作者/講者: 王喬弘 醫師
整理: 陳羿方 醫師
校稿: Ian YC Chen, MD
上次校閱: 2019/02/25

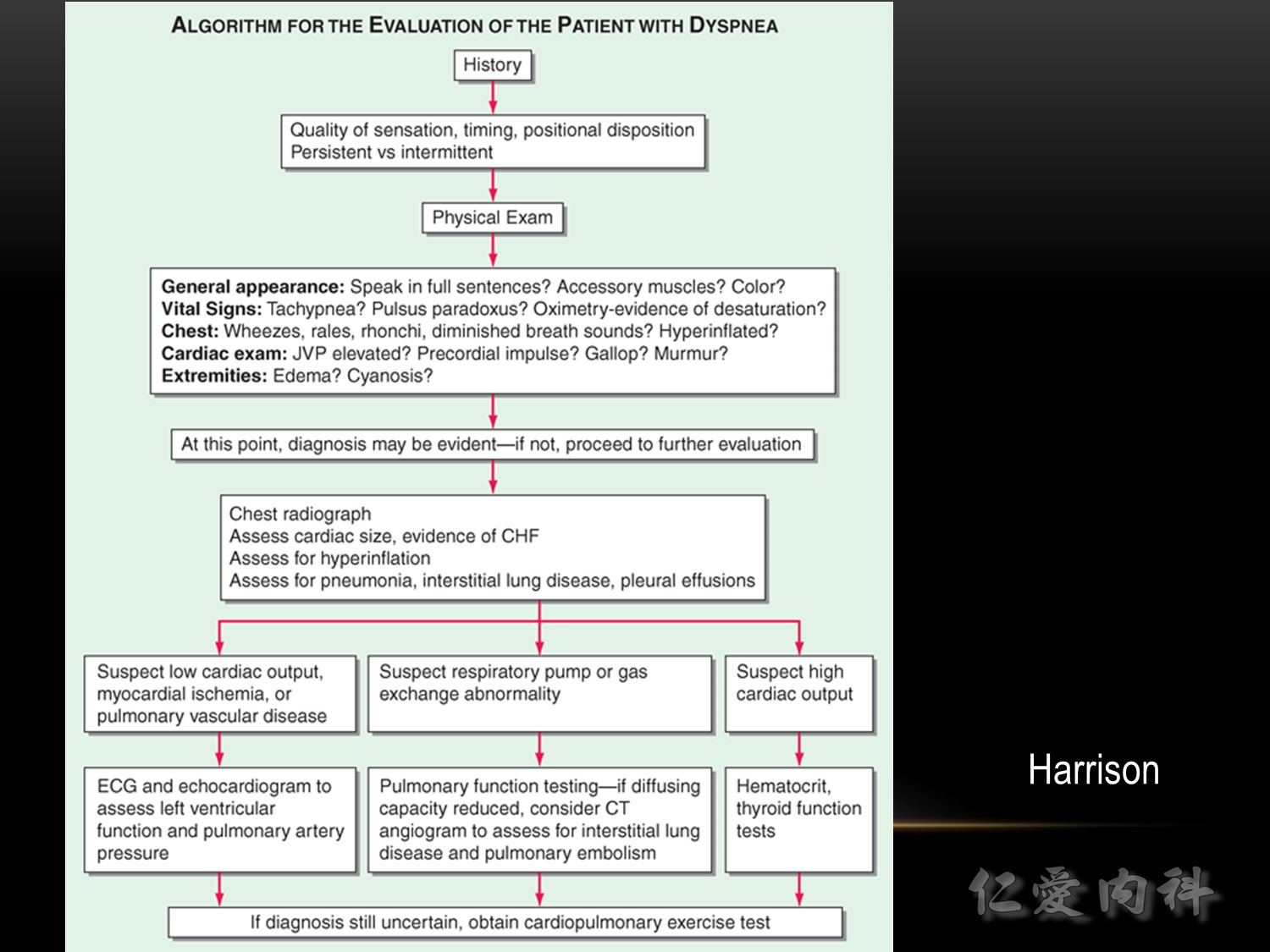
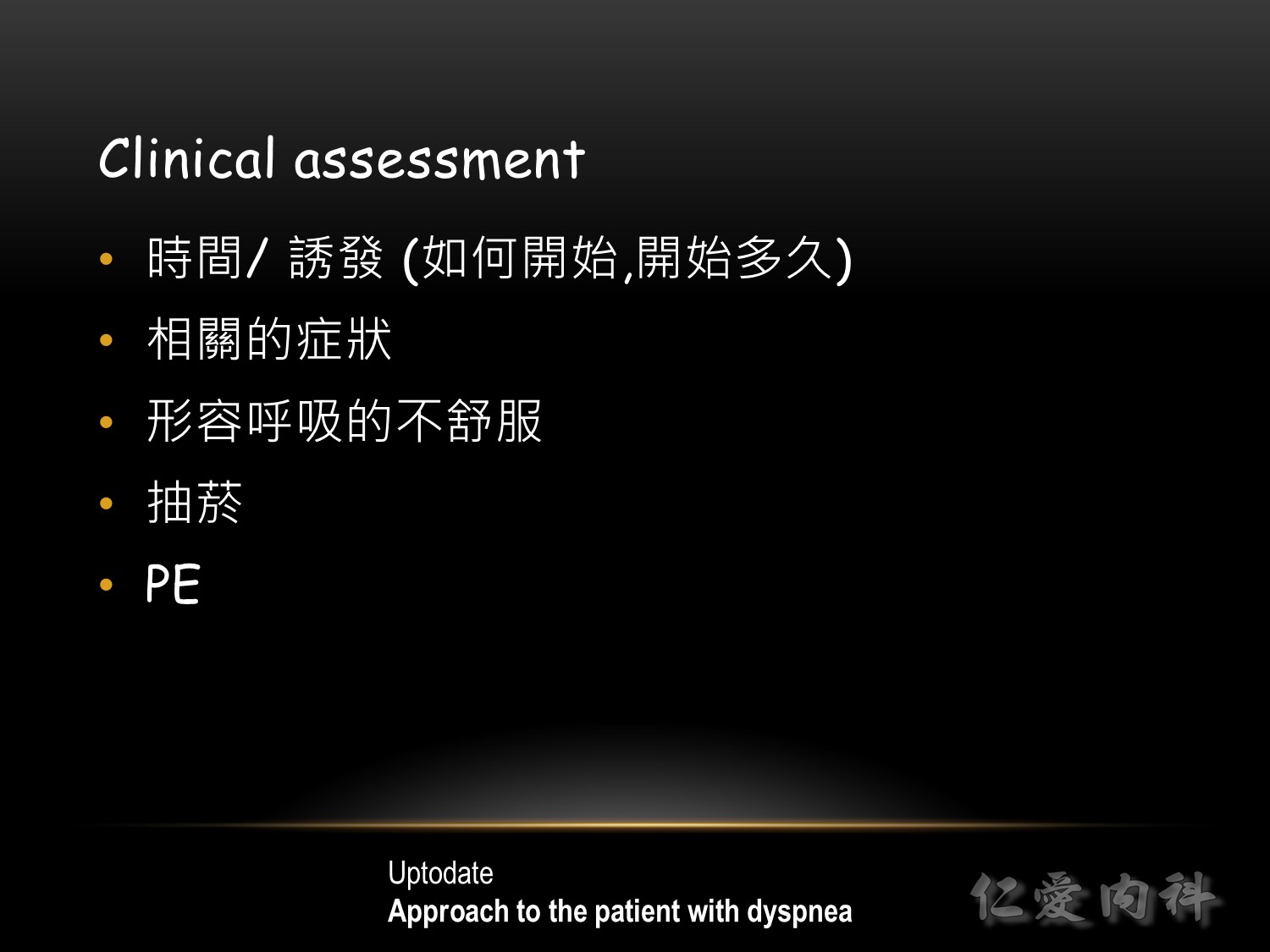
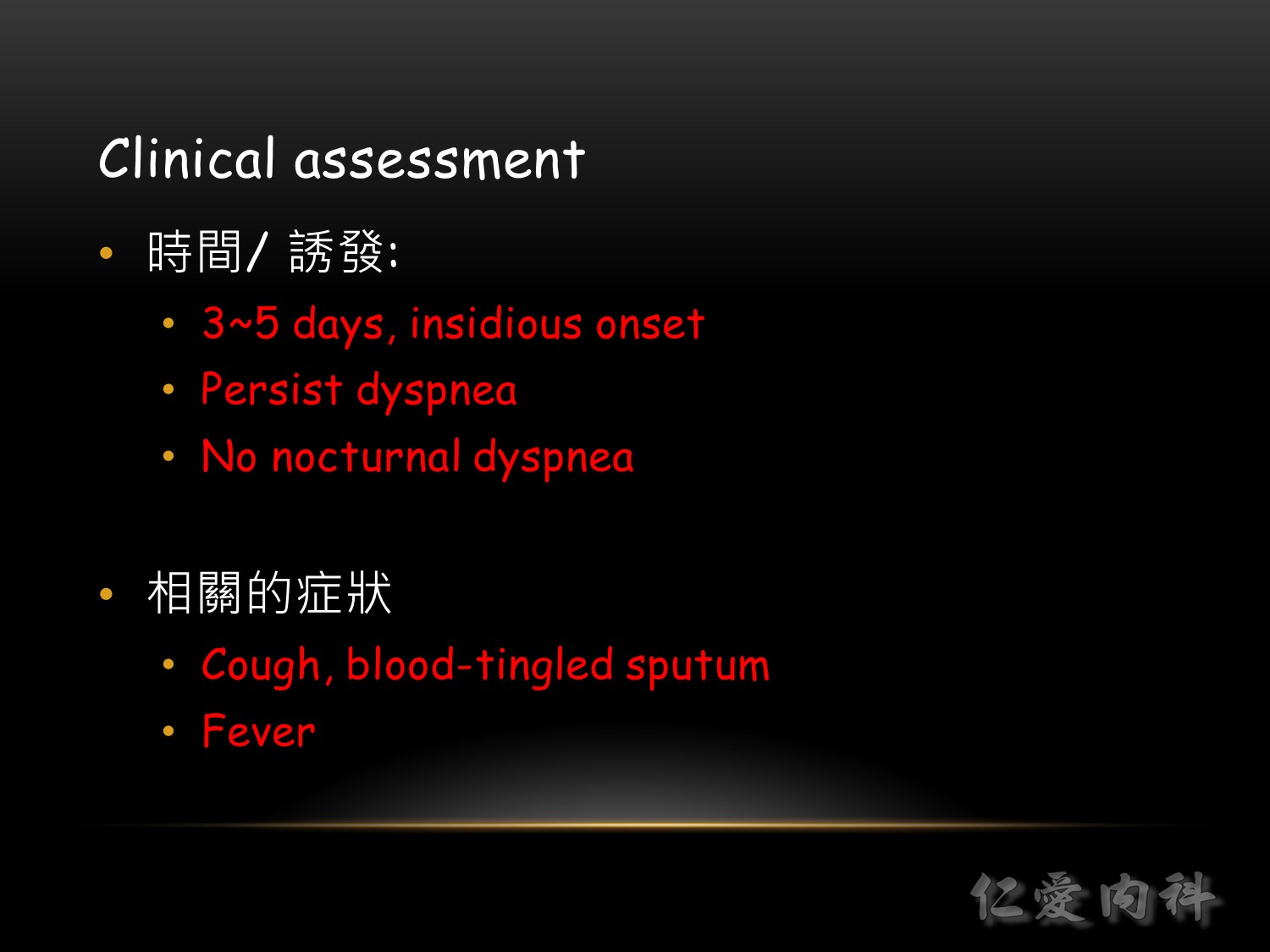
A more precise classification of the patient’s symptoms is helpful in the differential diagnosis. There are multiple criteria to be considered:
(1) Temporal
♥ acute onset, vs. chronic (present for more than four weeks), vs. acute worsening of pre-existing symptoms
♥ intermittent vs. permanent
♥ episodic (attacks)
(2) Situational
♥ at rest
♥ on exertion
♥ accompanying emotional stress
♥ depending on body position
♥ depending on special exposure(s)
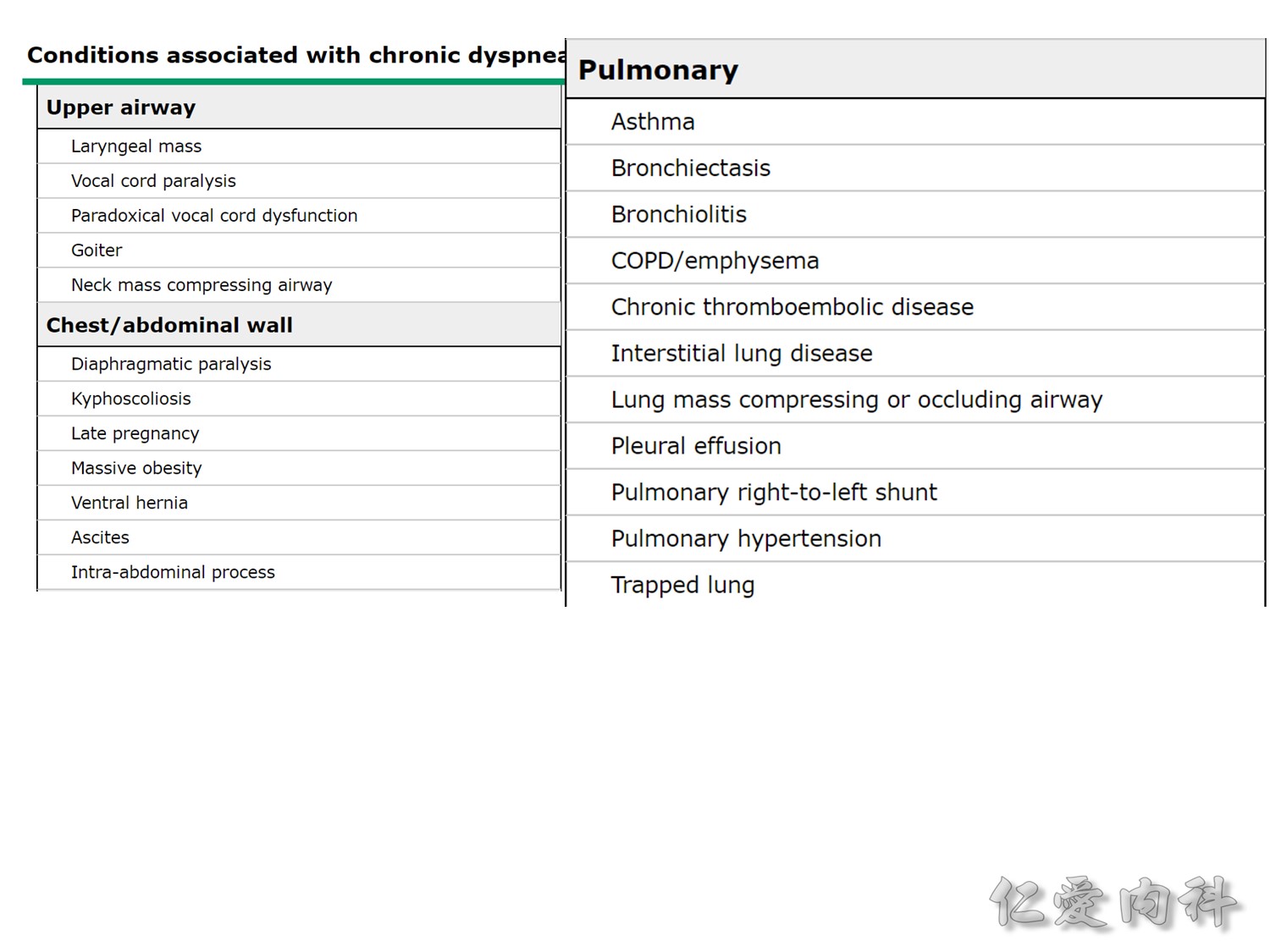
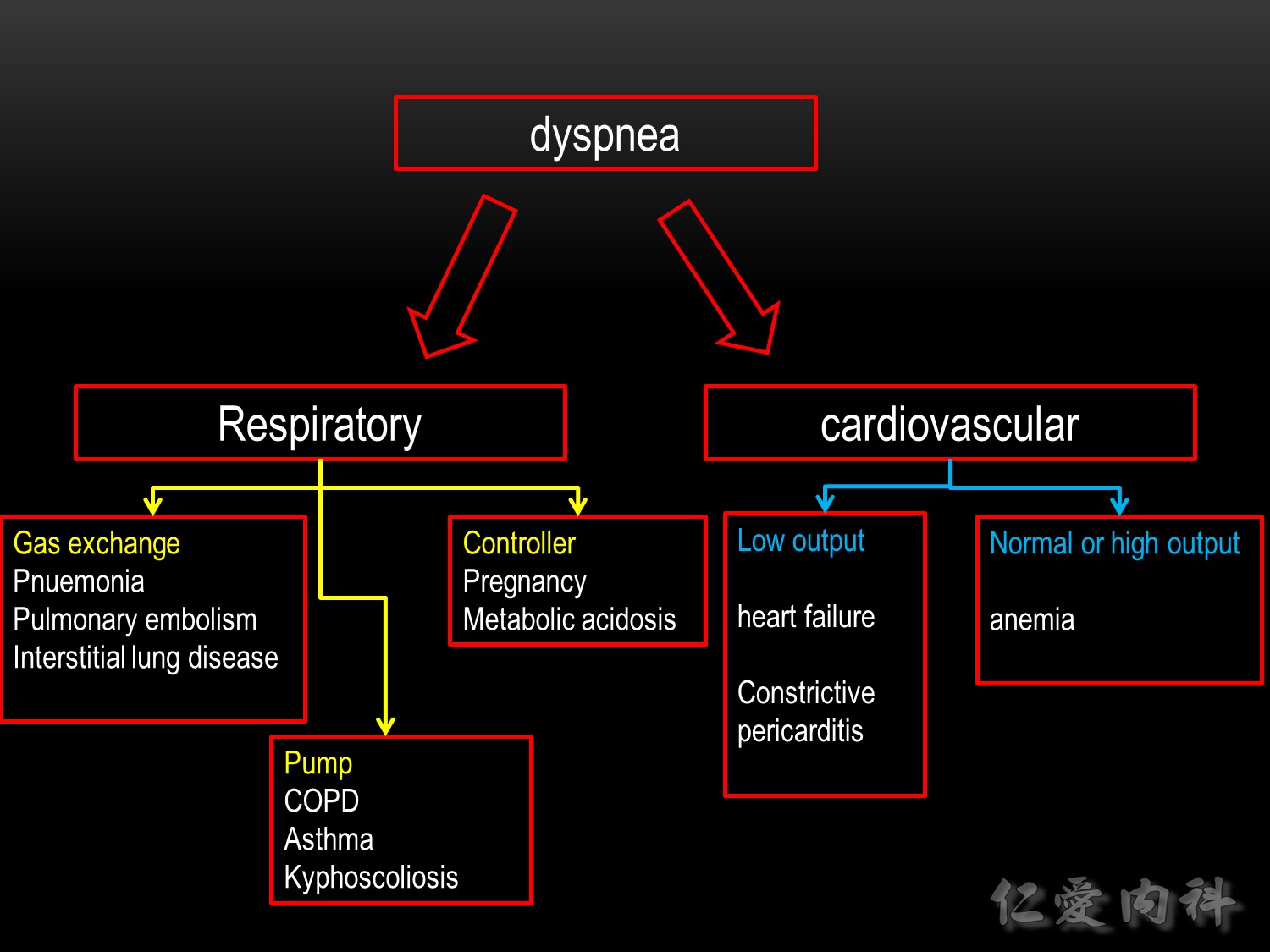
(3) Pathogenetic
♥ problems relating to the respiratory system (central control of breathing, airways, gas exchange)
♥ problems relating to the cardiovascular system
♥ mixed cardiac and pulmonary causes
♥ other causes, e.g., anemia, thyroid disease, poor physical condition (i.e., muscle deconditioning)
♥ mental causes
The diagnosis and treatment of dyspnea are sometimes made more difficult by the simultaneous presence of more than one underlying disease, particularly in elderly, multimorbid patients.
Ref: The Differential Diagnosis of Dyspnea
Dominik Berliner, Nils Schneider, Tobias Welte, Johann Bauersachs, Dtsch Arztebl Int. 2016 Dec; 113(49): 834–845.
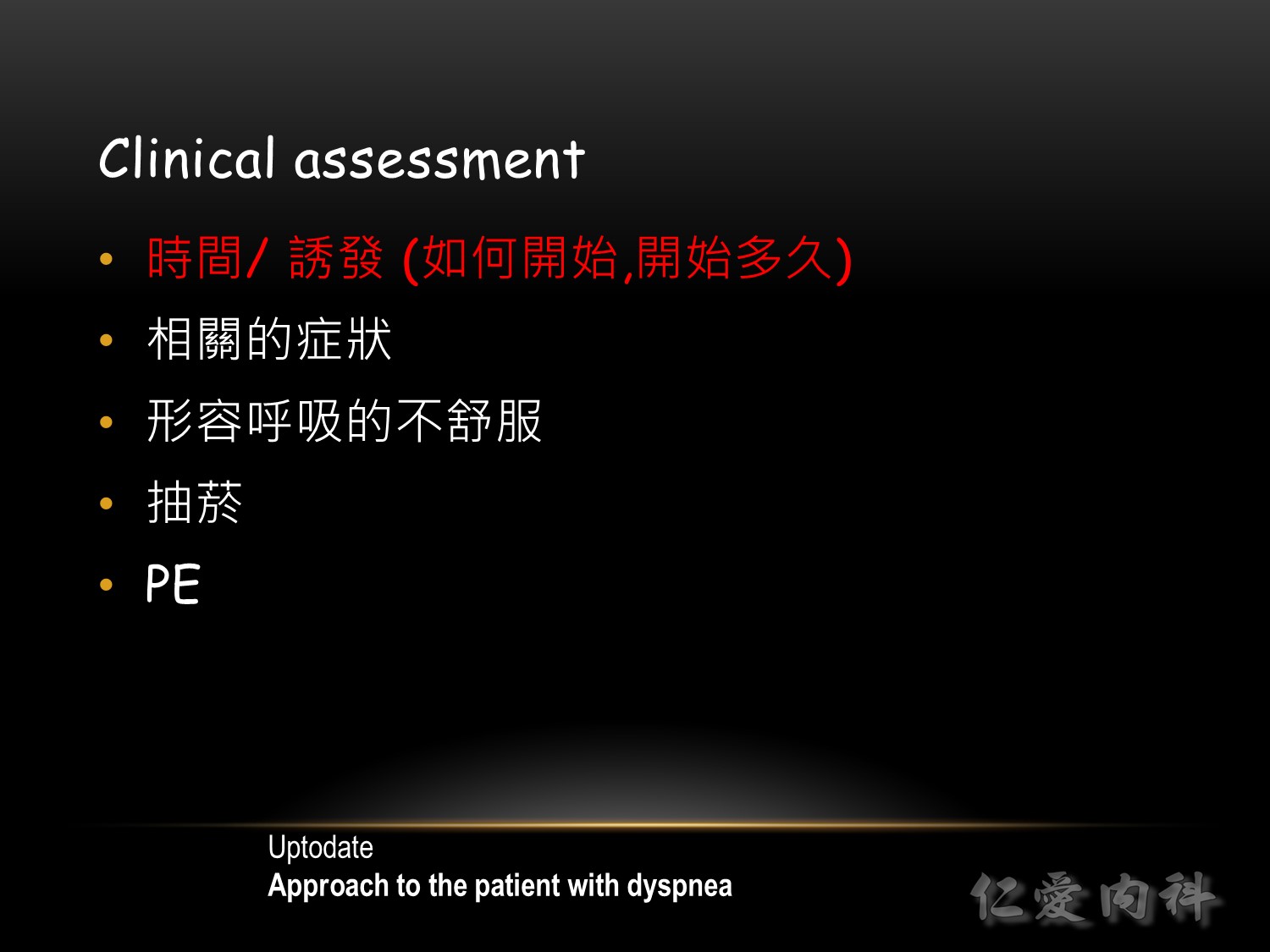
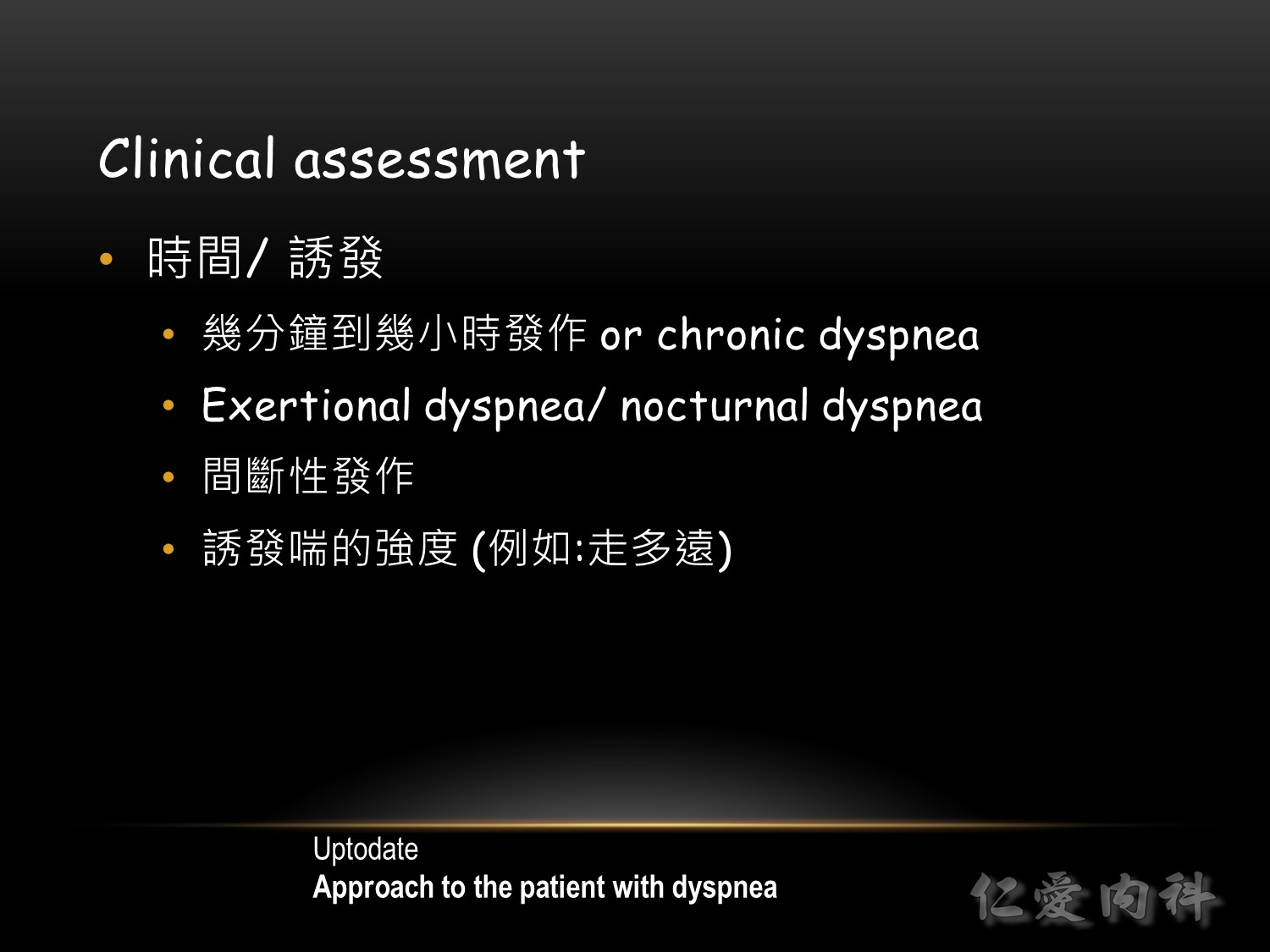
病人如果走 15-30 meters (50-100 feet) 就會喘,通常都有急性肺微血管楔型壓升高 (elevated pulmonary capillary wedge pressure) 或是肺動脈高壓 (pulmonary hypertension)。而運動引發之 asthma 常常需要更高強度的運動約 3 分鐘後發生,在 10~15 分鐘內達到高峰。
需問清楚散步走多久?樓梯爬幾層樓會導致呼吸困難?這可用來評估其嚴重度。


(1) 突然的劇痛:有可能是因為發生氣胸、肺栓塞,主動脈剝離,急性心肌梗塞
(2) 發燒,黃痰 (可能是感染)
(3) 體重減輕,咳血:可能是腫瘤或結核造成
在問完病史後,有了初步的 differential diagnoses 後,通常可進一部安排相關檢查,包括胸部 X 光、動脈血、常規血液、心電圖、肺功能等檢查 (佐證你的想法,切忌一開始就採取亂槍打鳥式的做法)。
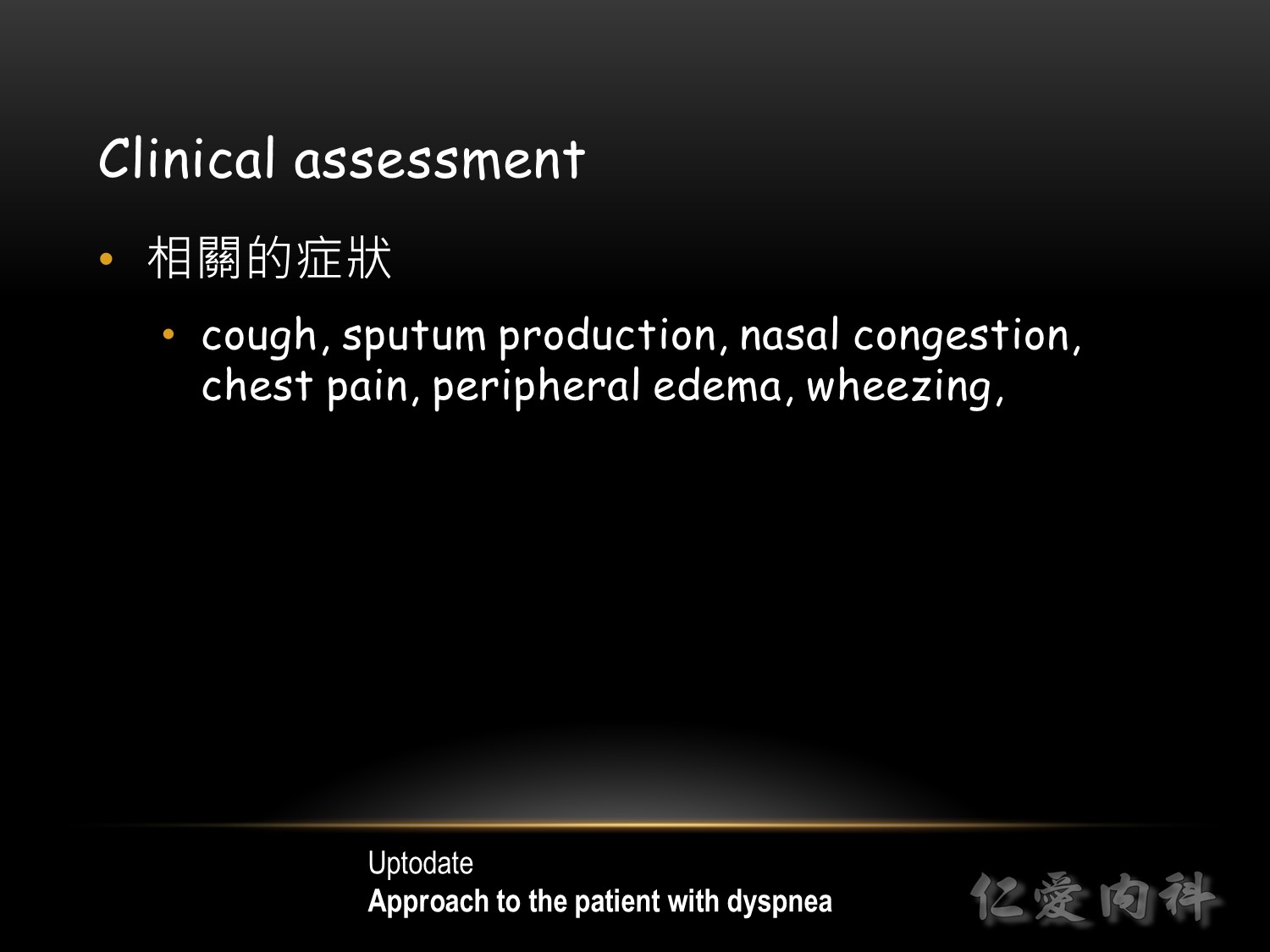
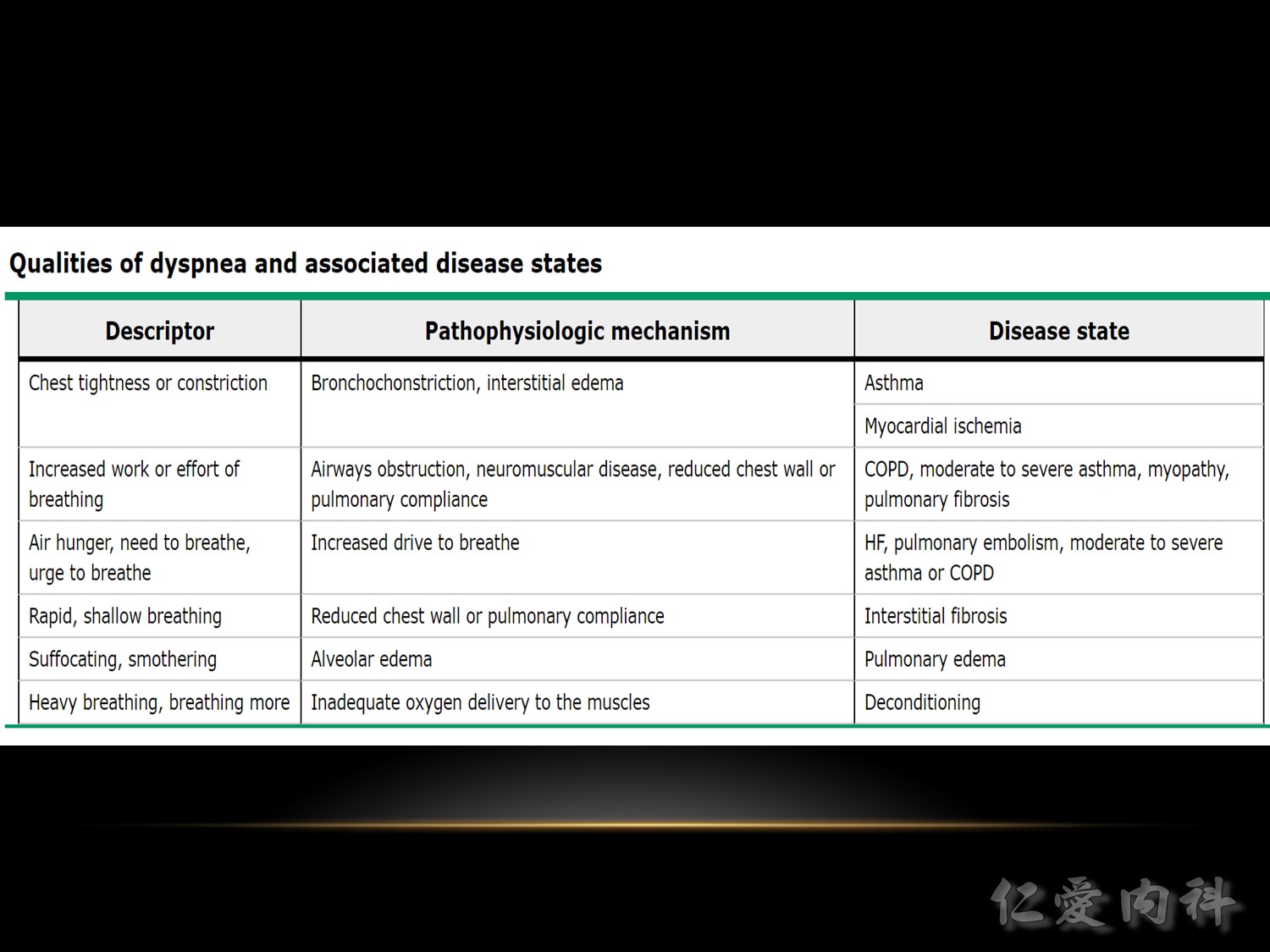
(1) 胸部緊、悶的感覺可能是由於氣喘病或者心絞痛造成。心絞痛的痛可能傳到左肩或下巴,也可能會有合併冒冷汗之現象。
(2) 覺得需要用力才喘得起來(呼吸道阻塞或者神經肌肉疾病或者肺部或胸壁彈性變差的問題 )
(3) 當躺下或者坐著時會比較容易呼吸困難;前者較像是心臟或者肺部之問題





♥ Inspection
Inspect patient, comment on respiratory status, conjunctiva (pale or not).
State that weight should be measured for BMI/fluid overload status.
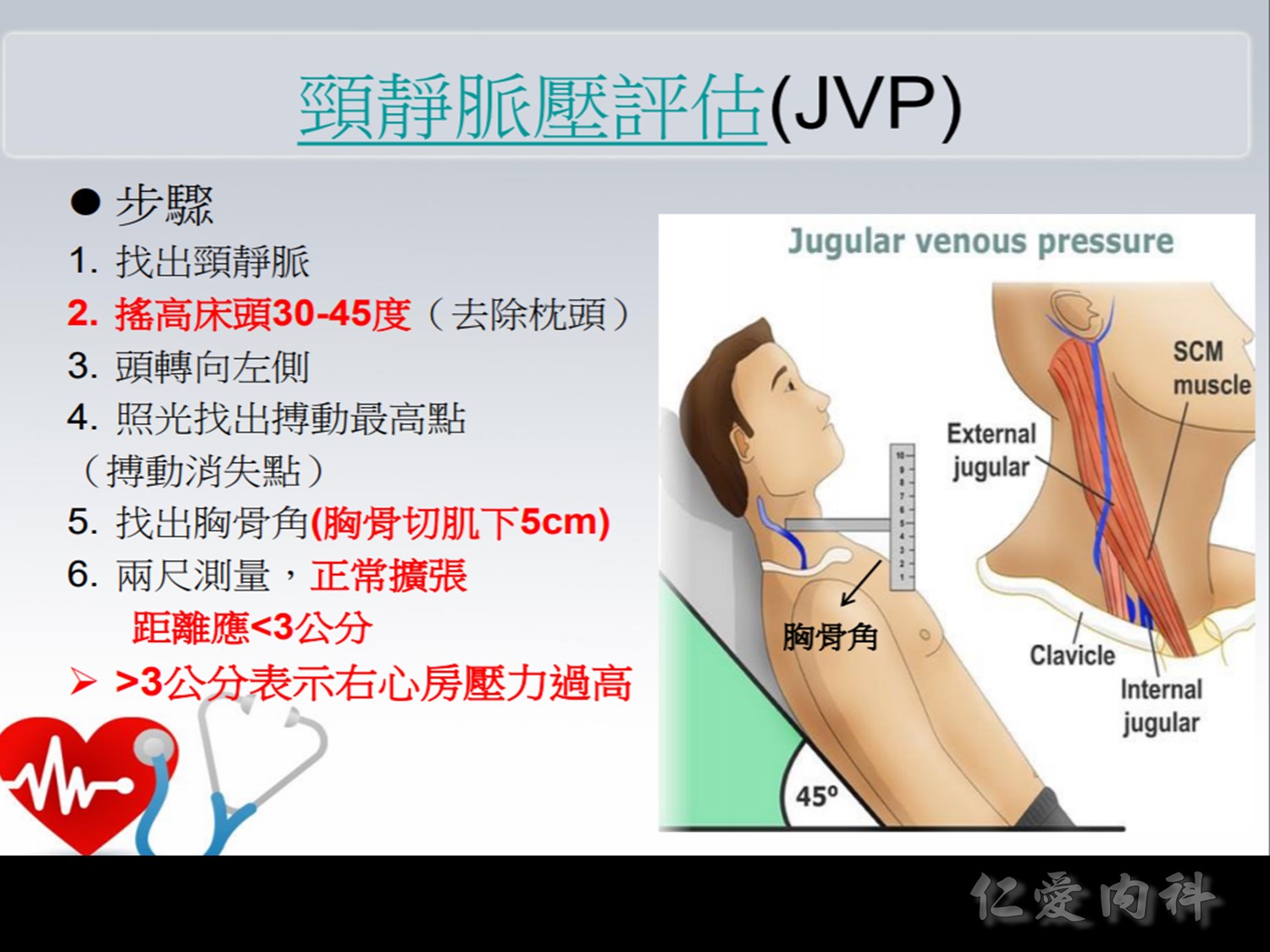
♥ Volume Status
Examine lower extremities for pitting edema.
Examine JVP and comments on its estimated height.
Measure pulse, comments on rate and rhythm.
Evaluate patient’s orthostatic vitals.
Examine the abdomen for ascites and a pulsatile liver, indicating right heart failure.
♥ Pre-cordium/Carotid
Palpate for the presence of thrills, heaves.
Palpate PMI and comments on size, amplitude, duration, and location.
Auscultate in all 4 areas of precordium with bell and diaphragm.
Comment on presence of murmurs, extra heart sounds.
Examine carotid arteries for bruits.
♥ Respiratory
Percusse posterior chest, comment on dullness.
Auscultate all lung fields, commenting on presence of crackles, wheeze or other adventitious breath sounds.
 如果到 paradoxical 就是快呼吸衰竭了
如果到 paradoxical 就是快呼吸衰竭了
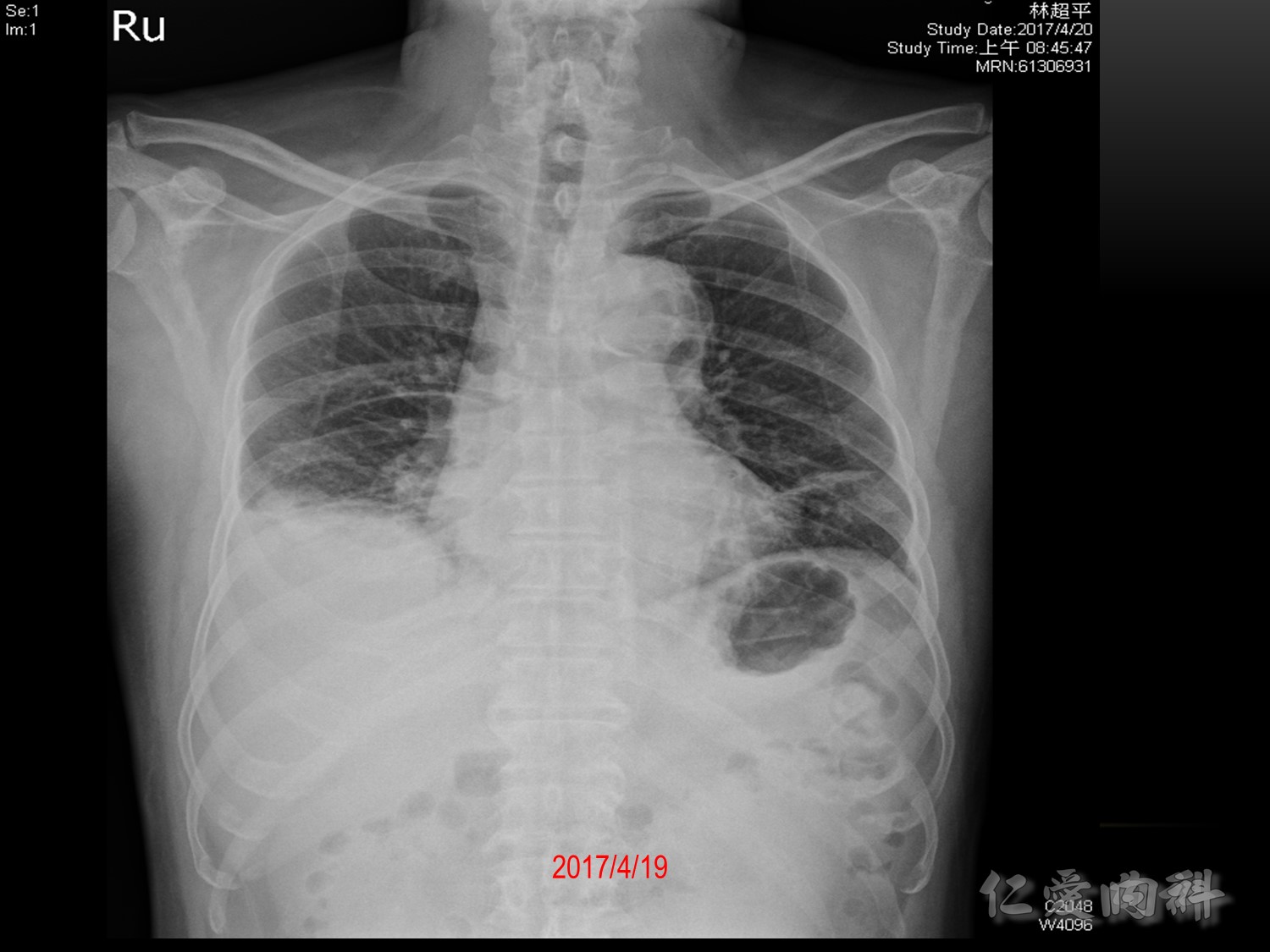
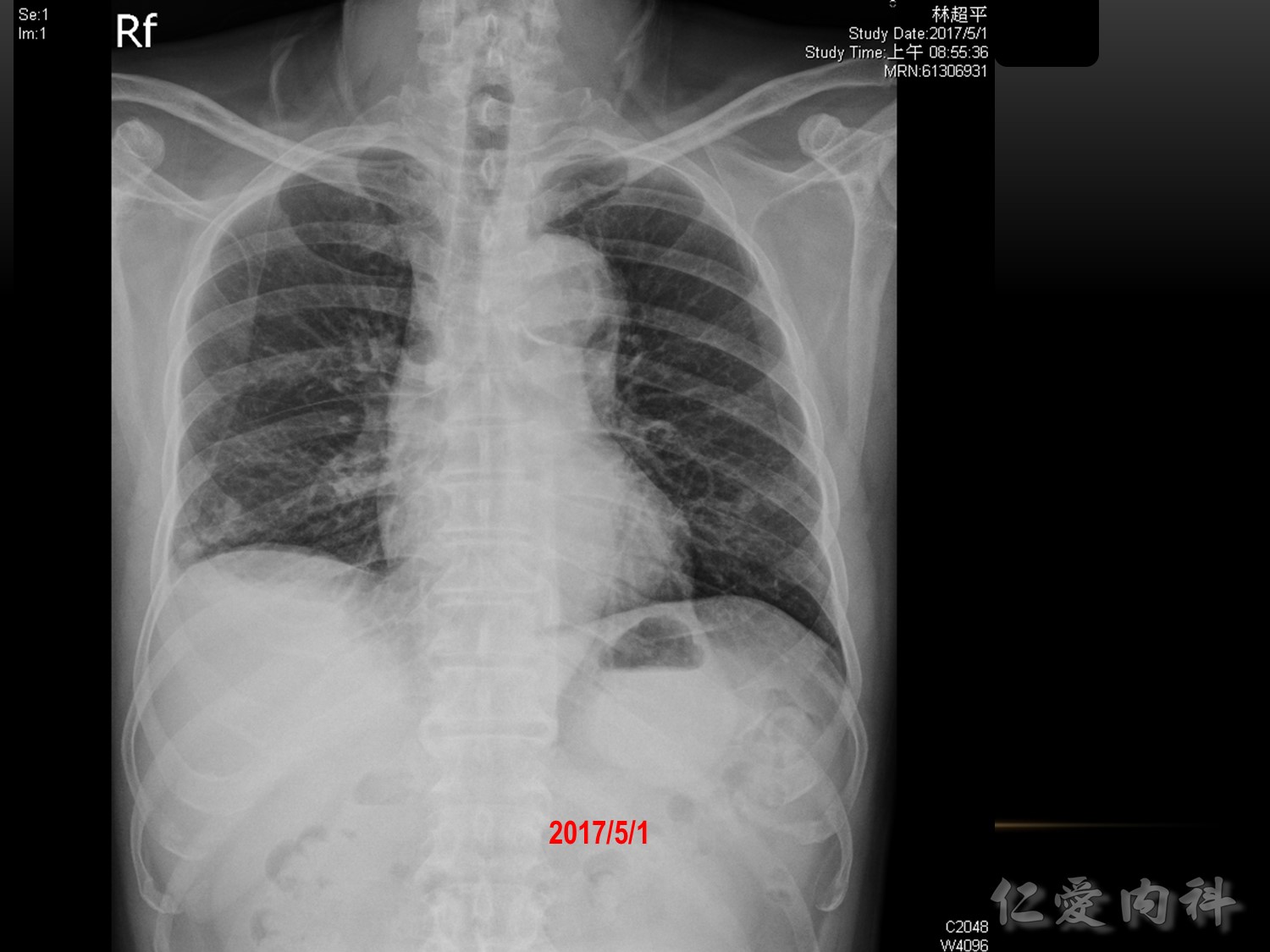
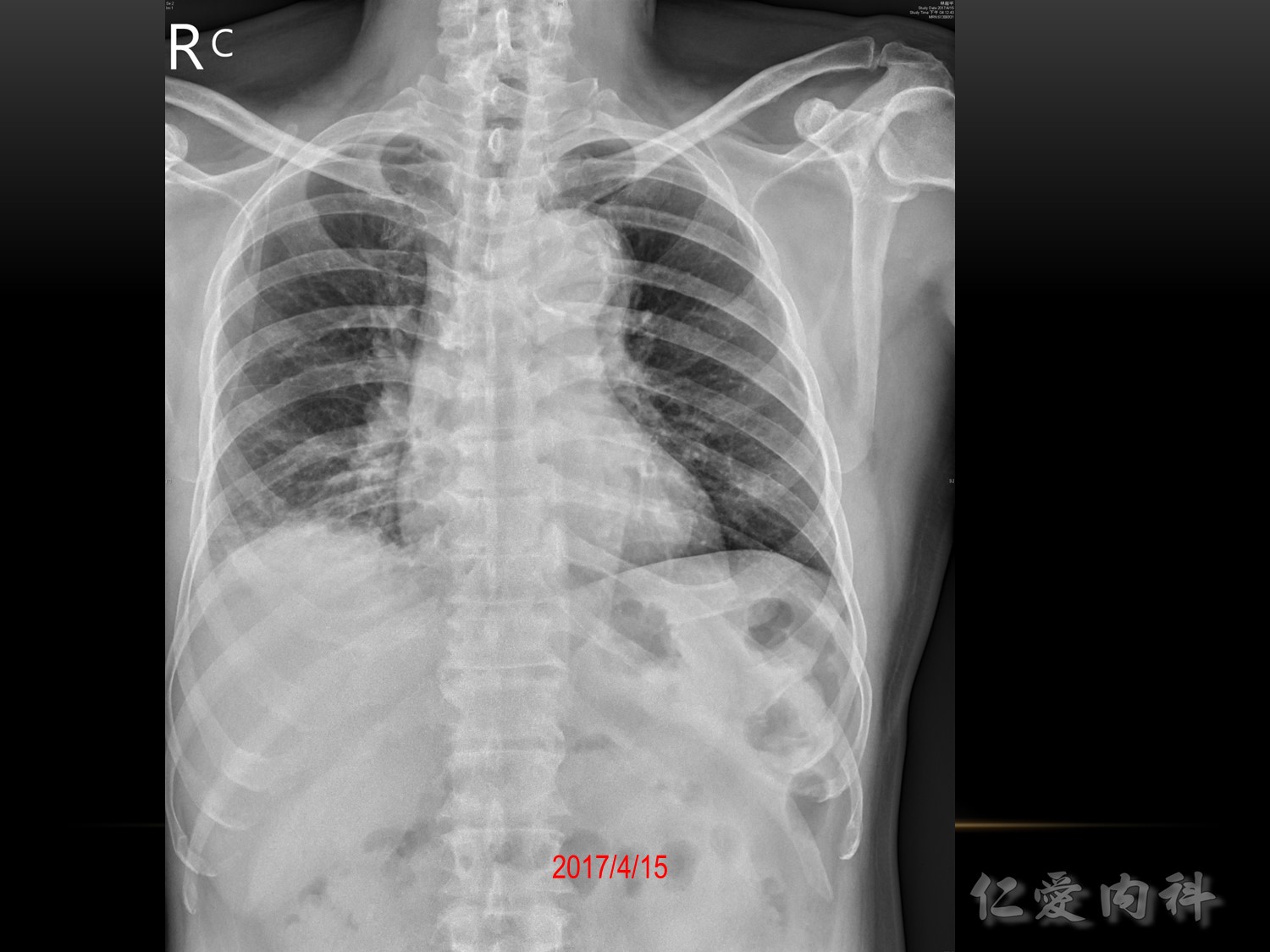
Chest X-ray interpretation
Confirm details
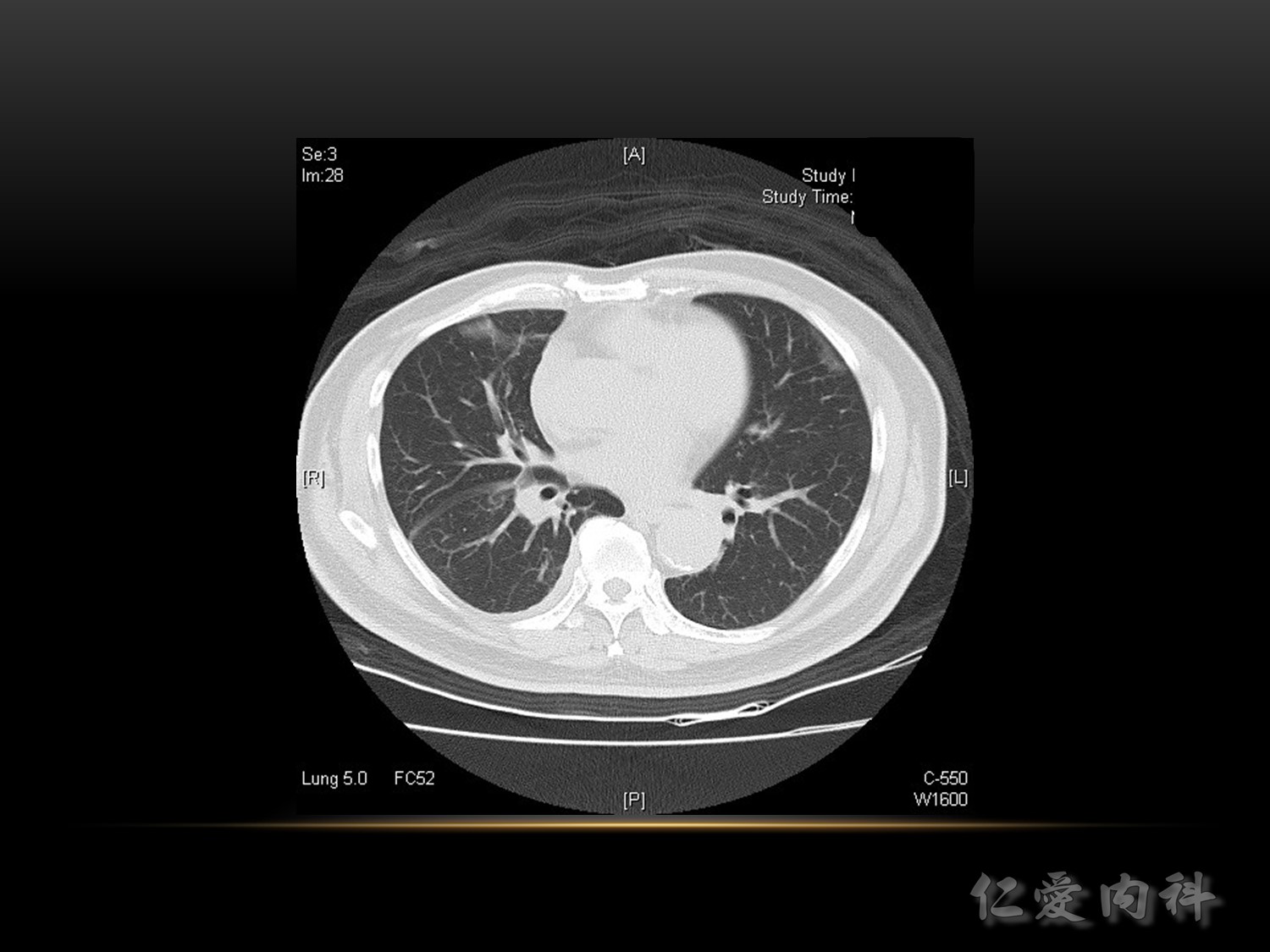
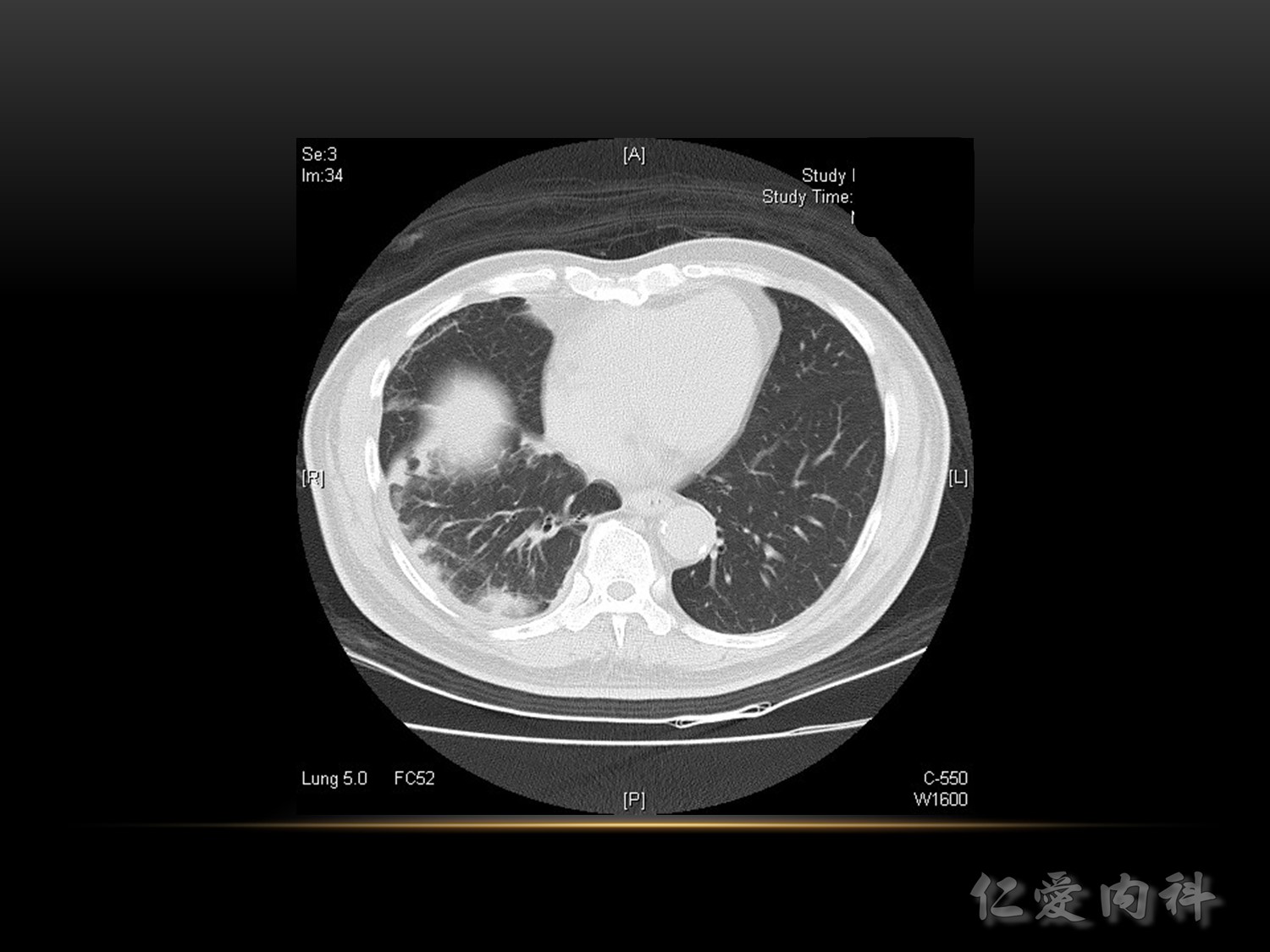
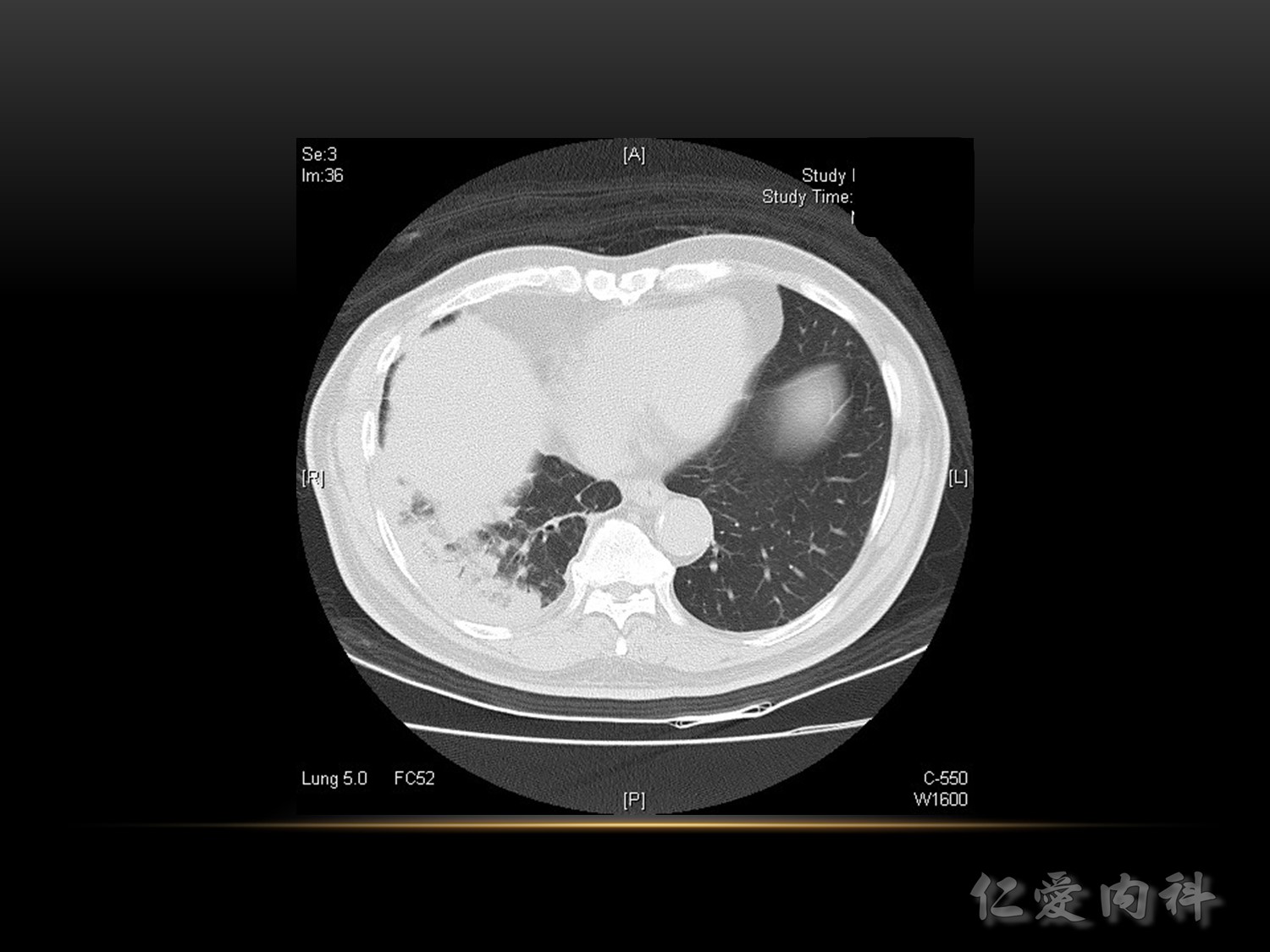
Image quality: 吸氣沒有吸飽
Airway、Breathing、Cardiac、Diaphragm、Everything else
Ref: https://geekymedics.com/chest-x-ray-interpretation-a-methodical-approach/

要住院嗎?
CURB-65
https://www.mdcalc.com/curb-65-score-pneumonia-severity


吸氣一樣吸得不好,左下: linear, band like, sputum 卡住

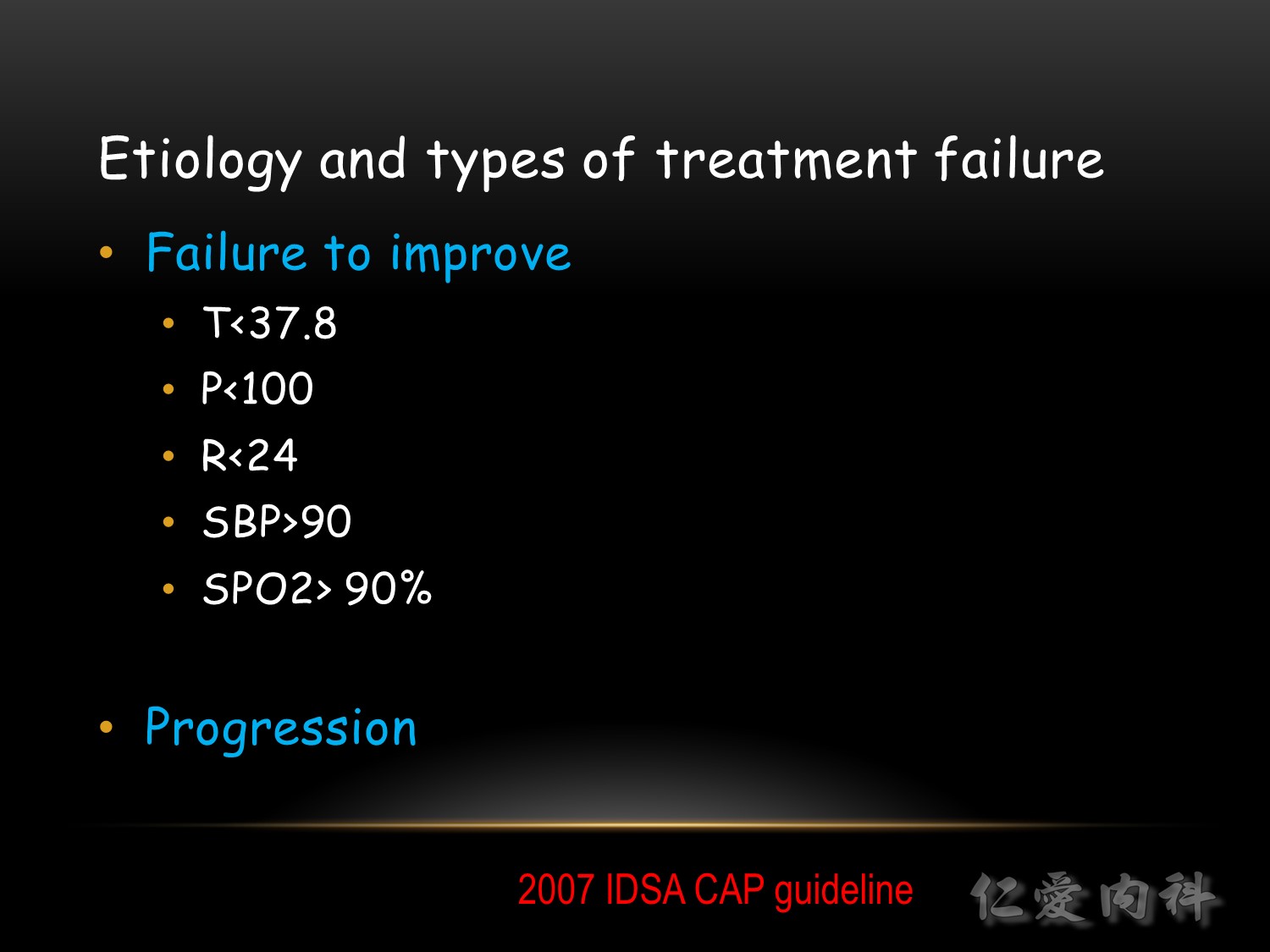

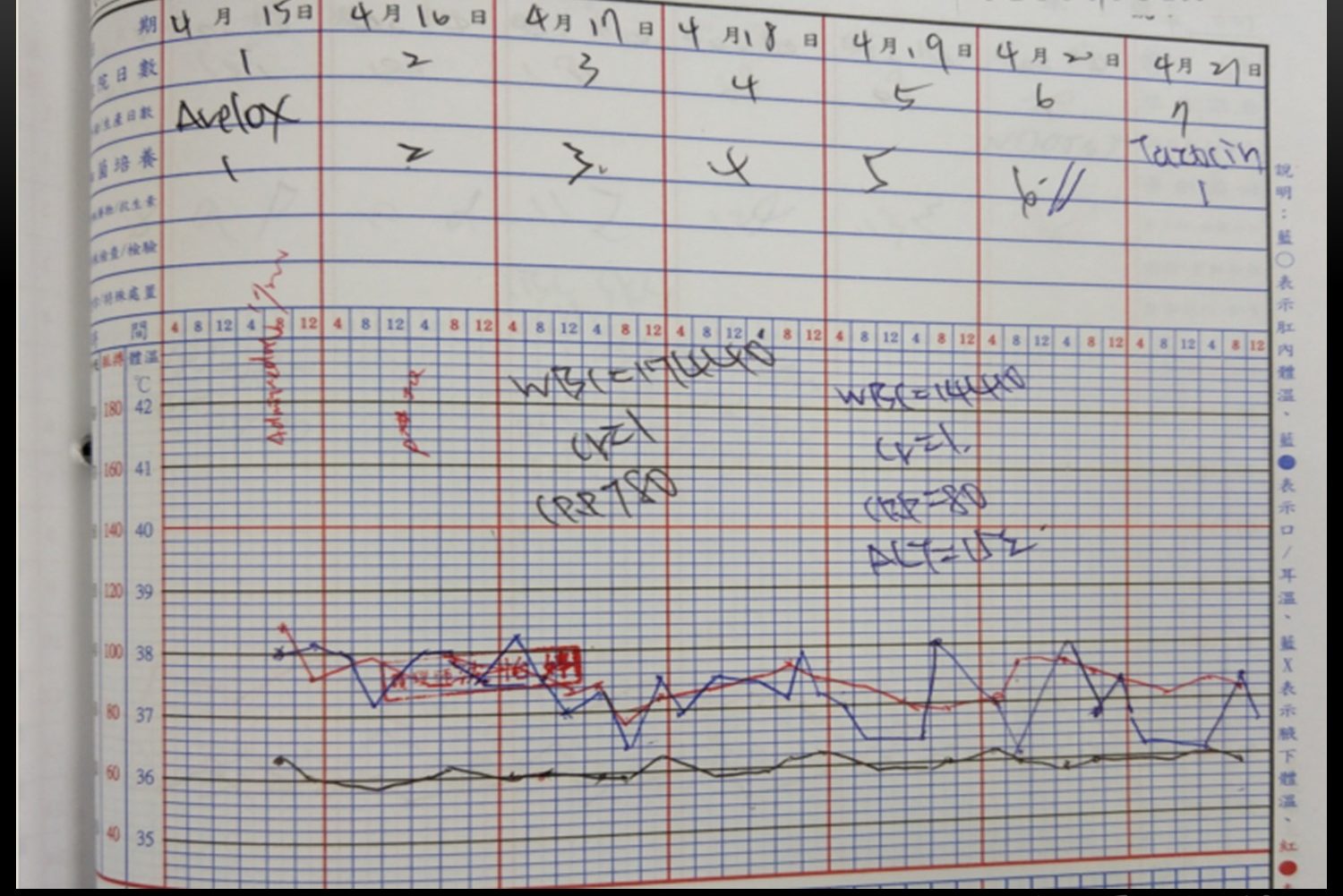
如果大於 72 小時臨床上沒有改善,可能要考慮:
♣ Resistant microorganism
♣ Uncovered pathogen
♣ Parapneumonic effusion/empyema
♣ Nosocomial superinfection
♣ Misdiagnosis: PE, CHF, vasculitis, COP
♣ Drug fever









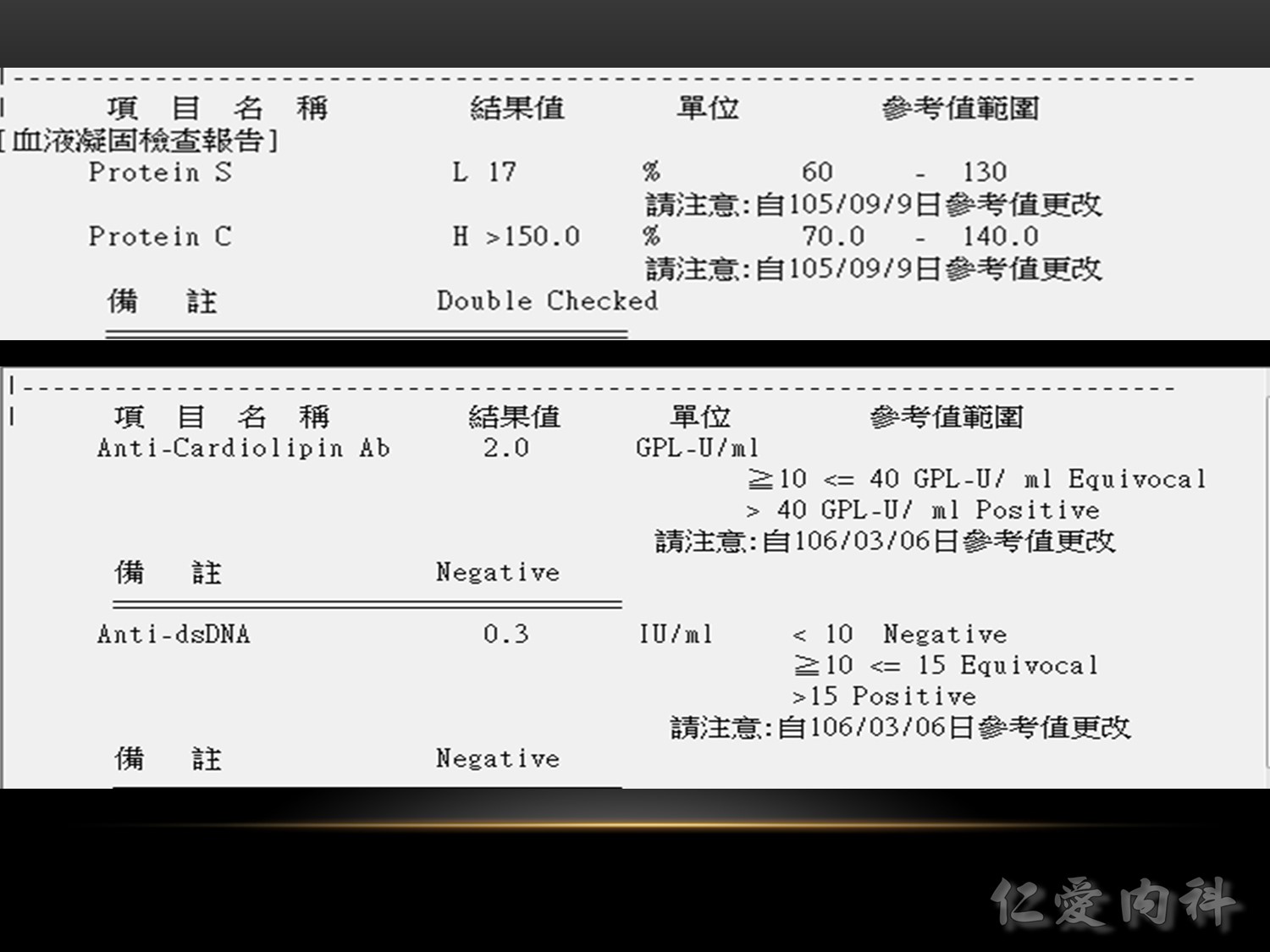
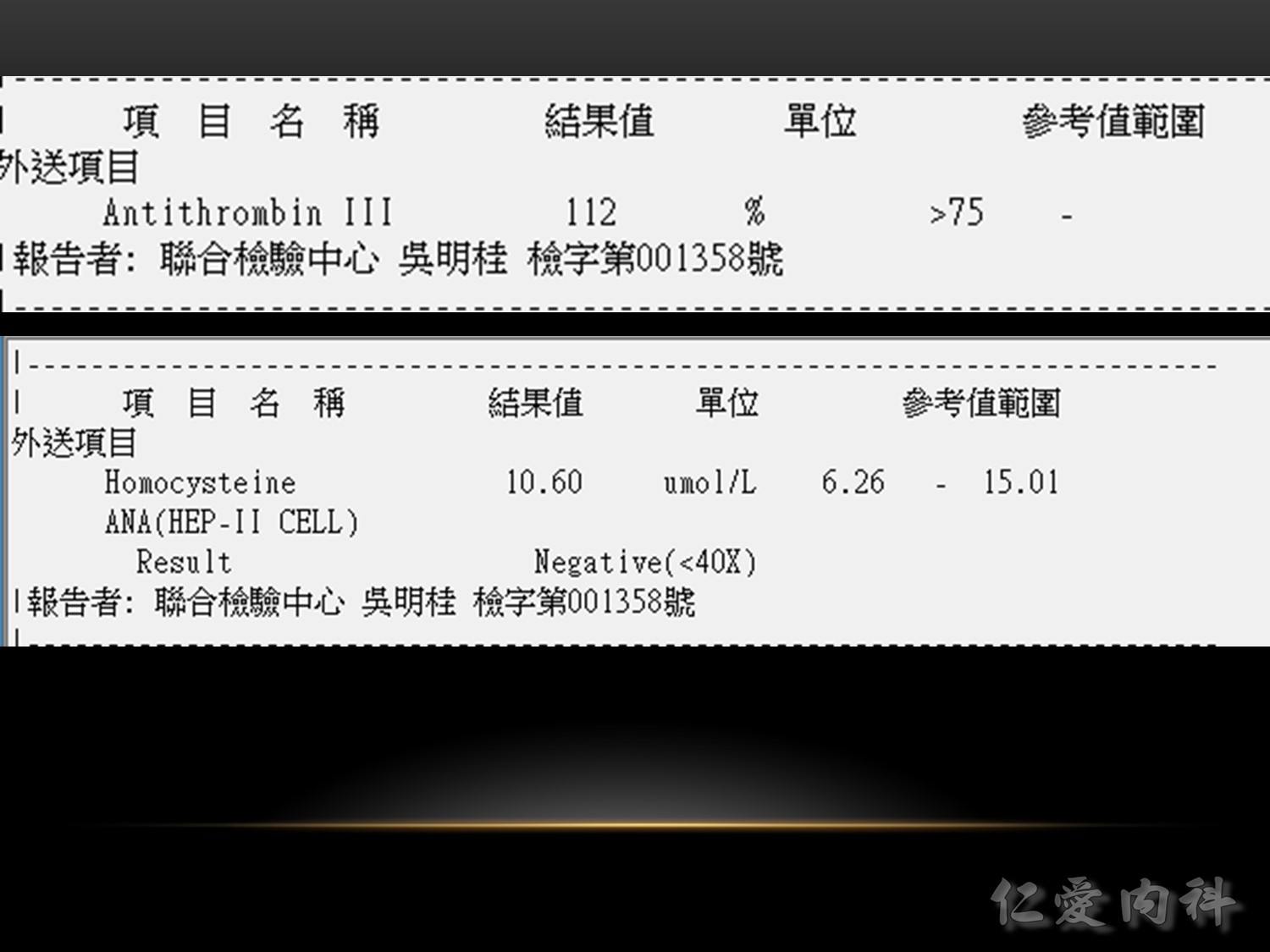
VTE 的誘發風險 :
藥品/醫療:荷爾蒙避孕藥、荷爾蒙補充療法、癌症化學治療、手術。
生活型態:長期不動 (immobilization)、肥胖、男性 (男性也算生活型態?)、高齡。
疾病:外傷、發炎性腸疾病、凝血功能異常、慢性心臟衰竭、慢性肺疾病、癌症、靜脈栓塞病史。
其中,凝血功能異常包括:抗磷脂質症候群 (antiphospholipid syndrome, APS)、factor V Leiden異常、凝血酶原 (prothrombin) G20210A 基因突變等。
Ref: http://jerryljw.blogspot.com/2016/05/blog-post.html

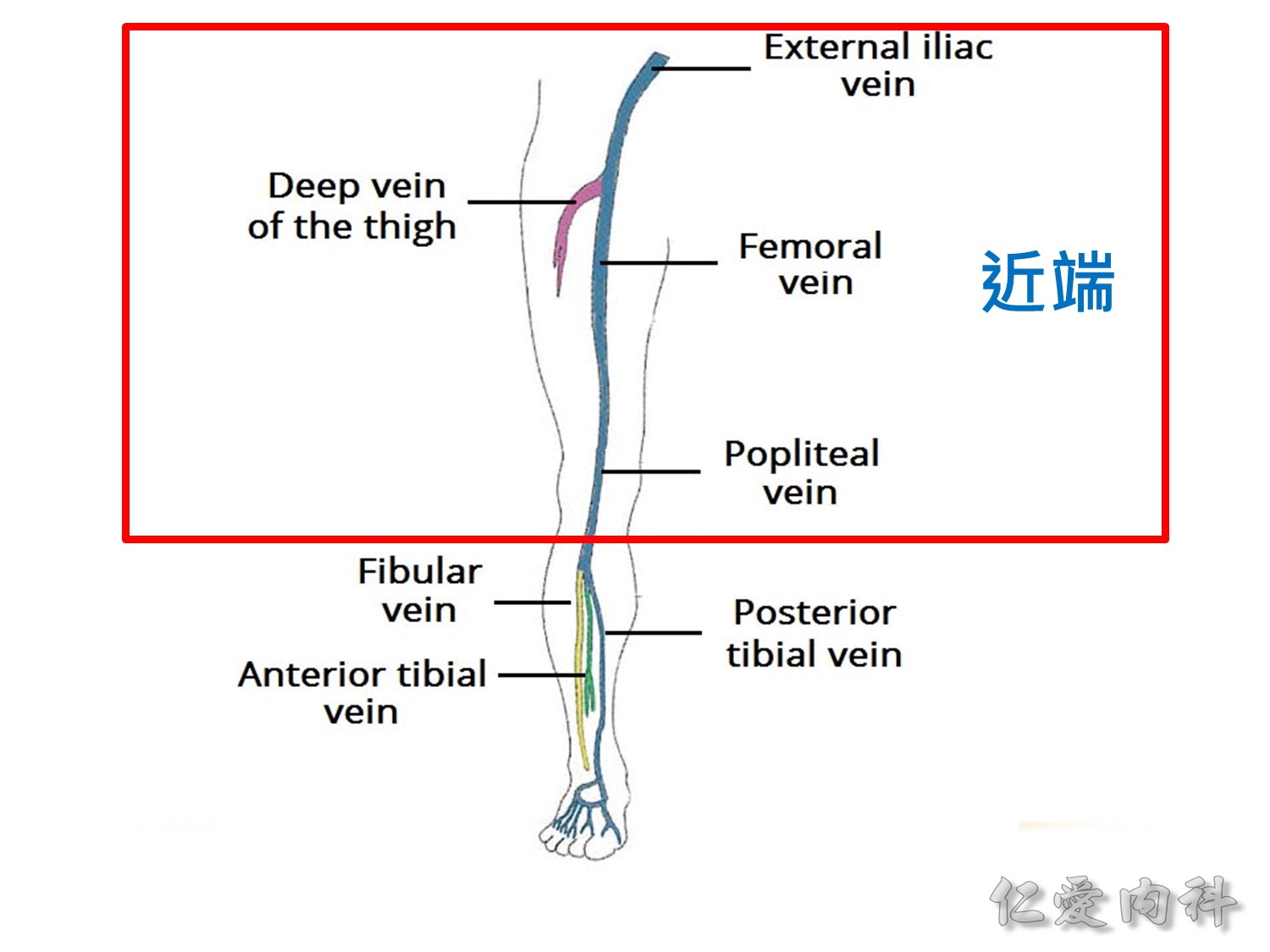
膝蓋以上就是近端
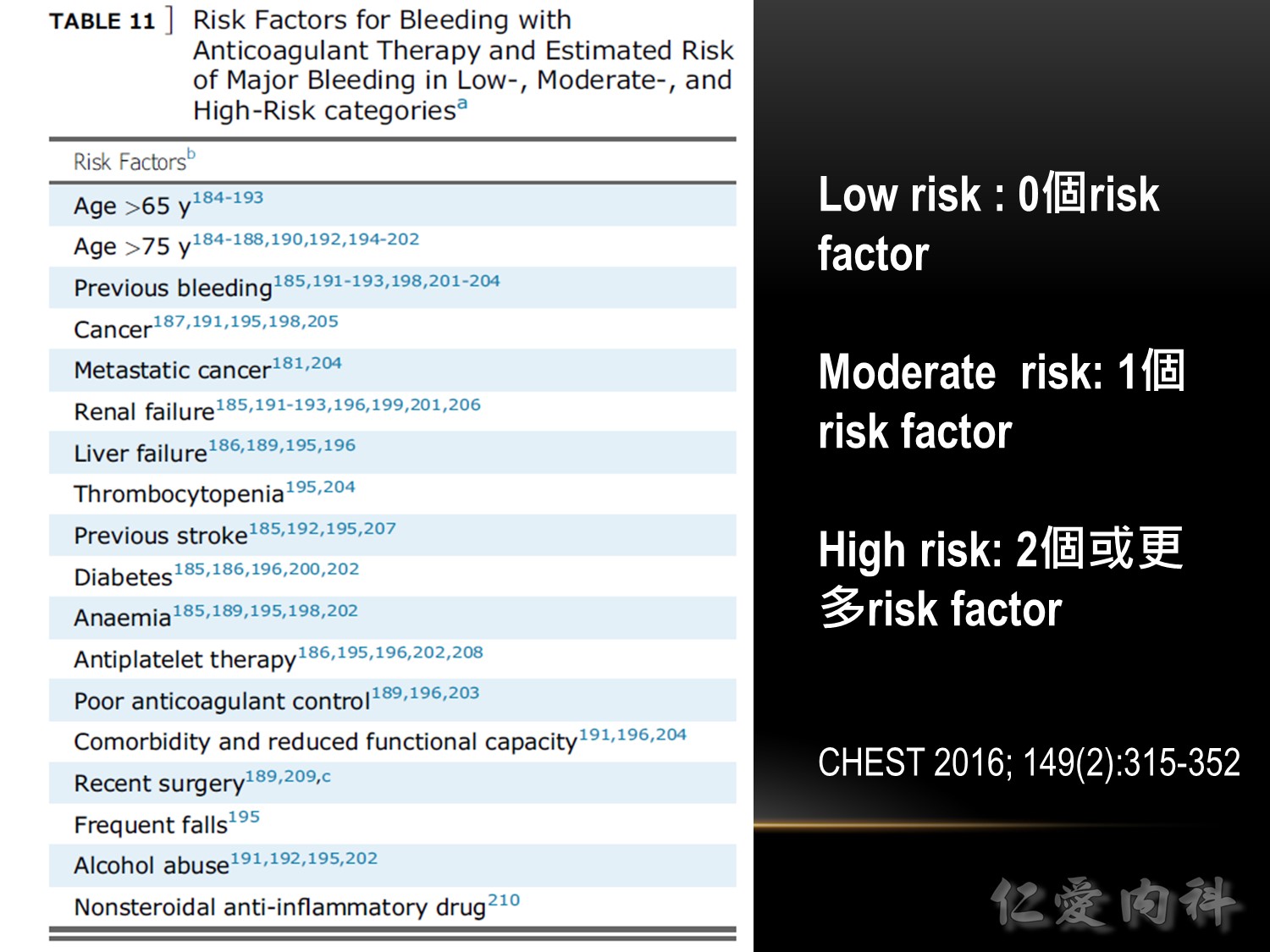
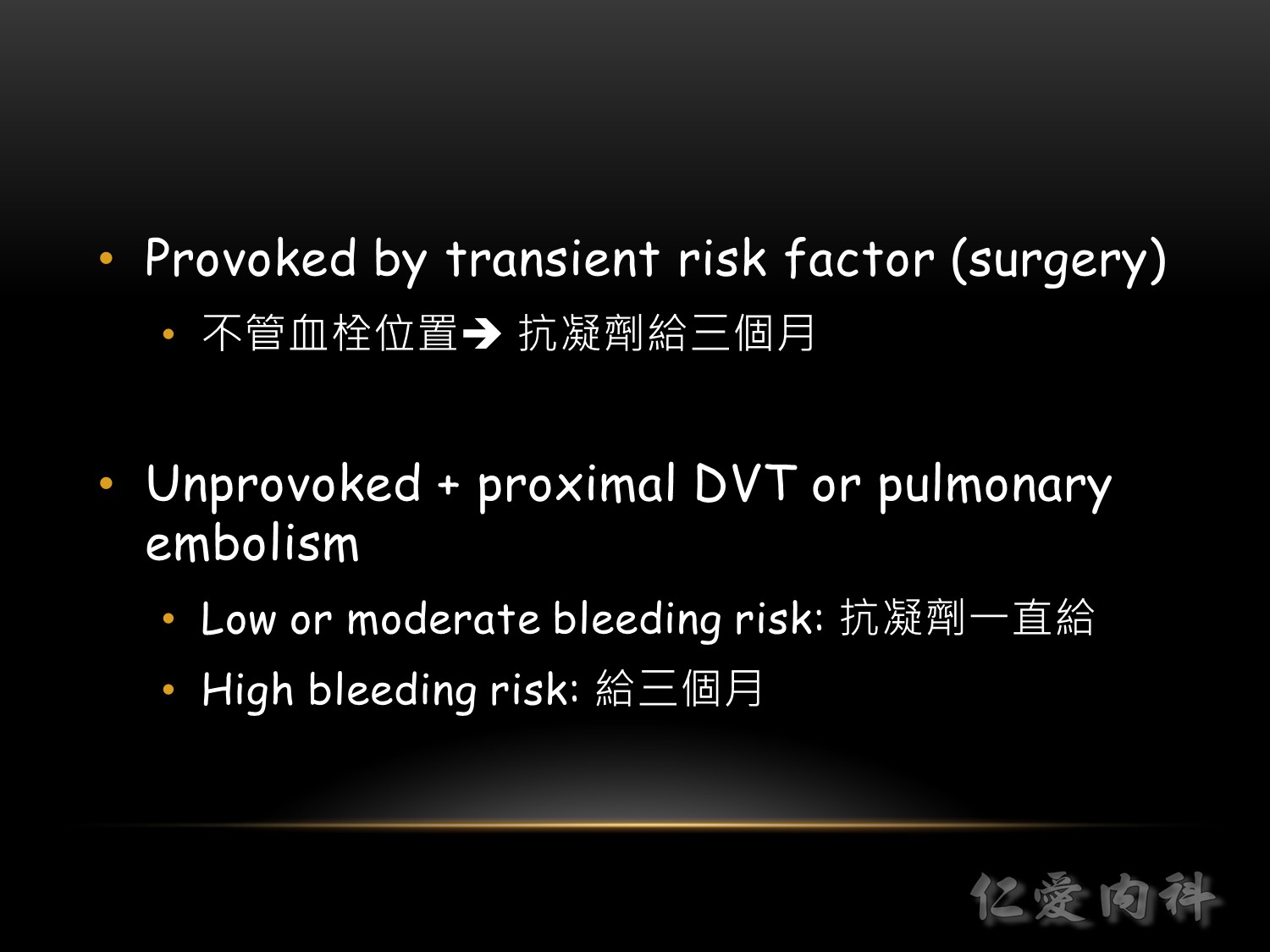
Based on this article:American College of Chest Physicians (ACCP) Guideline and Expert Panel Report on Antithrombotic Therapy for VTE Disease.



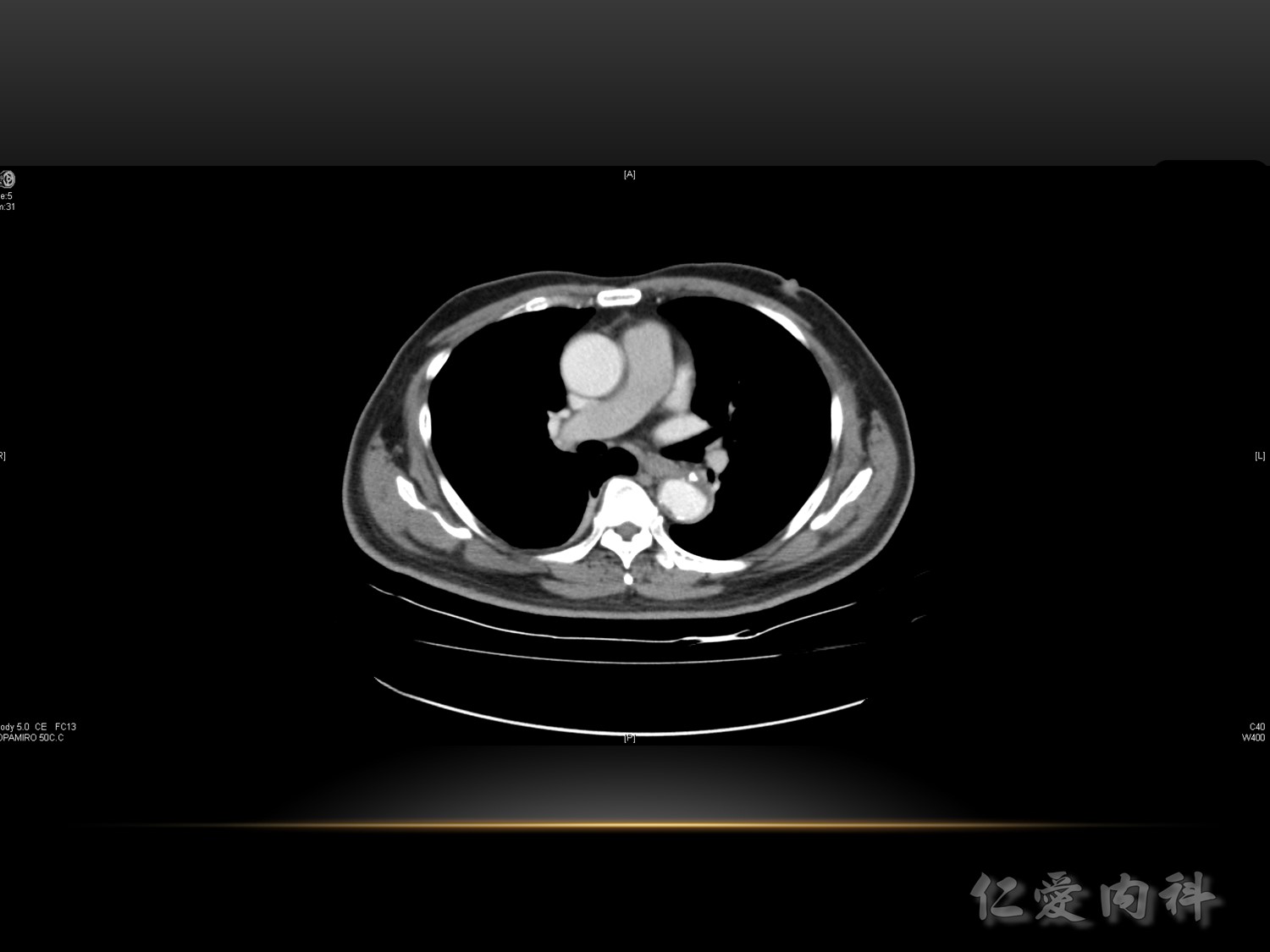
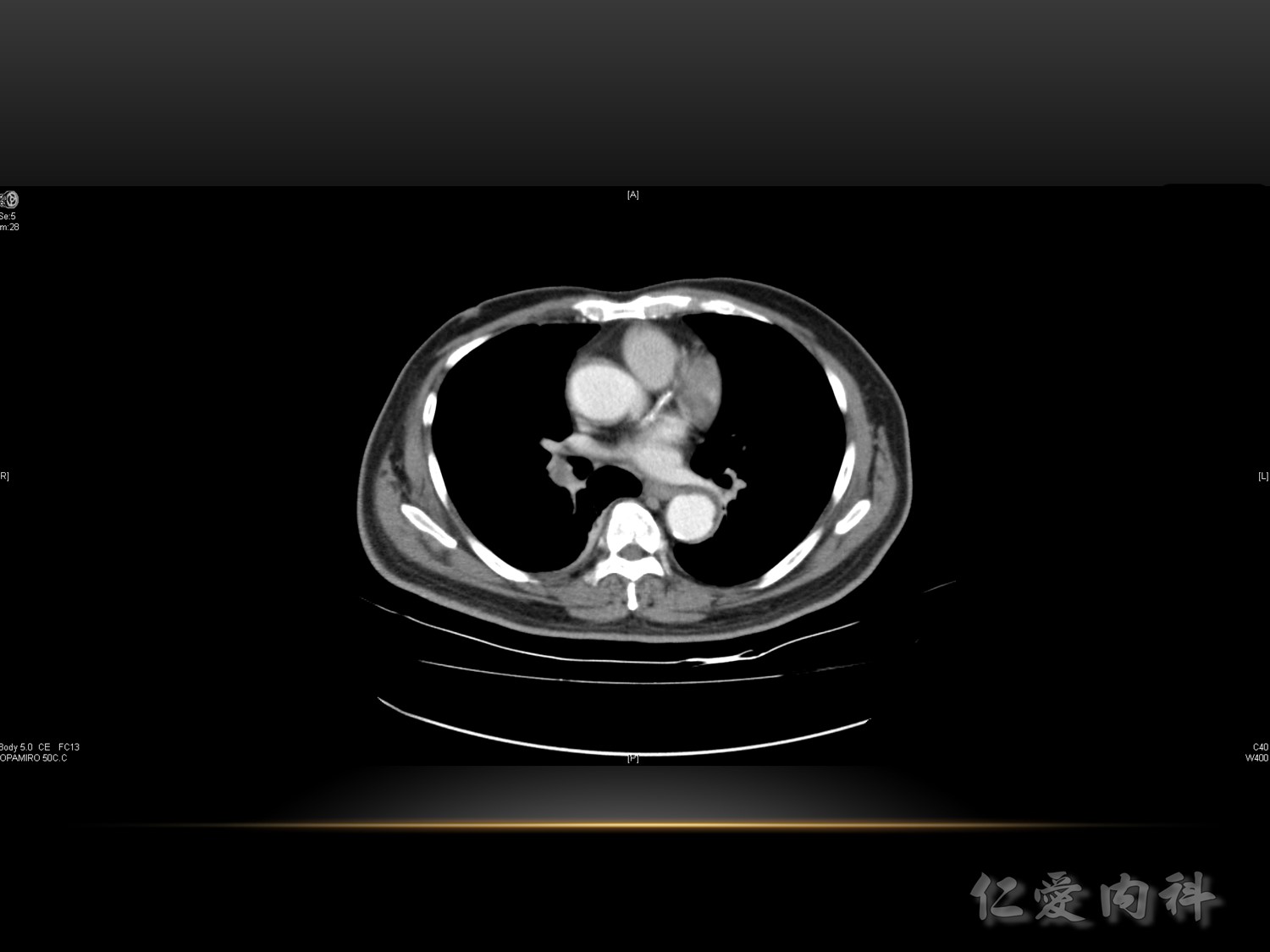
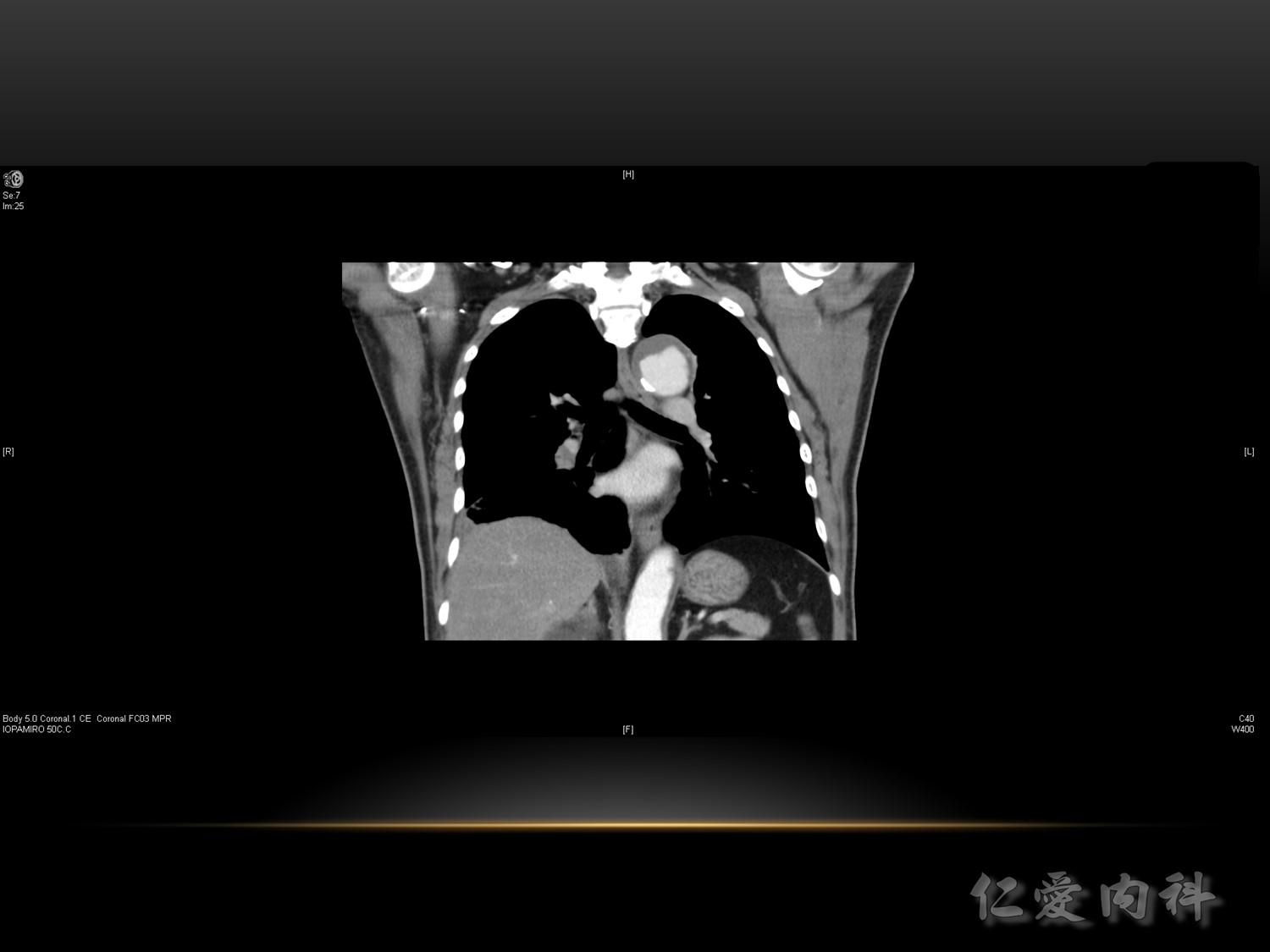
Step 0: confirm diagnosis
Step 1: stratify risk with Pulmonary Embolism Severity Index (PESI)
Step 3: offer PESI-based management

What then is the role of CDT in patients with PE?
We think that current evidence suggests that CDT is preferred to systemic thrombolytic therapy
1.in patients with acute PE who require active thrombus removal and
2.have risk factors for bleeding.
We suggest that venous puncture for CDT should always be ultrasound-guided and that the total dose of thrombolytic drug should be kept to a minimum in patients with a high risk of bleeding . If there is need for active thrombus removal in patients with a very high risk of bleeding, it may be necessary to use catheter-based therapy without thrombolytic drug or to use surgical embolectomy.
We are not ready to encourage use of CDT in preference to anticoagulation alone in stable patients with acute PE and right ventricular dysfunction.
Ref:JACC: Cardiovascular Interventions
Volume 8, Issue 10, August 2015DOI: 10.1016/j.jcin.2015.06.009 Catheter-Directed Thrombolysis for Pulmonary Embolism