonitis


















Members of each group used a nasal ointment twice daily for 5 consecutive days every 4 wk. The treatment group used calcium mupirocin 2% (Bactroban nasal; SmithKline Beecham, Welwyn Garden City, United Kingdom) and the control group used placebo ointment.
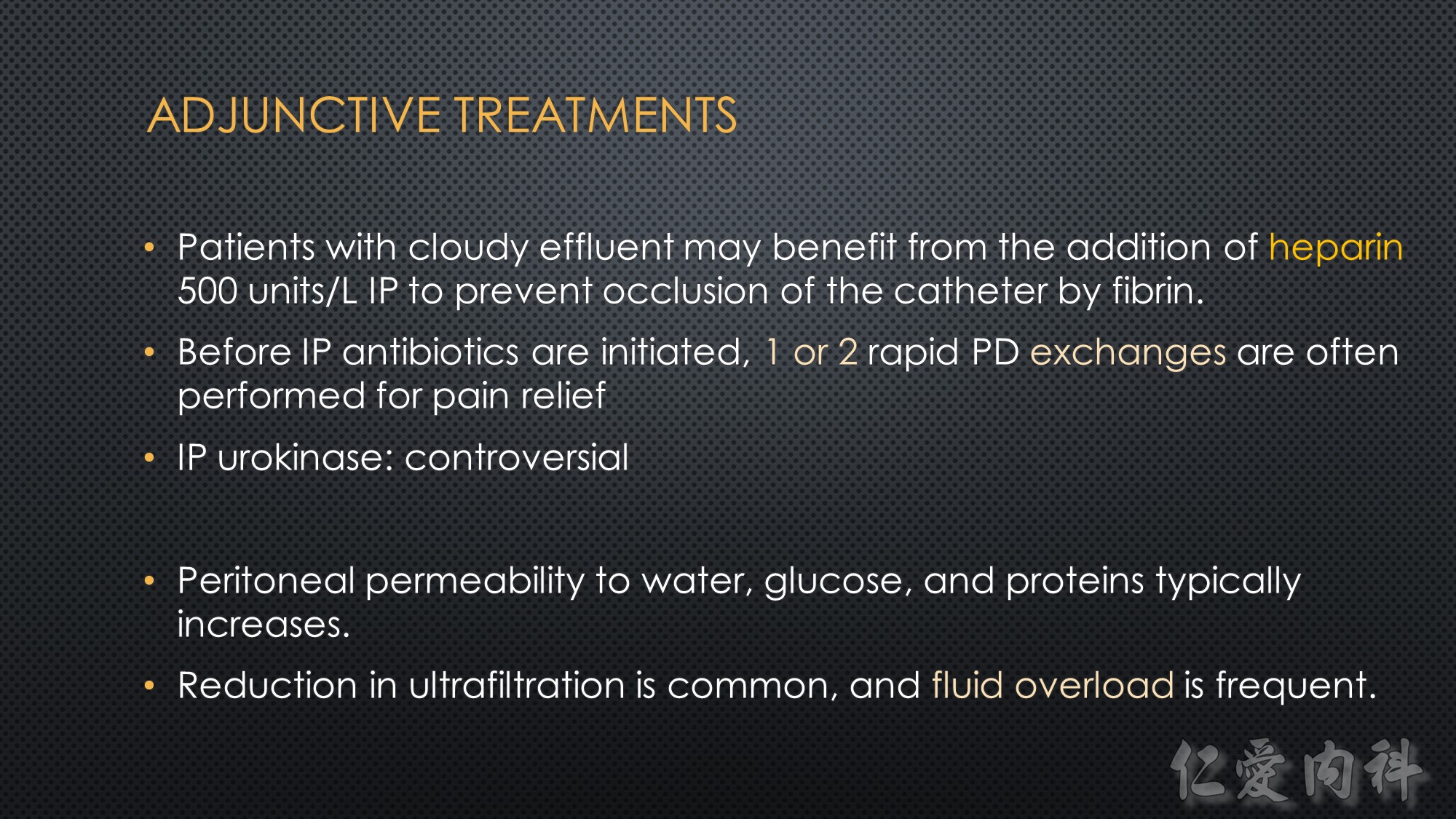
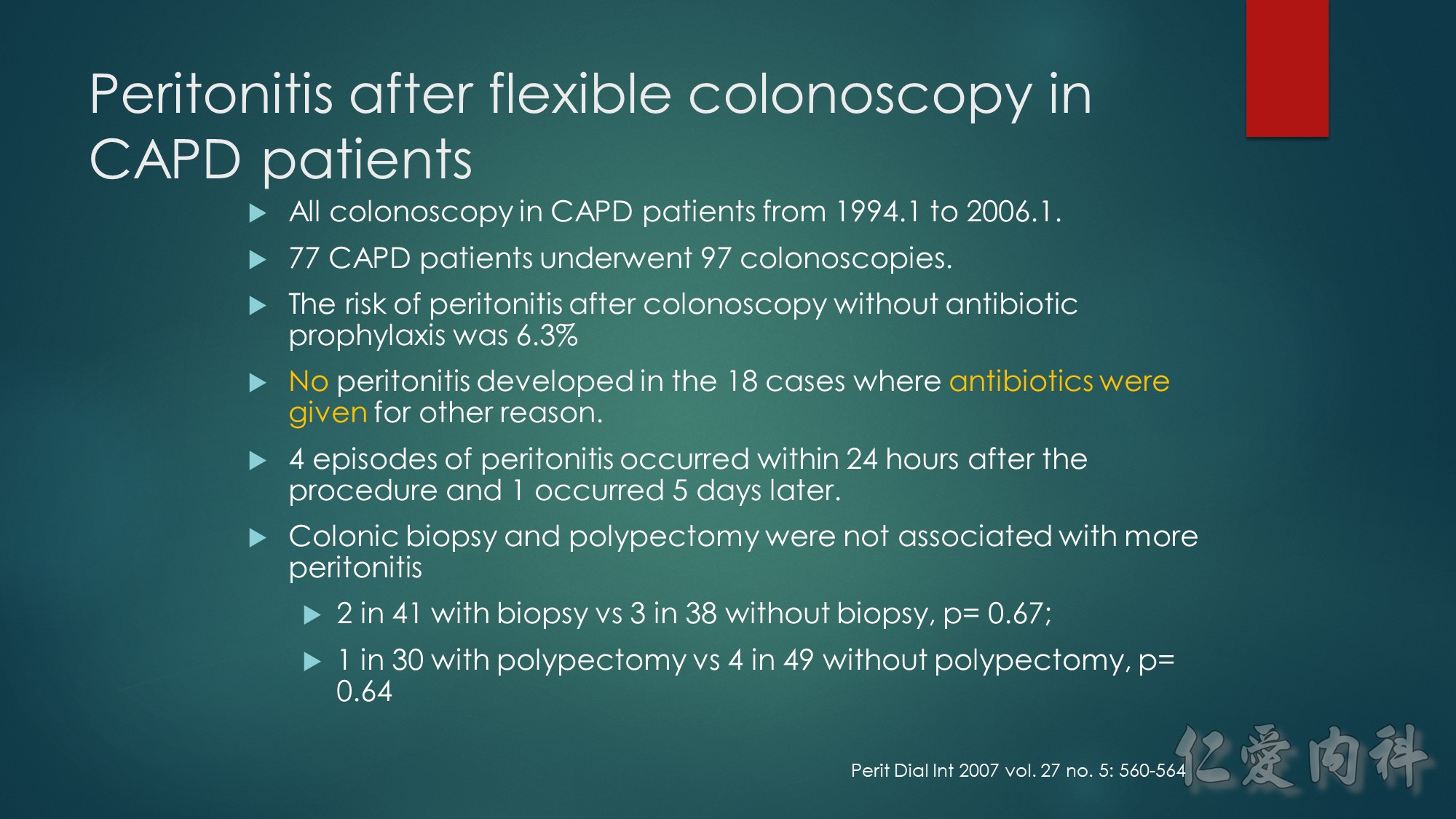
Although there is no compelling evidence to date that treatment of hypokalemia, constipation, or gastroenteritis reduces the rate of peritonitis, such problems, which are common in the PD setting, merit treatment in their own right.







A study of compliance
with the exchange procedure done at 6 months after the
start of PD found that most patients had begun to take
shortcuts or had simply veered off the prescribed steps
that they had been carefully taught at the start of PD