作者/講者: Dr. Ian YC Chen
校稿: Dr. Ian YC Chen
上次校閱: 2018/03/27
This introduction is based on the relevant content in Murray and Nadel’s Textbook of Respiratory Medicine – (Sixth Edition)

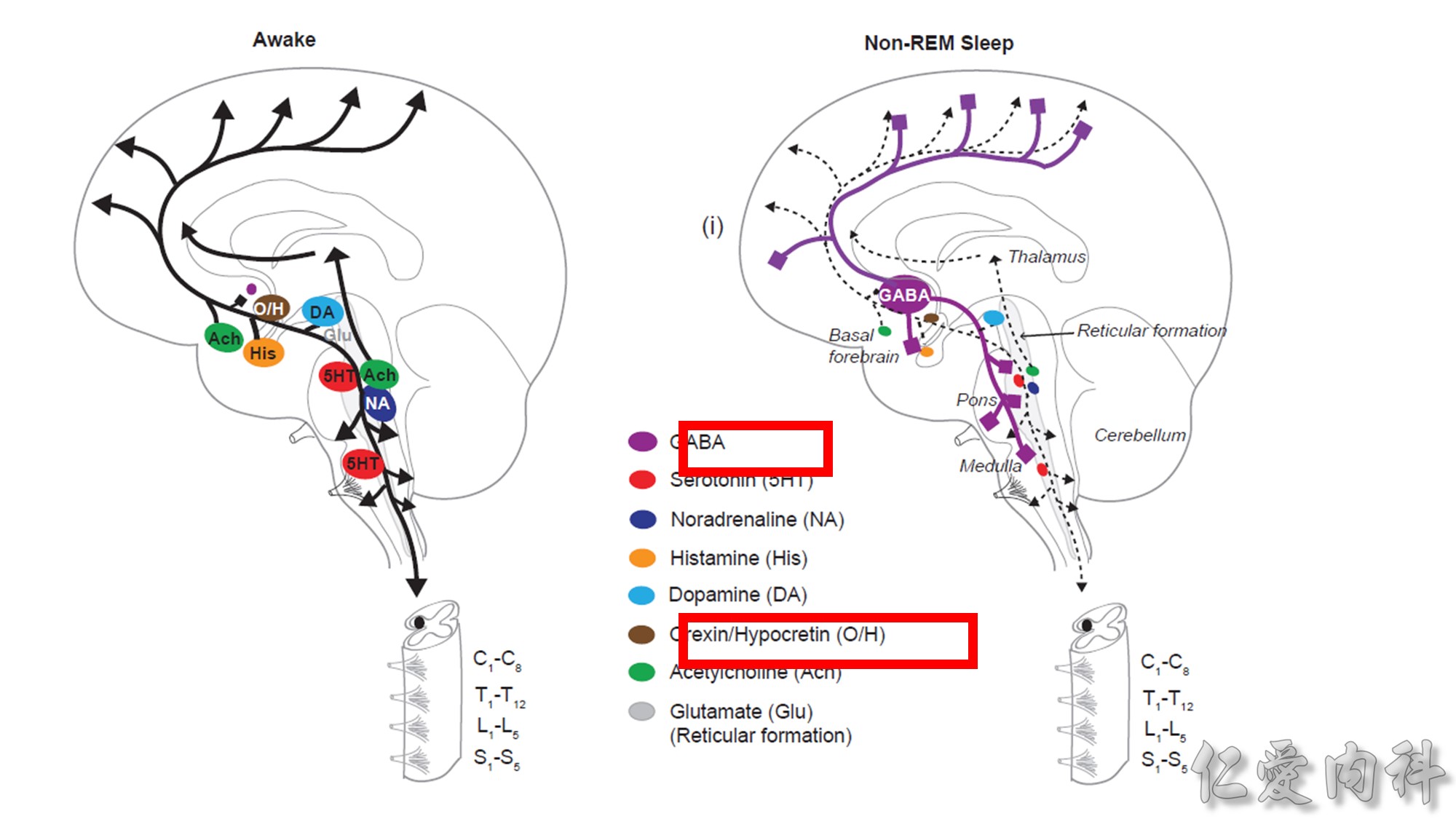
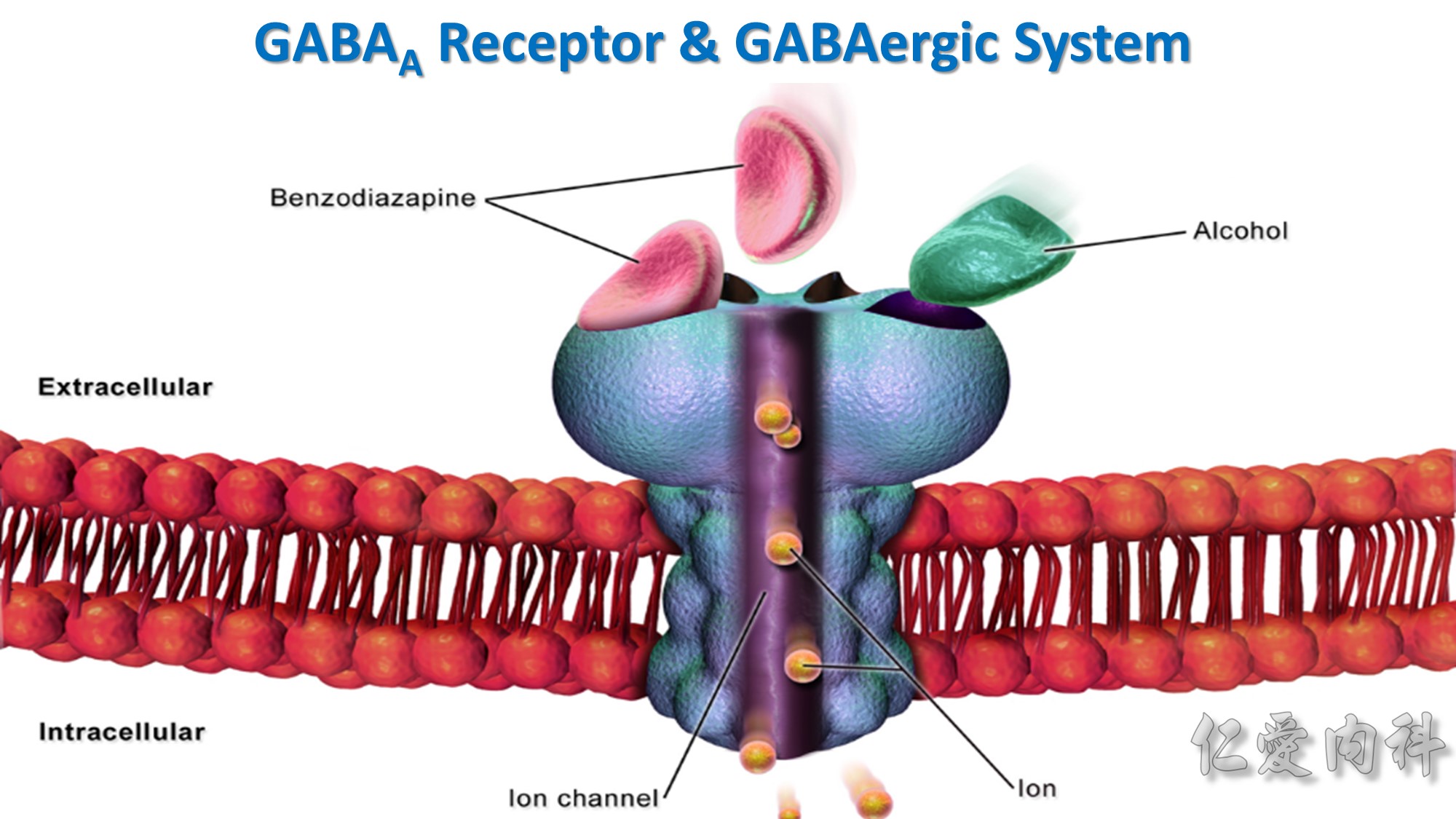
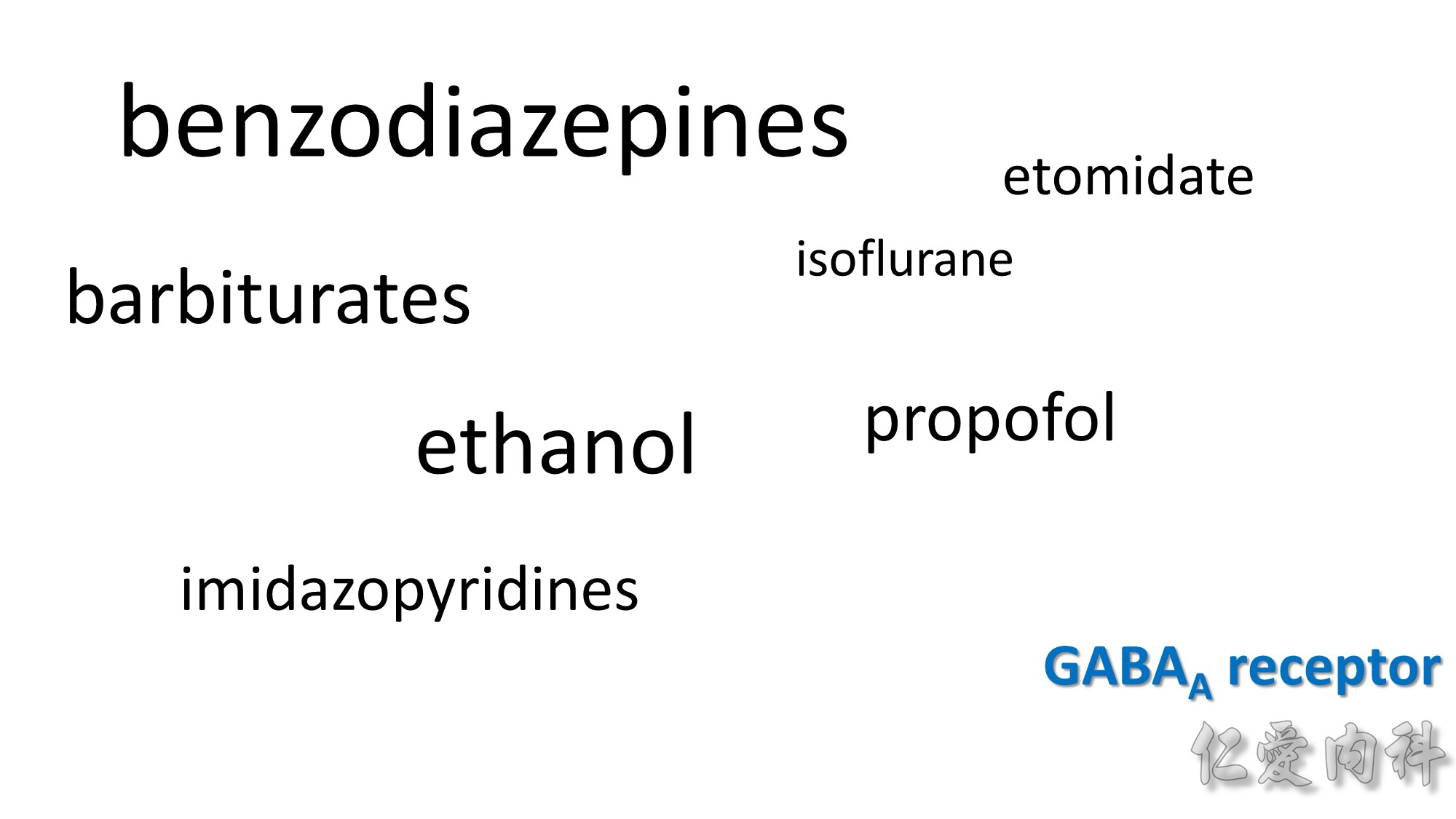
GABA: gamma-aminobutyric acid
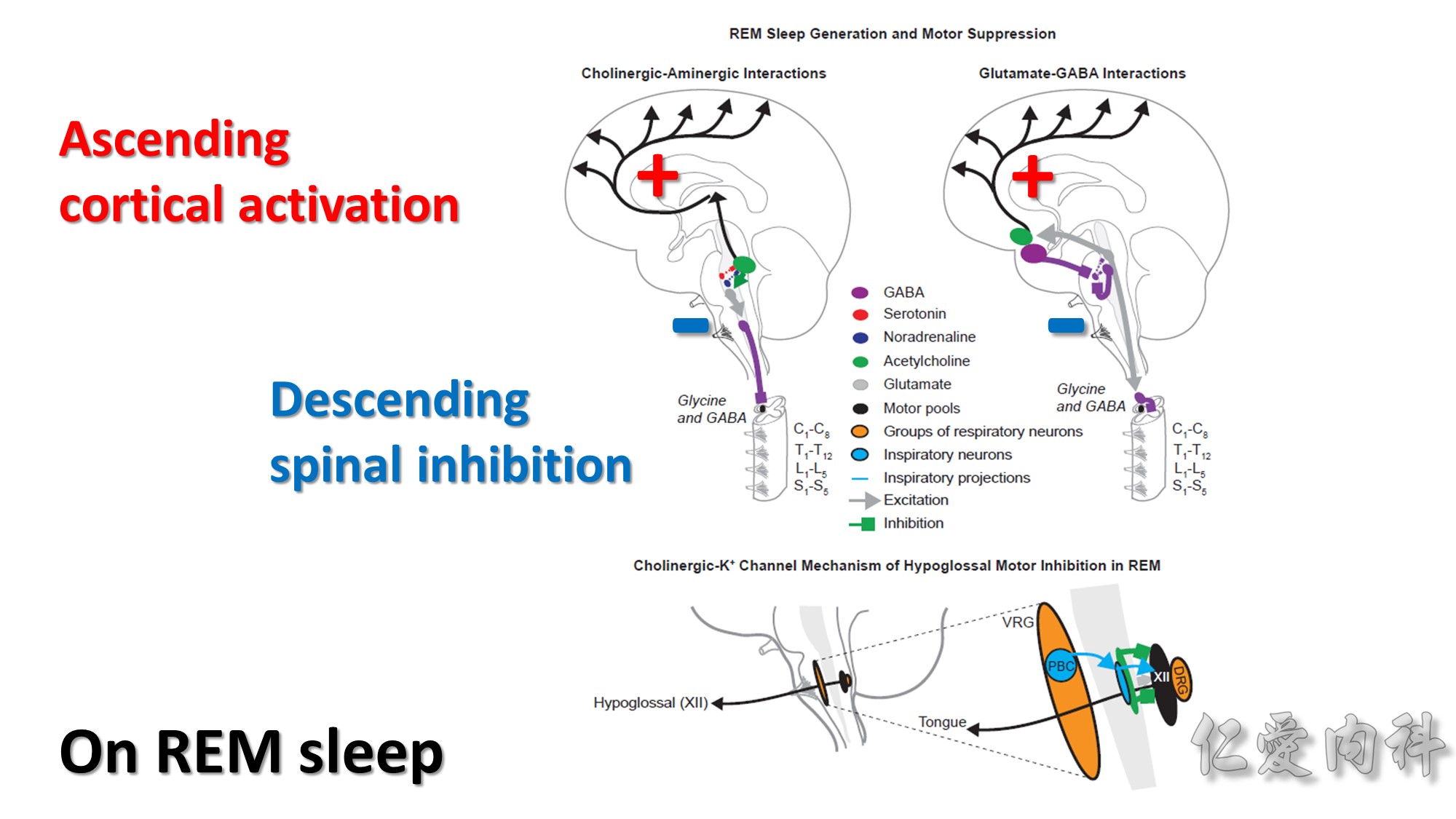
VRG: ventral respiratory group
DRG: dorsal respiratory group
PBC: pre-Bötzinger complex
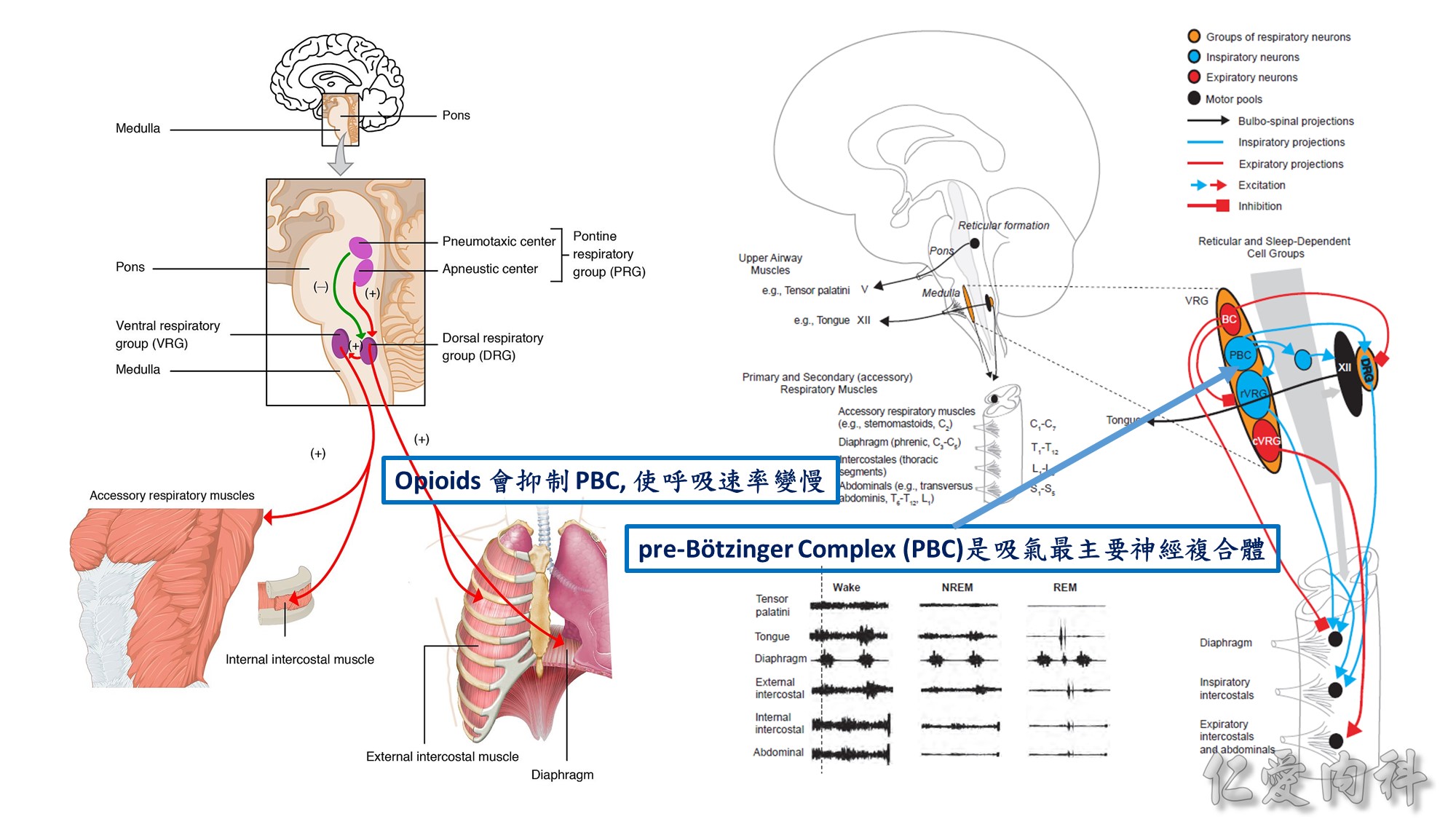
BC: Bötzinger Complex
PBC: pre-Bötzinger Complex
DRG: dorsal respiratory group
VRG: ventral respiratory group
cVRG: caudal VRG
rVRG: rostral VRG
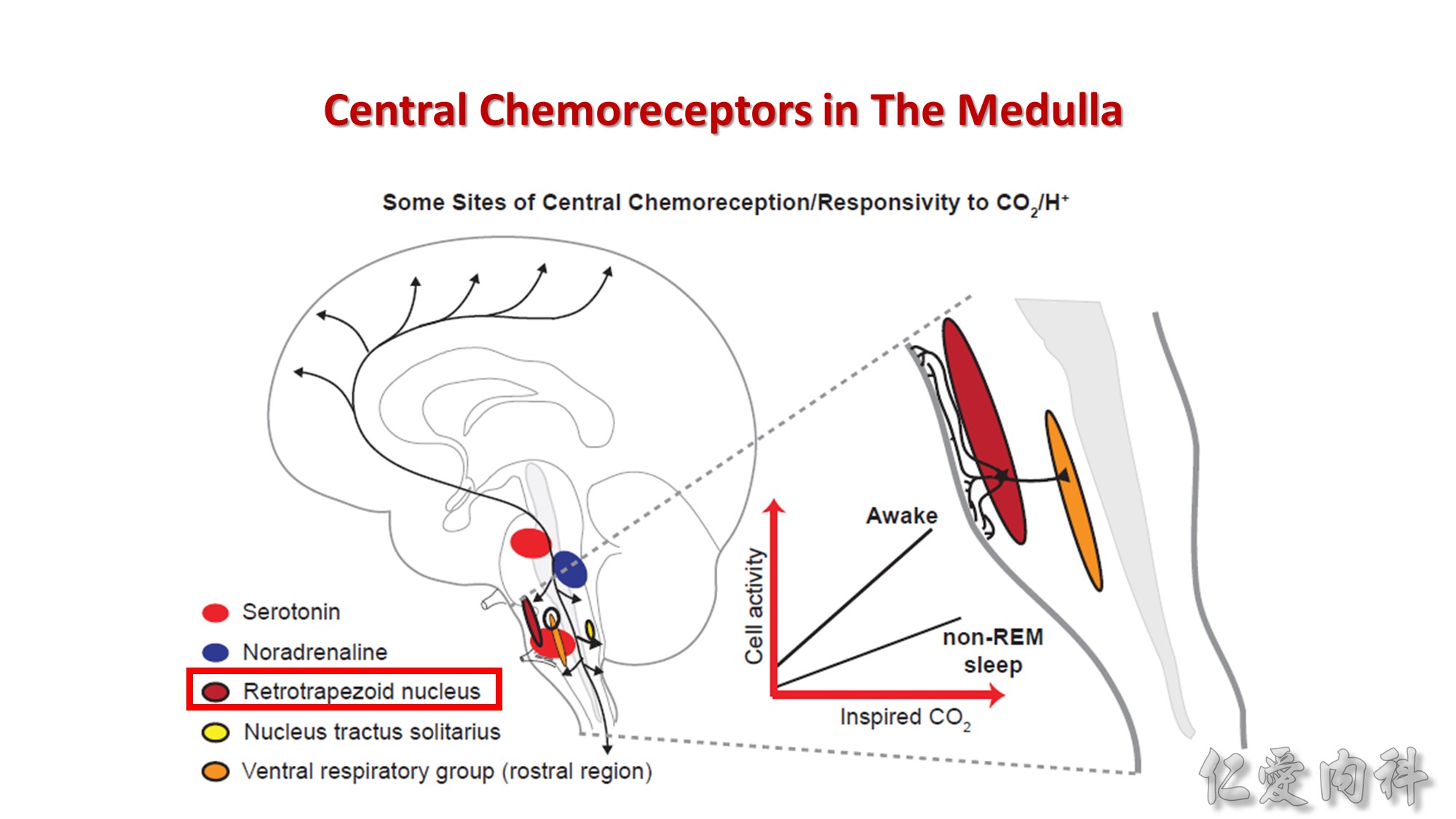
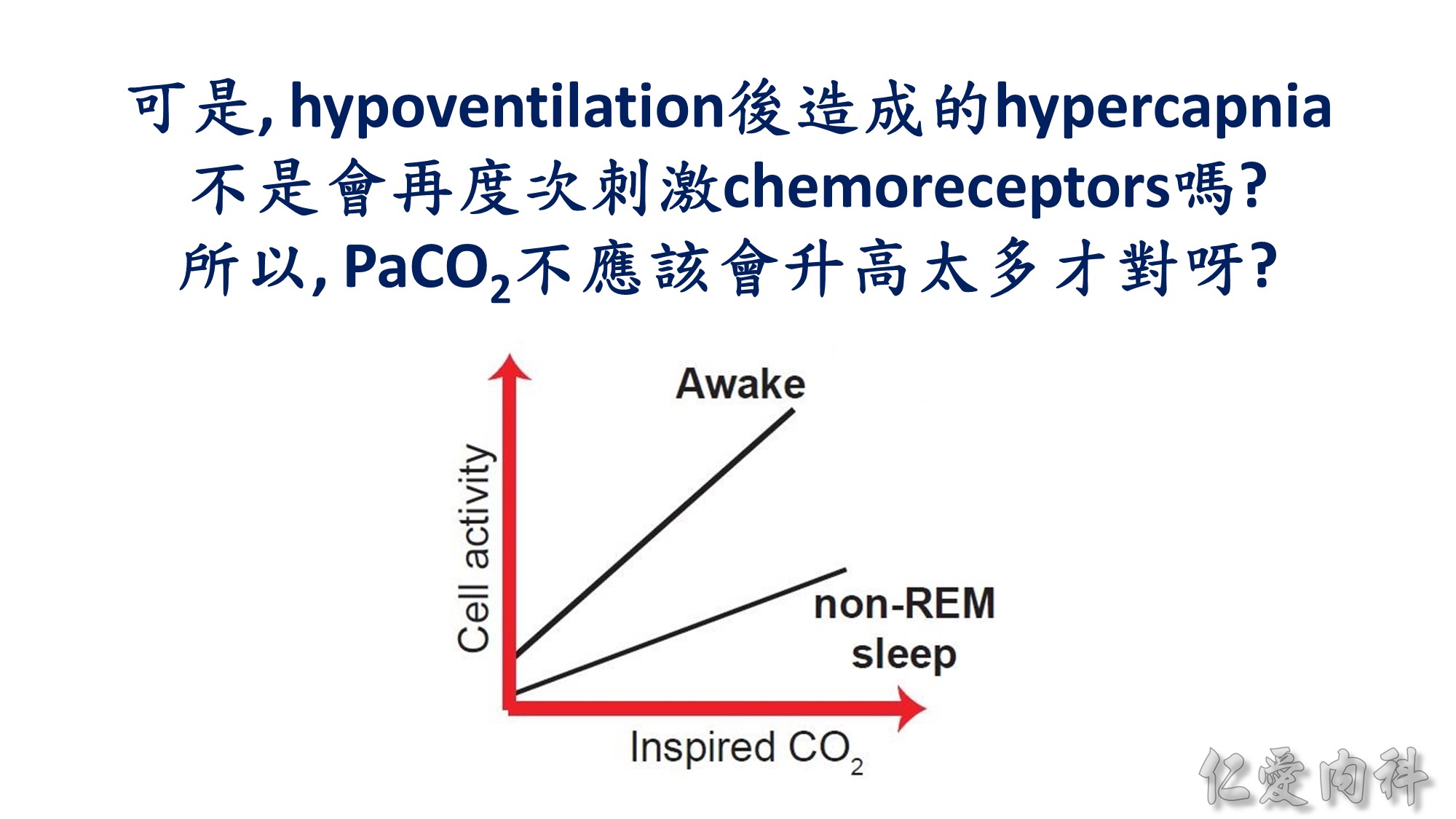
A key site that is intrinsically sensitive to alterations in CO2/H+ is the retrotrapezoid nucleus located near the ventral surface of the medulla. This region of the brain is magnified in the
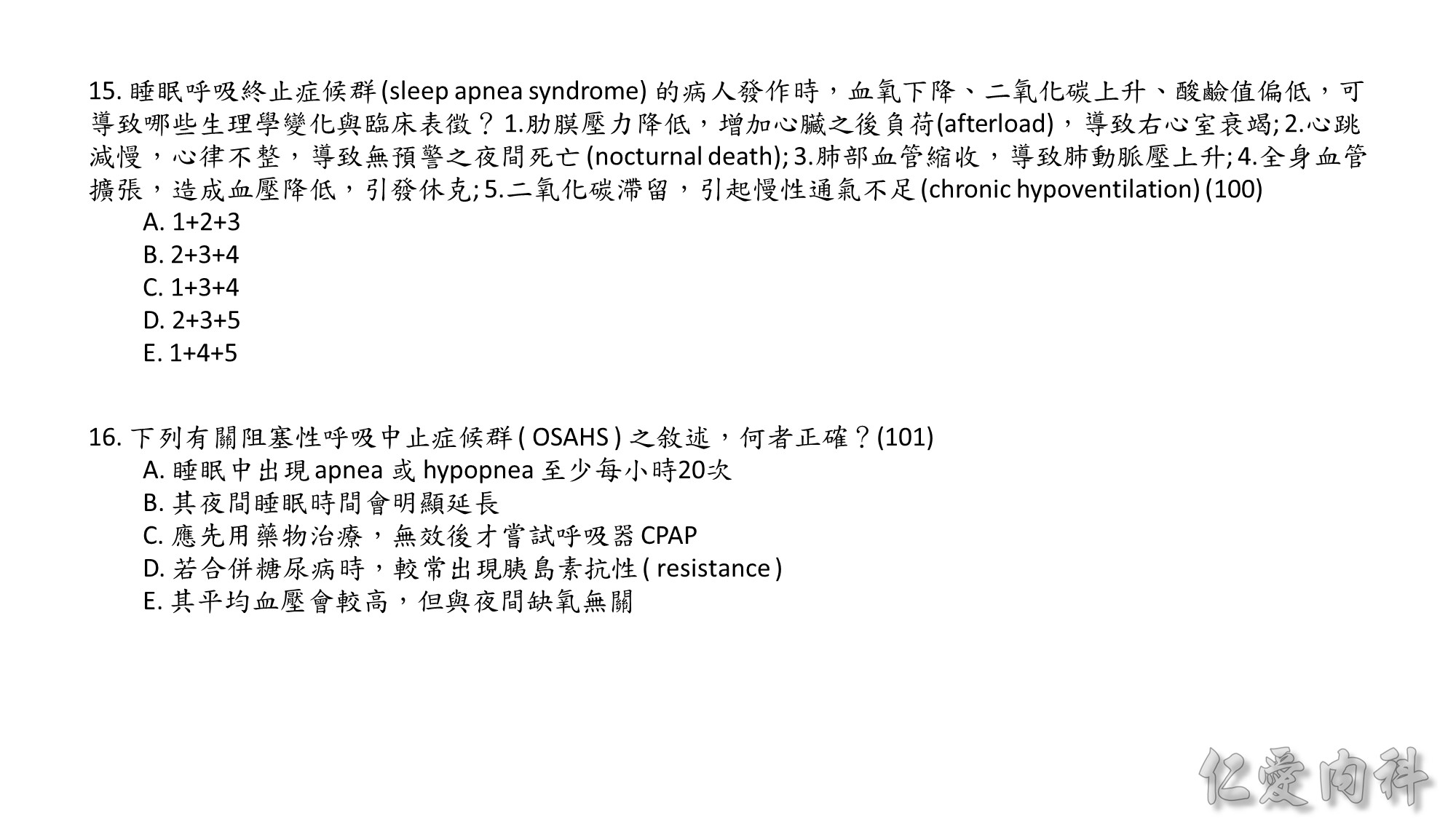
panel on the right. Branching dendrites from retrotrapezoid neurons “taste” the cerebrospinal fluid at the medullary surface and are activated by increased
CO2 (lowered H+). Activity related to CO2/H+ influences several brain regions, including the ventral respiratory group, so driving breathing. The inset shows
the response of a brain-stem serotonergic neuron to increases in inspired CO2. There are several features of note: (1) baseline activity (i.e., at zero inspired
CO2) is higher in wakefulness than in sleep, in keeping with Figure 85-1; (2) the neuronal activity at any given inspired CO2 is greater in wakefulness than
in sleep; (3) the slope (gain) of response is also greater in wakefulness than in sleep. Together, these three features parallel the overall respiratory responses
to CO2 as measured by changes in ventilation.
Note: in the bifurcation of the common carotid arteries located the peripheral chemoreceptors.

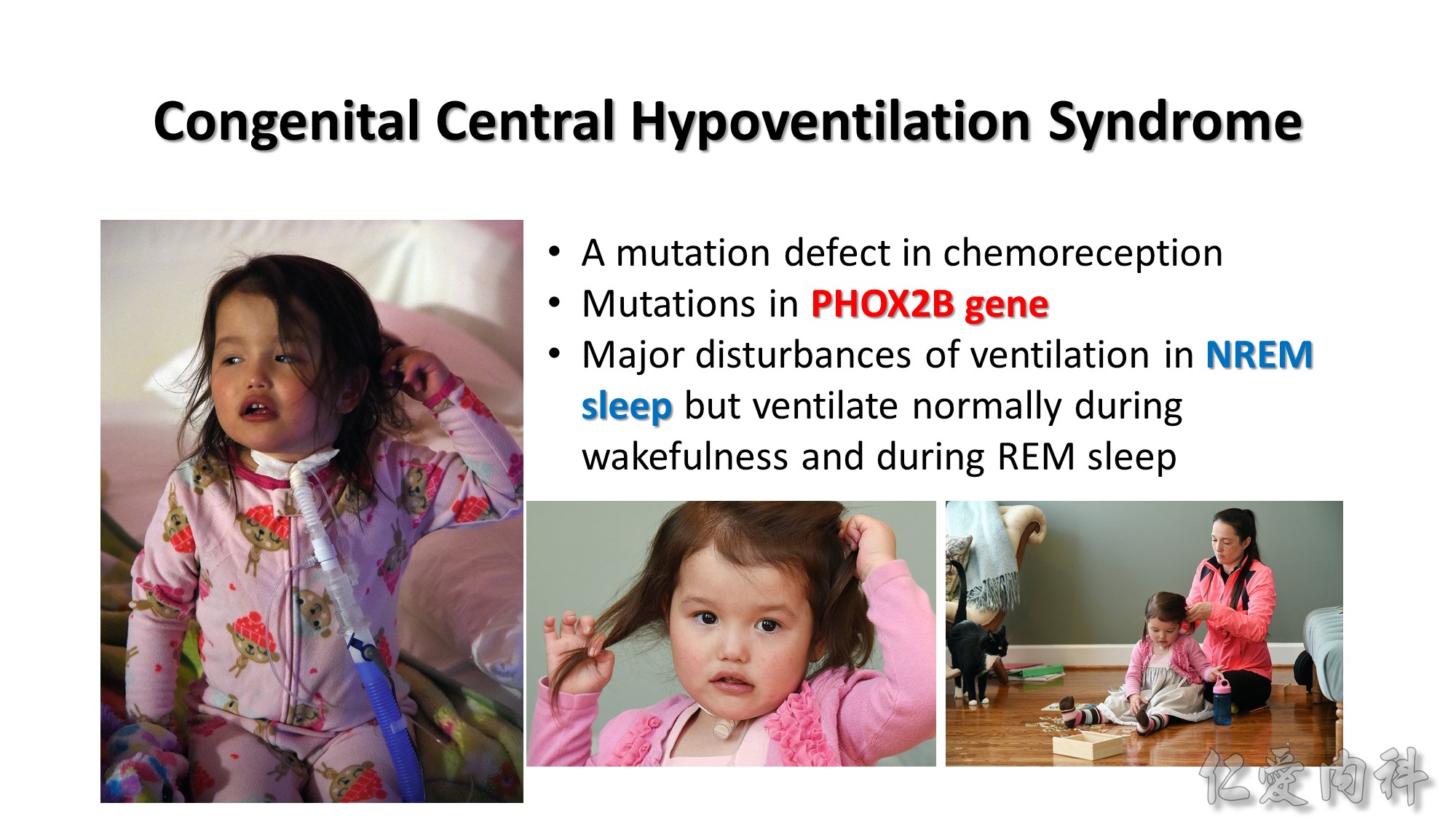
PHOX2B: paired-like homeobox 2b
http://www.al.com/news/index.ssf/2015/02/living_with_a_nightmare_local.html
(Accessed on 2018/02/13)
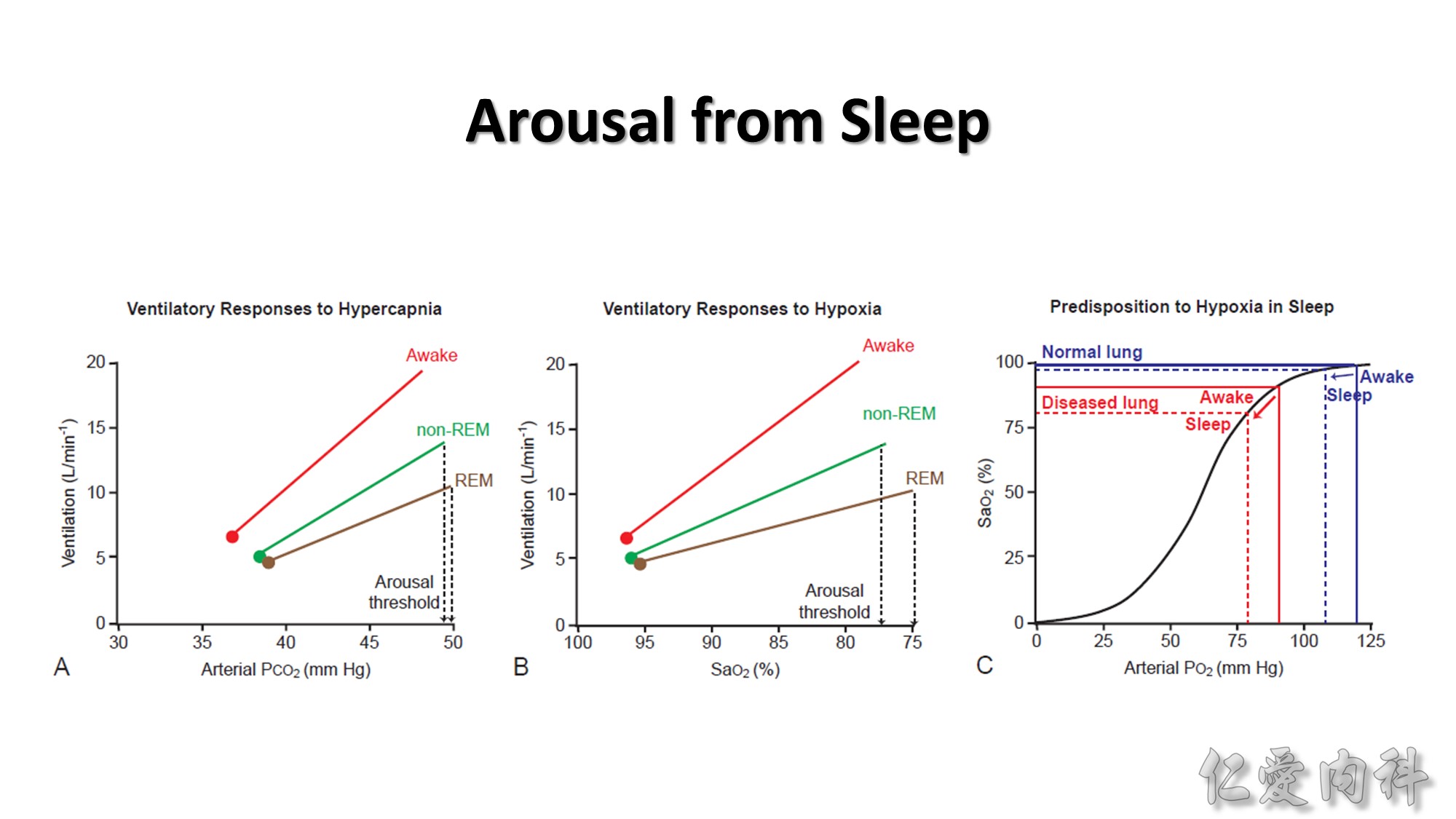
Summary graphs showing the ventilatory and arousal responses to hypercapnia (A) and hypoxia (B).
Note: (1) The decrease in basal ventilation from wakefulness (red) to non-REM (green) and REM (brown) sleep; (2) ventilation is greater in wakefulness at any given elevated arterial CO2 or lowered arterial oxygen saturation (SaO2) compared to non-REM sleep and REM sleep; (3) the slope (gain) of the ventilatory responses to hypercapnia and hypoxia is also greater in wakefulness than in non-REM sleep and is most depressed in REM sleep. Also shown are the thresholds for hypercapnia (A) and asphyxia hypoxia (B) to elicit arousal from sleep. The figure also illustrates the relationship between the starting (waking) arterial partial pressure of O2 and the magnitude of the decrease in SaO2 from wakefulness to sleep (C). Normal decreases in ventilation from wakefulness to sleep lead to normal decreases in arterial PO2 but only modest or trivial decrease in SaO2 in sleep, because the starting arterial PO2 is on the flat portion of the oxyhemoglobin dissociation curve (blue lines, C). Such a situation, for example, typically would be experienced by individuals living at sea level, or in individuals with healthy lungs and/or with normal ventilation and lung perfusion. The same magnitude of decrease in ventilation and arterial PO2 from wakefulness to sleep, however, can lead to a large decrease in SaO2 if an individual is initially hypoxic and therefore initially positioned on the steep portion of the dissociation curve (starting SaO2 of about 90%).
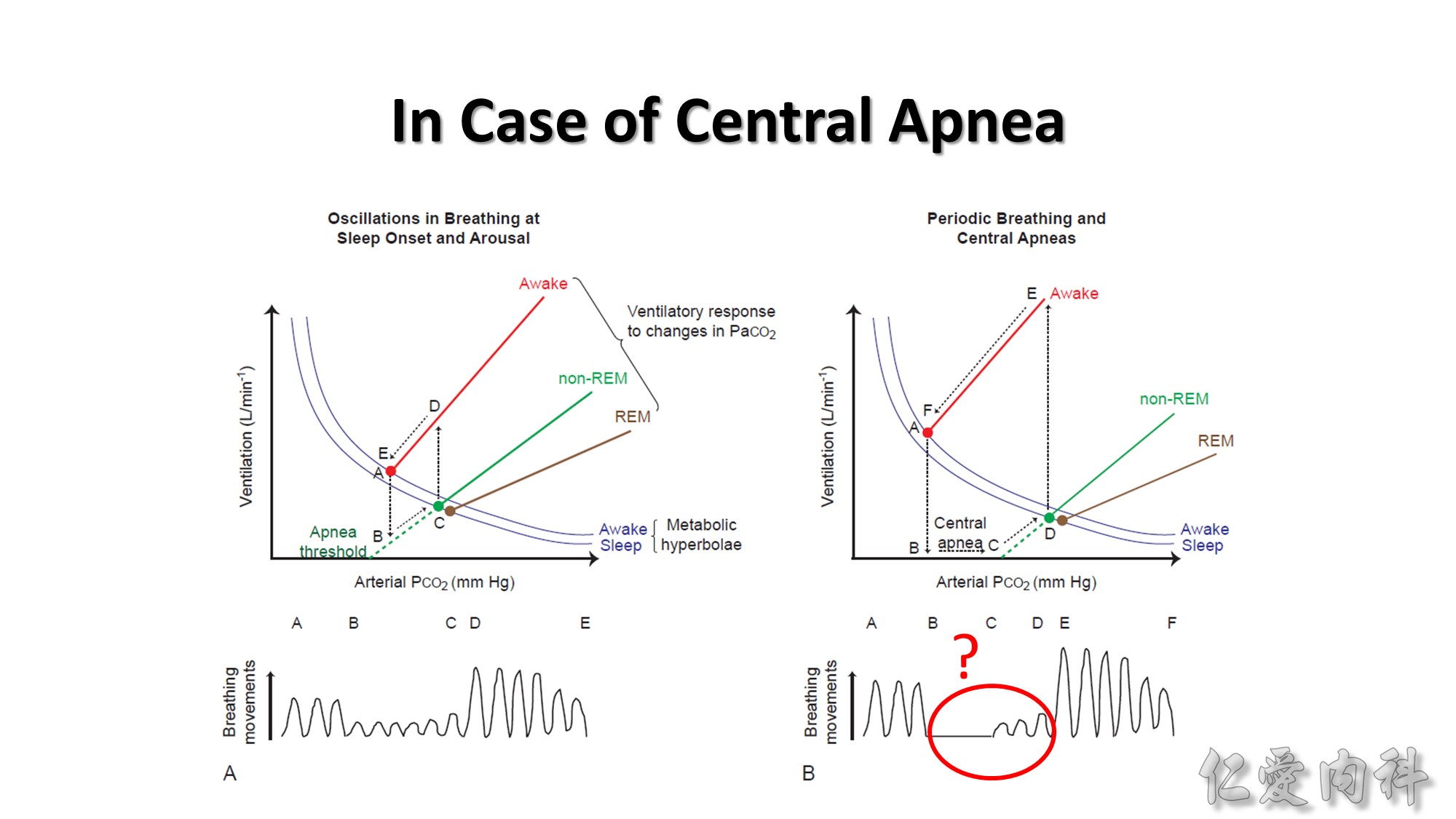
Schema to illustrate how interactions between the ventilatory responses to hypercapnia and transitions between sleep and wakefulness can provoke unstable breathing and central apneas. The equilibrium point for stable breathing in wakefulness is illustrated by point A (red) in the left graph. This equilibrium point intersects the ventilatory response to increased arterial PCO2 (red line) and the change in arterial PCO2 that results from a change in ventilation (the metabolic hyperbola, blue line). The ventilatory response to increased arterial PCO2 in non-REM and REM sleep are also shown (green and brown lines, respectively). Also shown is how a decrease in arterial PCO2 in non-REM sleep can result in reduced ventilation and eventually apnea (dashed green line). At sleep onset, the arterial PCO2 that was previously present in wakefulness (point A) produces lesser ventilation in sleep according to the extrapolation of the ventilatory response to CO2 in sleep (dashed green line, point B). This decrease in ventilation is out of proportion to metabolic rate so ventilation progressively increases toward the new sleeping equilibrium position (point C, green). If the patient arouses from sleep, then the arterial PCO2 that represents the equilibrium point for breathing in sleep (green) now represents a hypercapnic stimulus according to the ventilatory response to CO2 in wakefulness, such that ventilation increases dramatically (points C to D). The elevated level of ventilation at point D is out of proportion to the prevailing metabolic rate so ventilation progressively decreases toward the waking equilibrium position (points D to E, red). The cycle of waxing and waning of ventilation with the waxing and waning of wakefulness and sleep continues until sleep is established. The physiologic principle that arises from this effect is that any separation of equilibrium points in wakefulness and non-REM sleep (red and green), for any reason can lead to periodic breathing and central apneas at sleep onset. Such periodicity and central apnea is shown in the right graph.
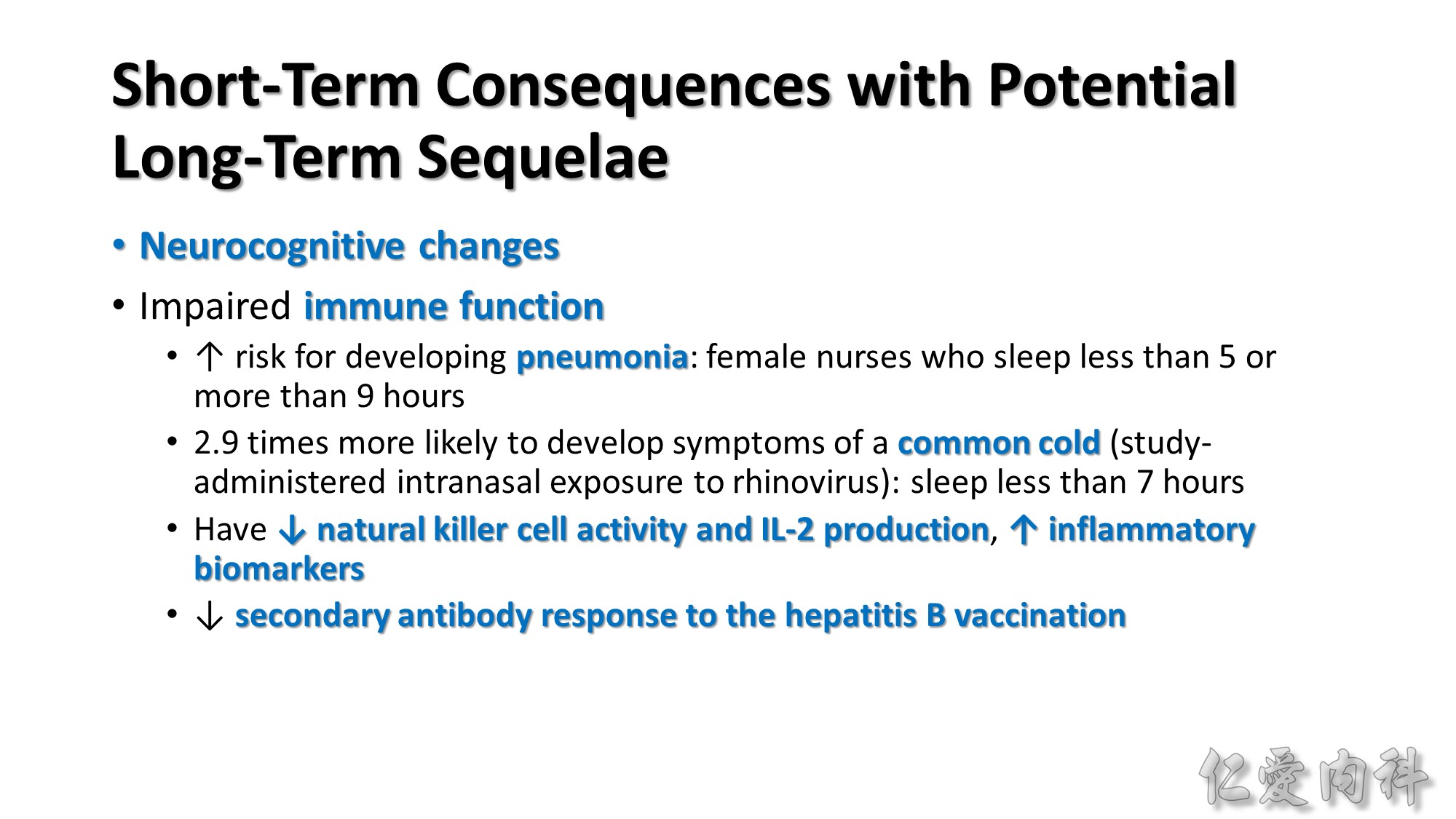
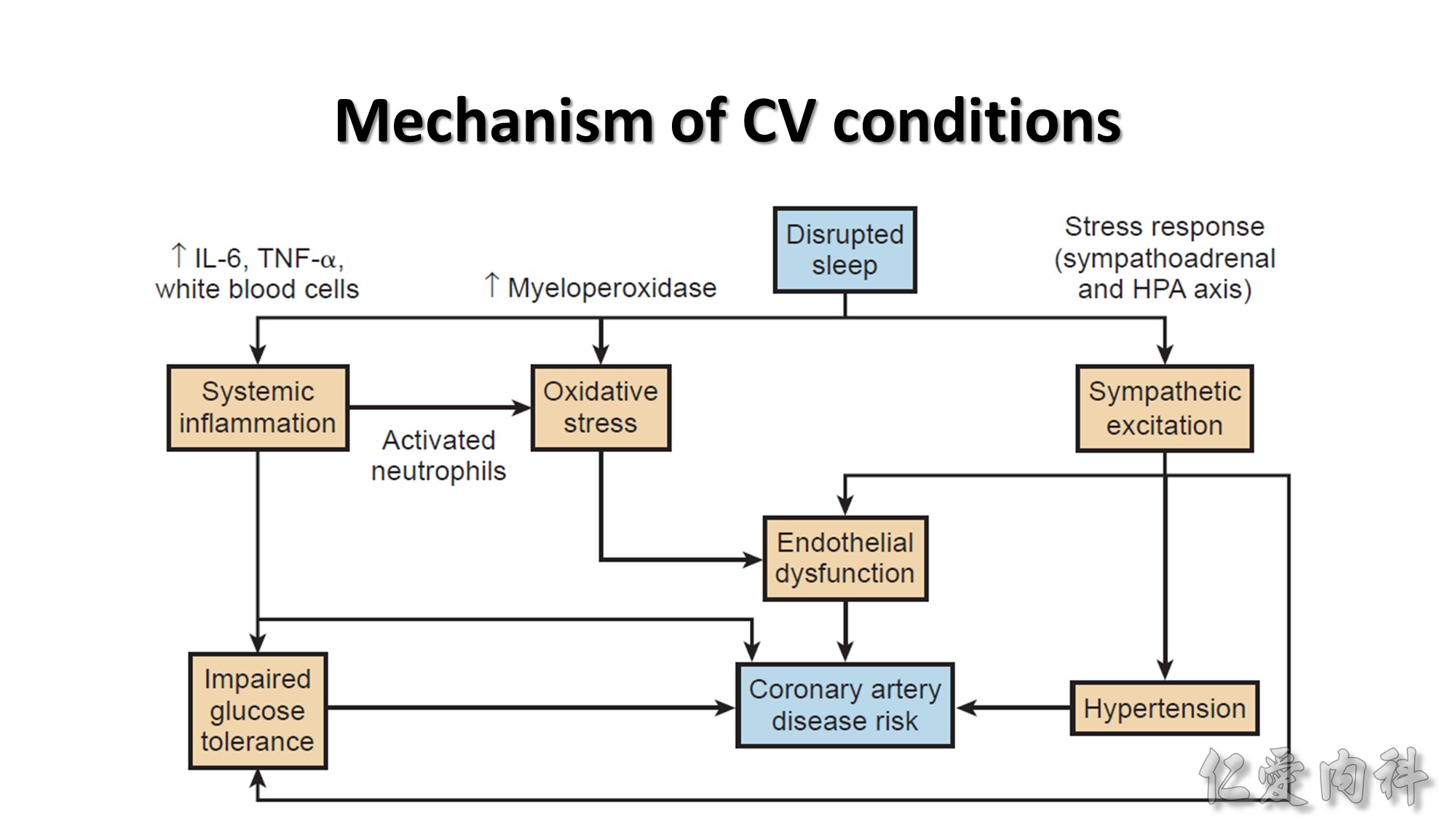
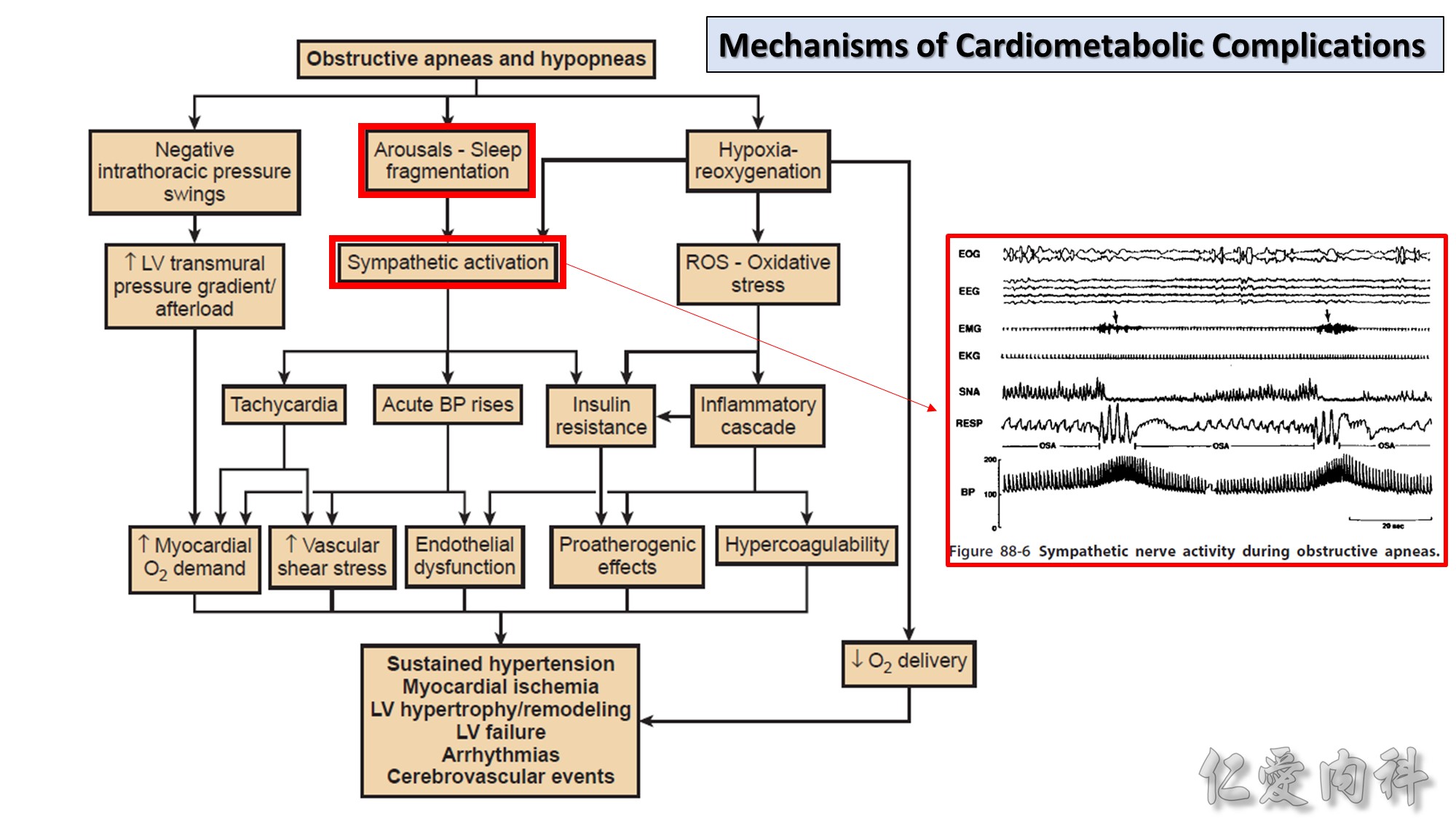
Systemic Inflammation
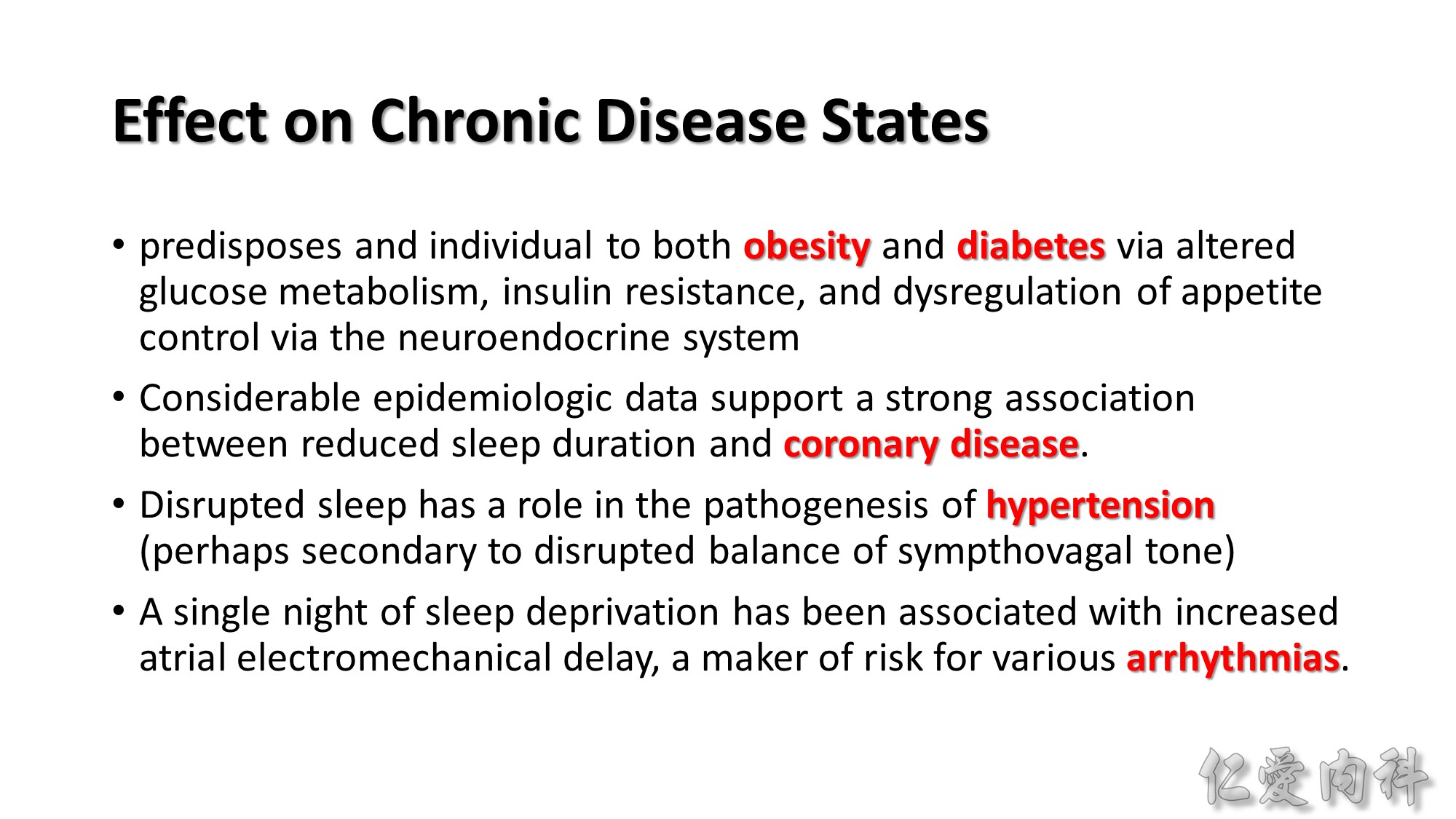
1.Sleep reduction to 6 hours/night is associated with an increase in secretion of the proinflammatory cytokines IL-6 and tumor necrosis factor (TNF)-α.
2.Elevation of IL-6 and TNF-α have been noted in disease states associated with systemic inflammation, including insulin resistance and cardiovascular disease.
3.CRP is synthesized in the liver predominantly by IL-6 activation.
Oxidative Stress
1.Periods of chronic sleep deprivation and recovery may lead to cardiovascular disease via leukocyte-mediated elevations of proatherogenic oxidative biomarkers (e.g., myeloperoxidase).
Dysautonomia
1.Activation of the neuroendocrine stress response and an overall increase in sympathetic tone.
2.The two primary systems involved with the neuroendocrine stress response in humans and other organisms are the sympathoadrenal system and the hypothalamic-pituitary-adrenal axis.
3.Onset of sleep has been associated with a rapid decrease in plasma levels of epinephrine and norepinephrine as a result of decreased sympathetic output in humans and rodents.
4.There is a shift to a dominant state of parasympathetic tone compared with sympathetic tone in the heart during normal circadian sleep. The phenomenon of “nocturnal dipping” is at least in part related to decreased sympathetic output during sleep.
5.Glucocorticoid release follows a circadian pattern as directed by the suprachiasmatic nucleus of the hypothalamus. More particularly, glucocorticoid levels decrease after the onset of sleep and peak just before the end of sleep.
Endothelial Dysfunction
1.The increase in reactive oxygen species leads to increased expression of adhesion molecules that activate leukocytes.
2.Studies of sleep apnea patients have demonstrated a relationship with markers of endothelial dysfunction including circulating levels of the adhesion molecules intercellular adhesion molecule-1 and L-selectin.
3.Increased vascular endothelial growth factor (VEGF) lead to abnormal vasodilatory responses, predisposing to hypertension and cardiovascular disease.
4.In a recent systematic review, OSA was found to be an independent predictor of subclinical cardiovascular disease, as assessed by measures such as coronary artery calcification and brachial artery flow-mediated dilation.



Pulse transit time: the time from the onset of the electrocardiographic QRS complex to the pulse wave in the finger

OSA Severity: respiratory disturbance index (apneas + hypopneas + RERAs) 少人用? 研究不夠? 不好用?
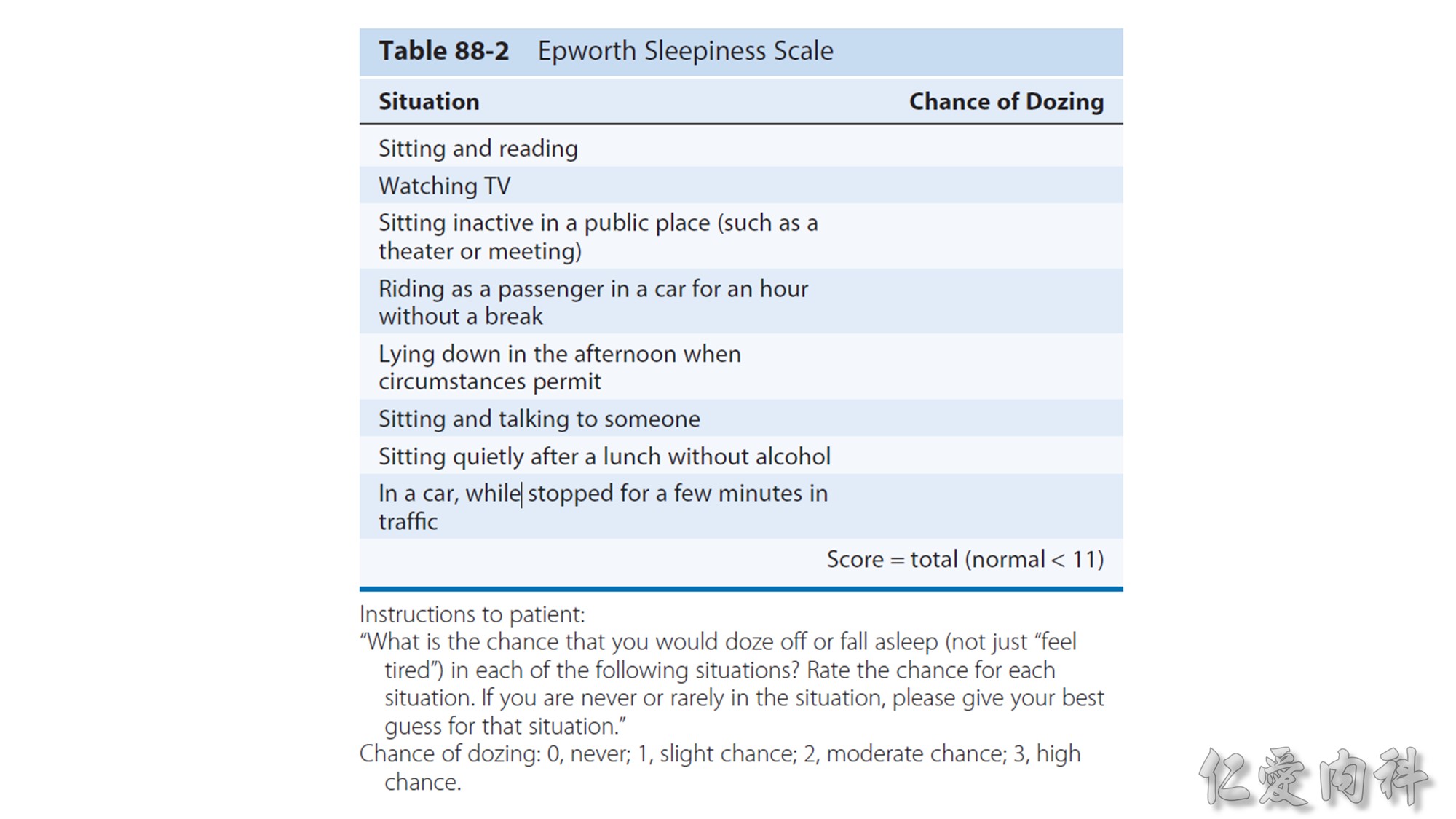
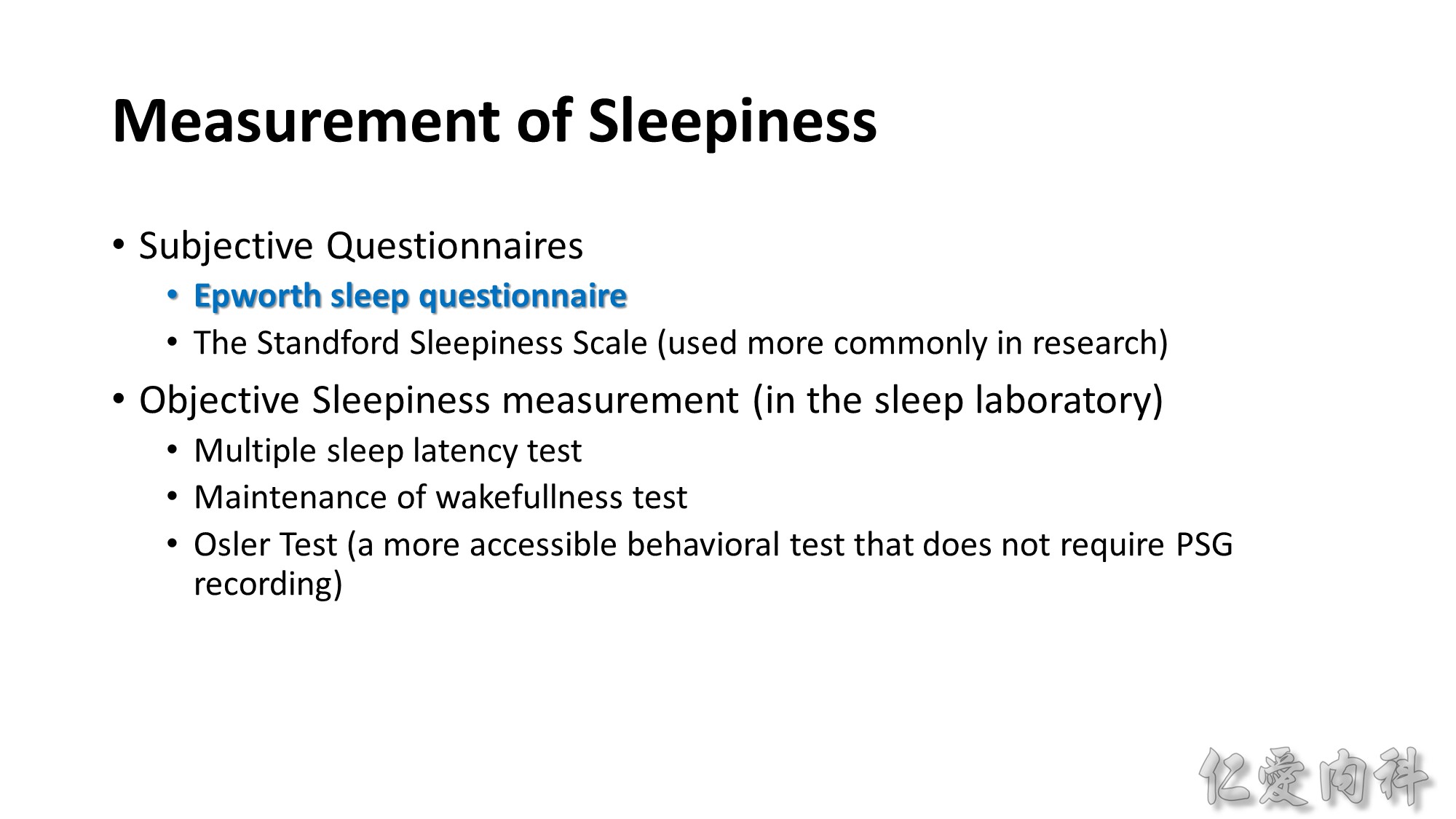
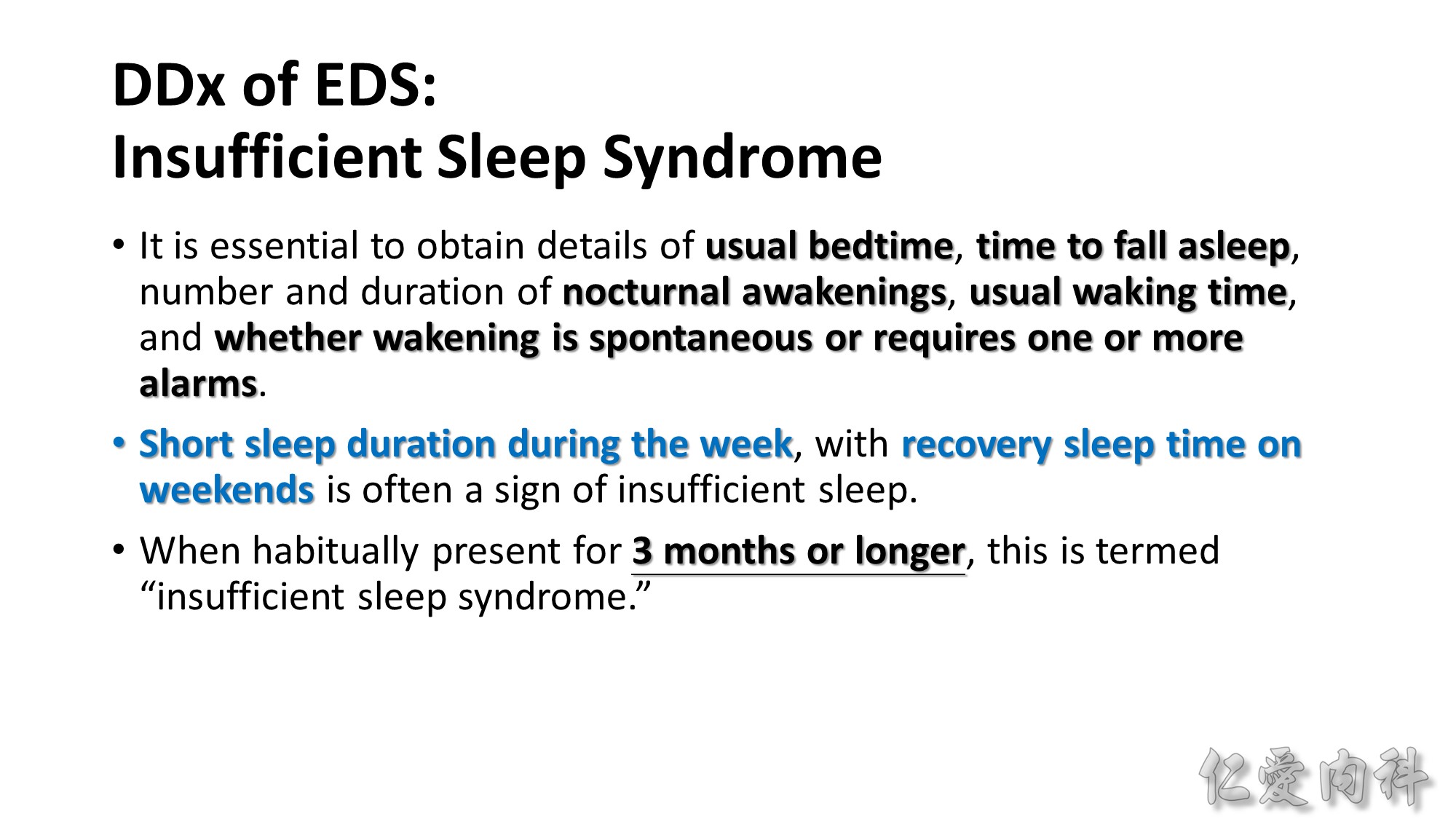
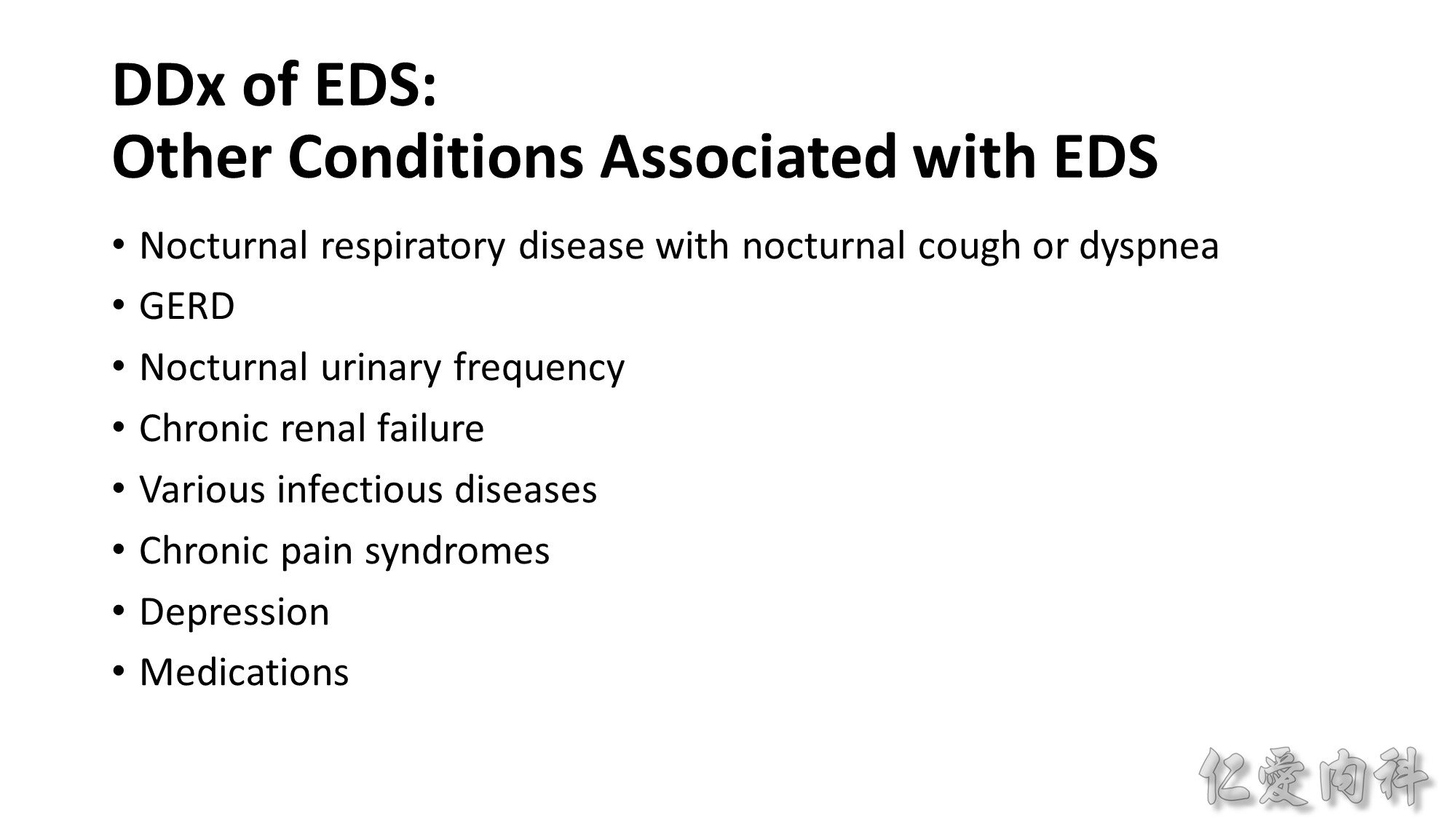
EDS is defined as a propensity to fall asleep in unwanted situations during normal waking hours.
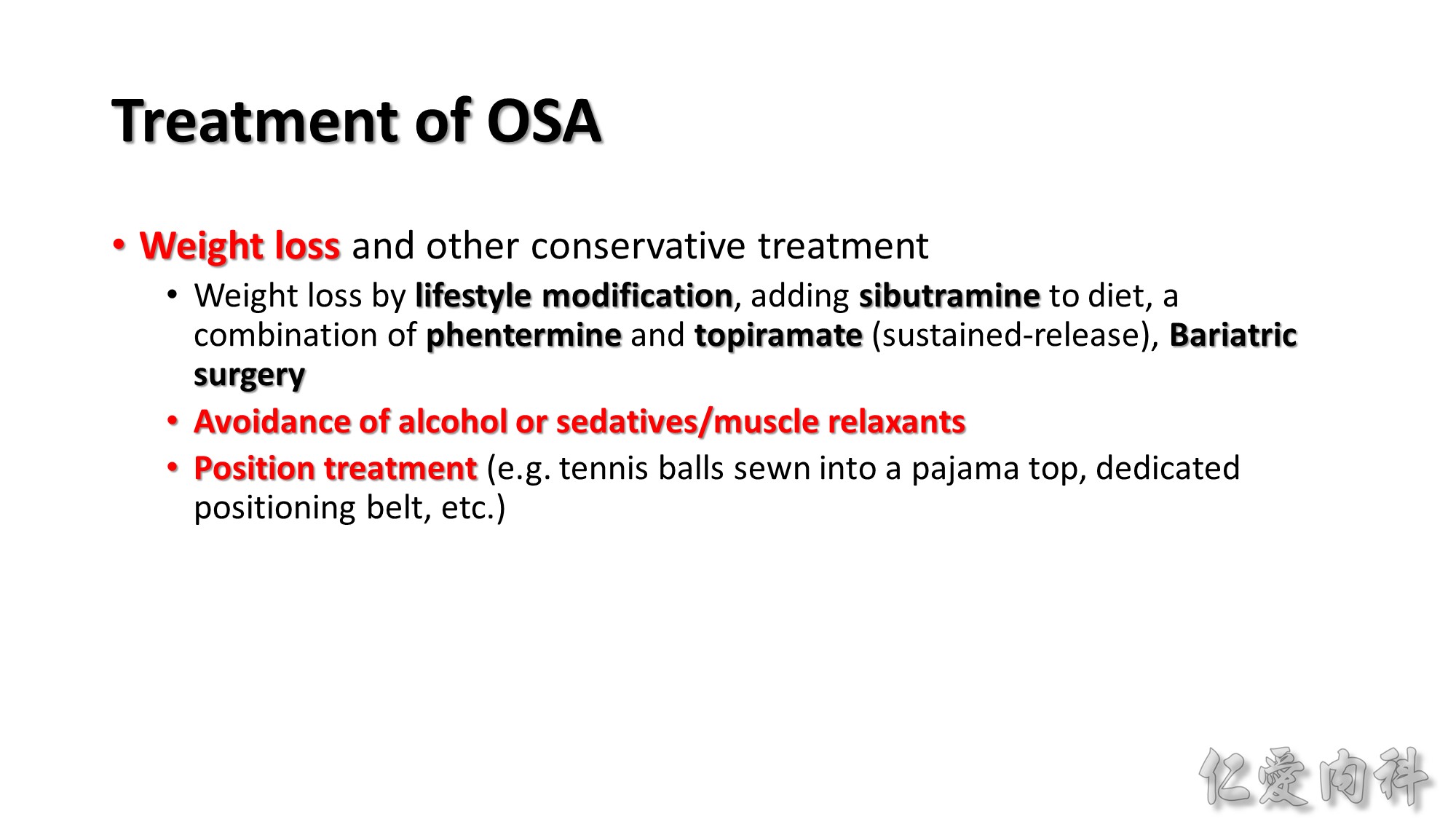
In OSA patients with venous insufficiency, the use of compression stockings to prevent daytime fluid accumulation in the legs was associated with a significant reduction in nocturnal fluid shift and in AHI. Consideration should therefore be given to this approach in managing OSA among older sedentary patients with venous insufficiency.
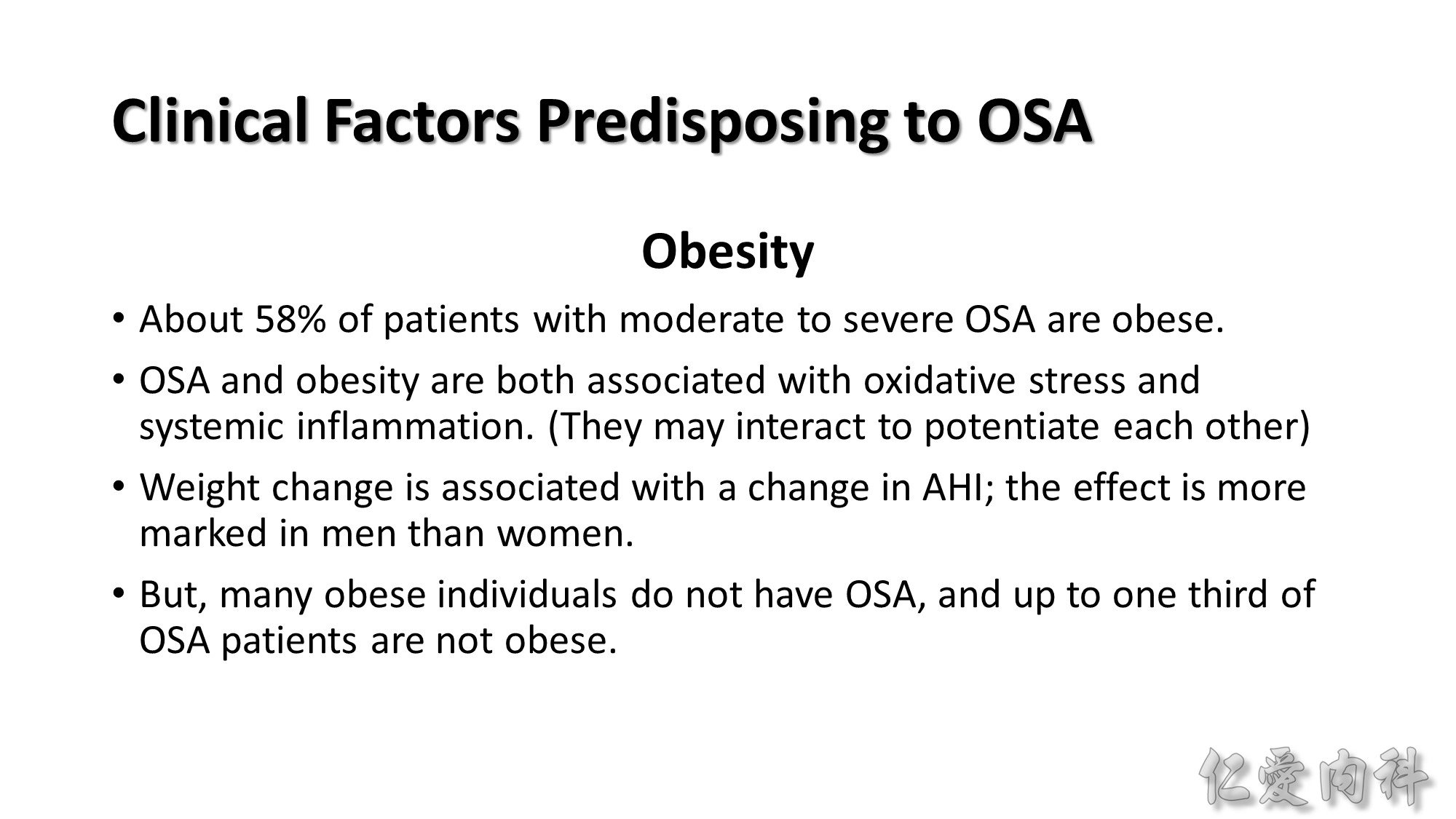
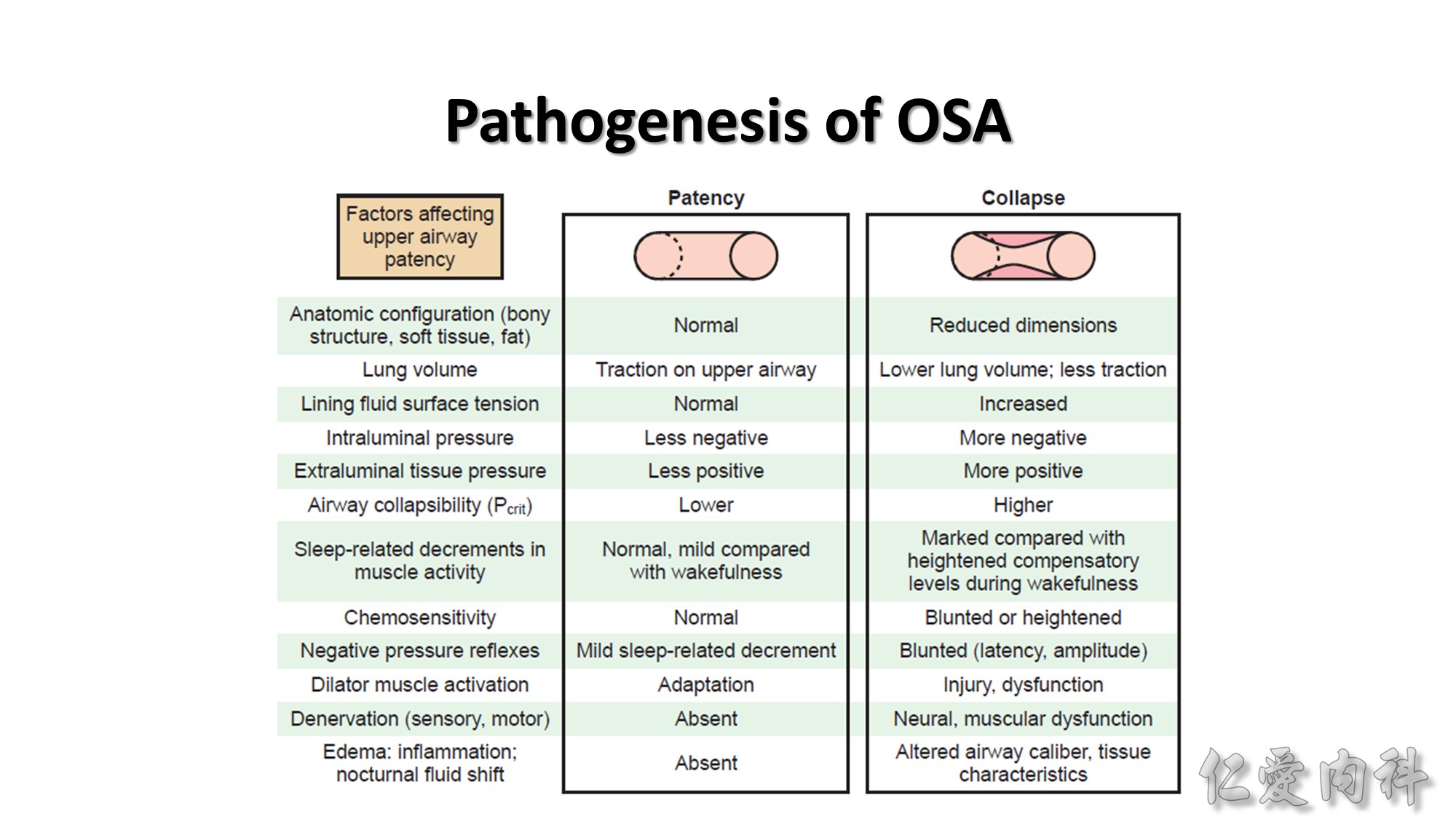
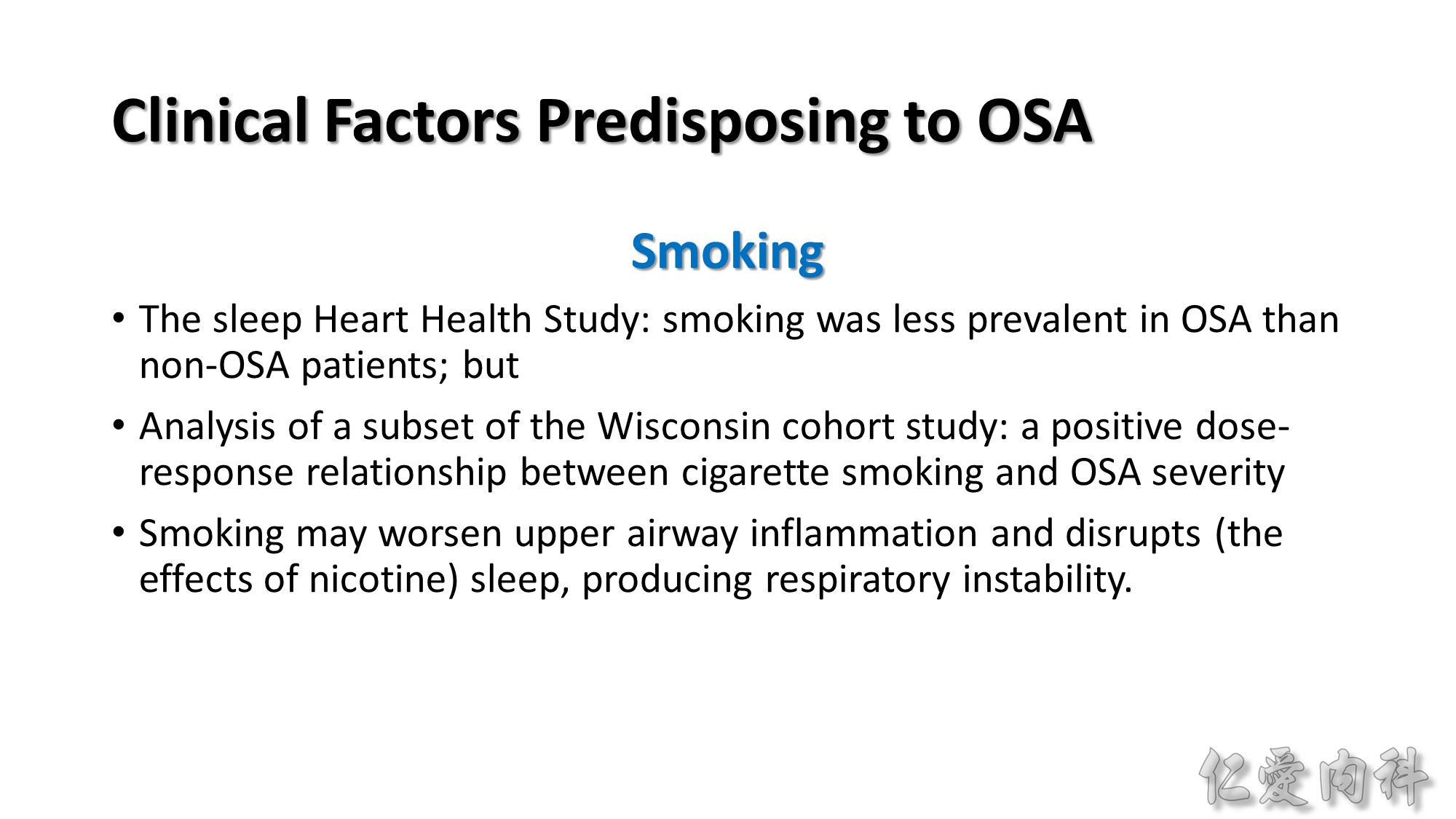
In the Wisconsin cohort over 8 years’ follow-up, a 10% increase in body weight was associated with a 32% increase in AHI and a sixfold increase in risk for developing an AHI of 15 or higher. A 10% weight loss was associated with a 26% reduction in AHI.
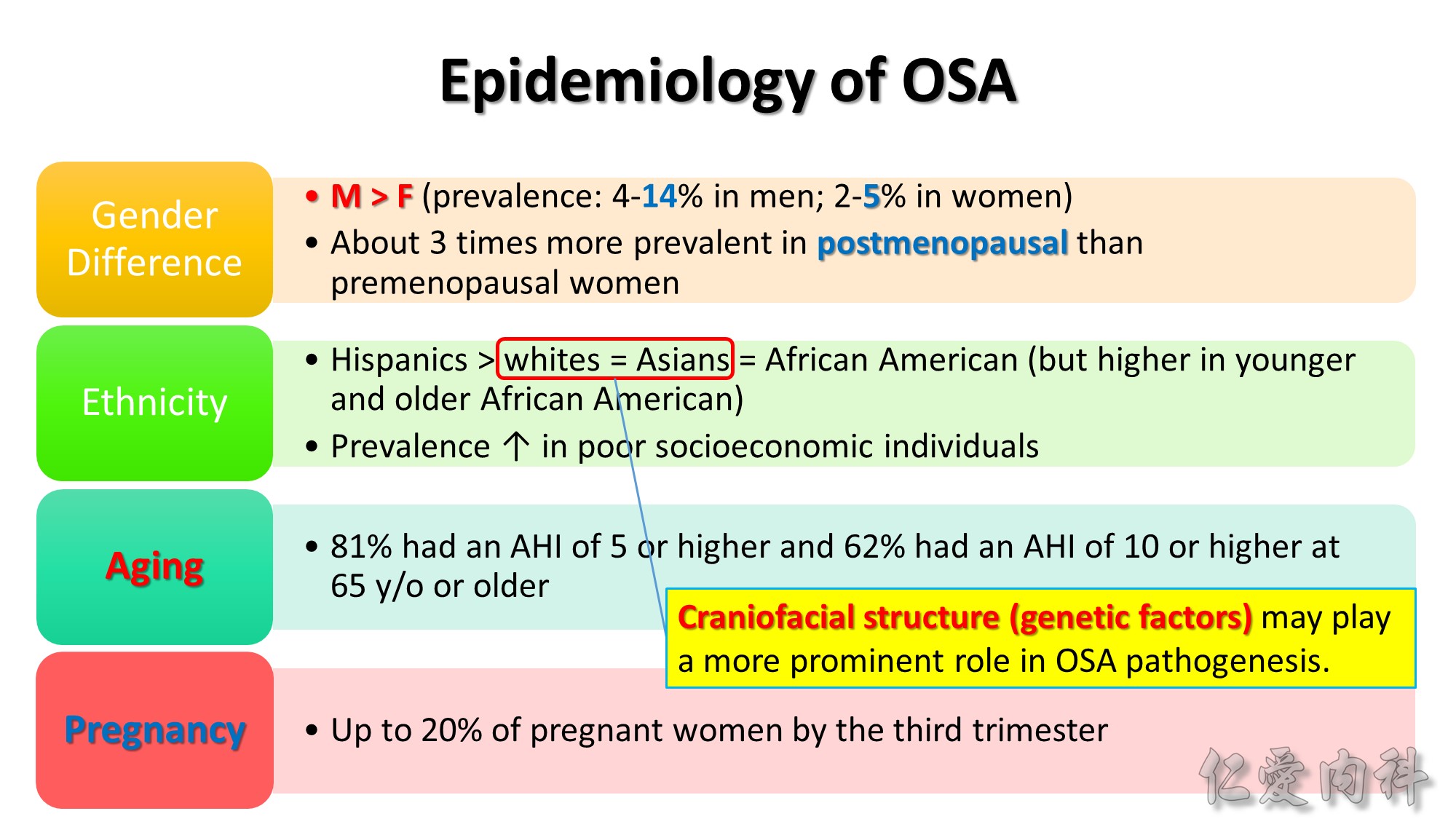
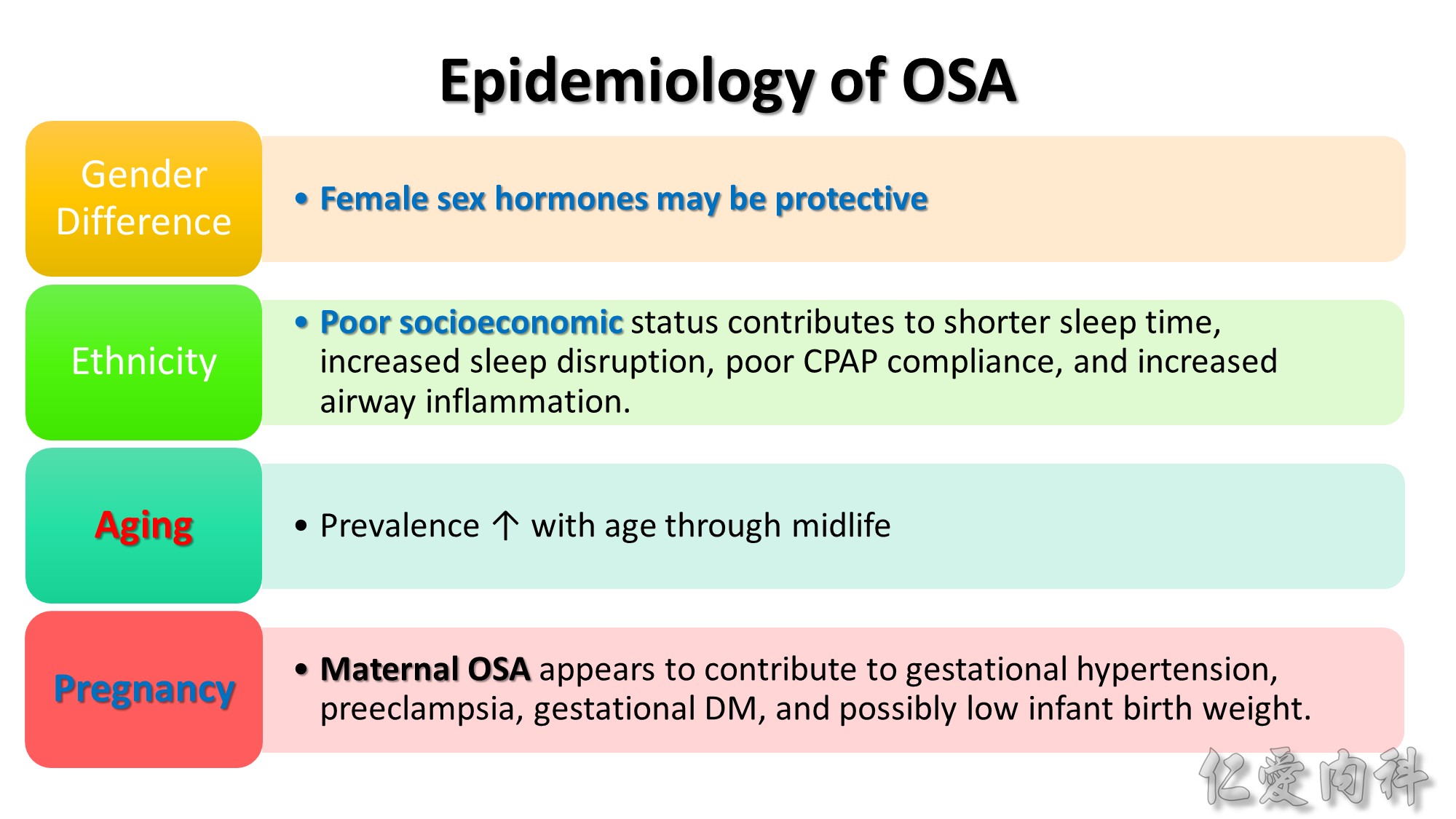
Female sex hormones may be protective; but hormone replacement appears to have little impact on OSA once present.
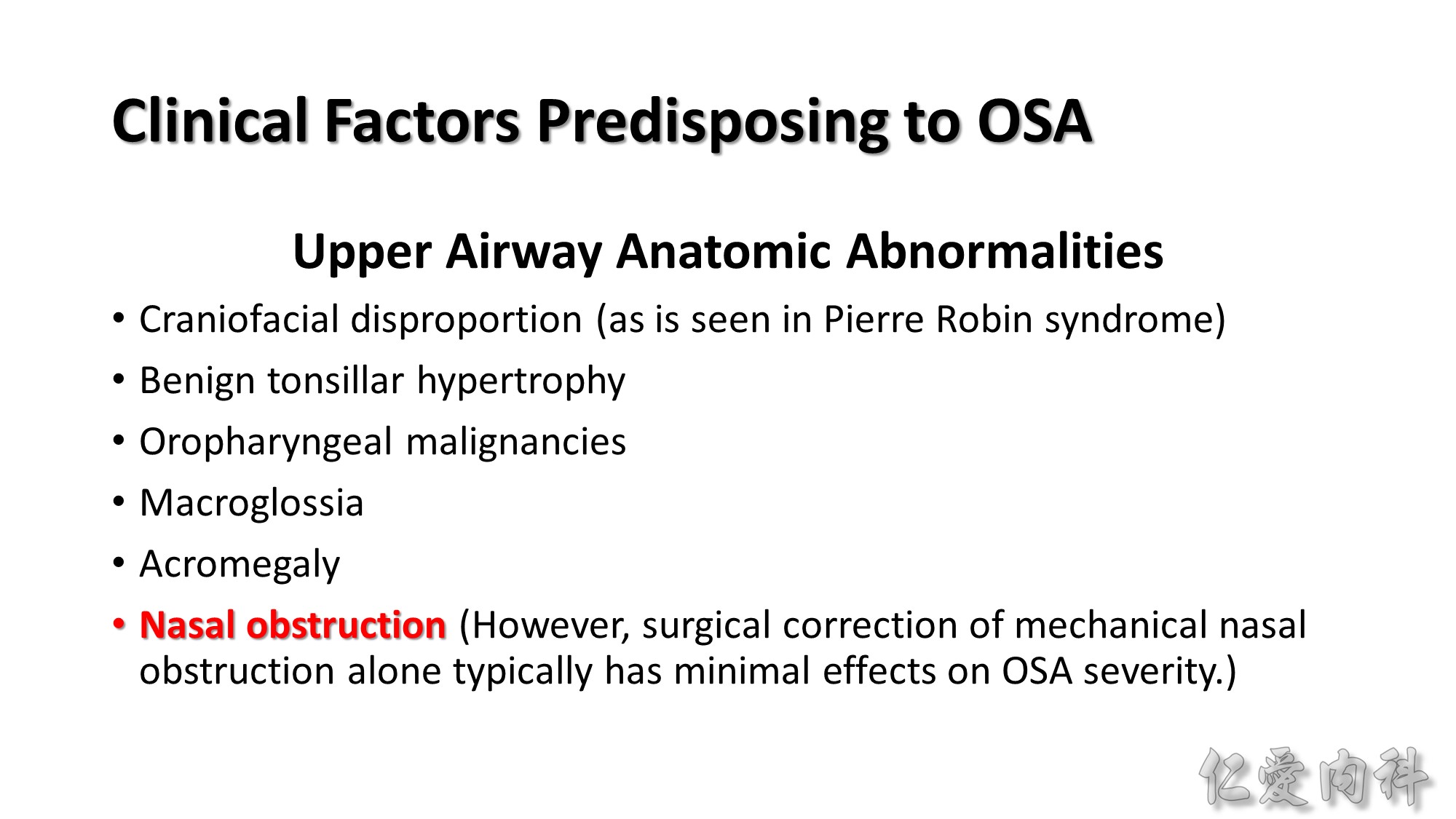
OSA prevalence in Asians is comparable to whites, despite a lower prevalence of obesity among Asians. Although obesity remains a important risk factor for OSA among Asians, craniofacial structure may play a more prominent role in OSA pathogenesis.
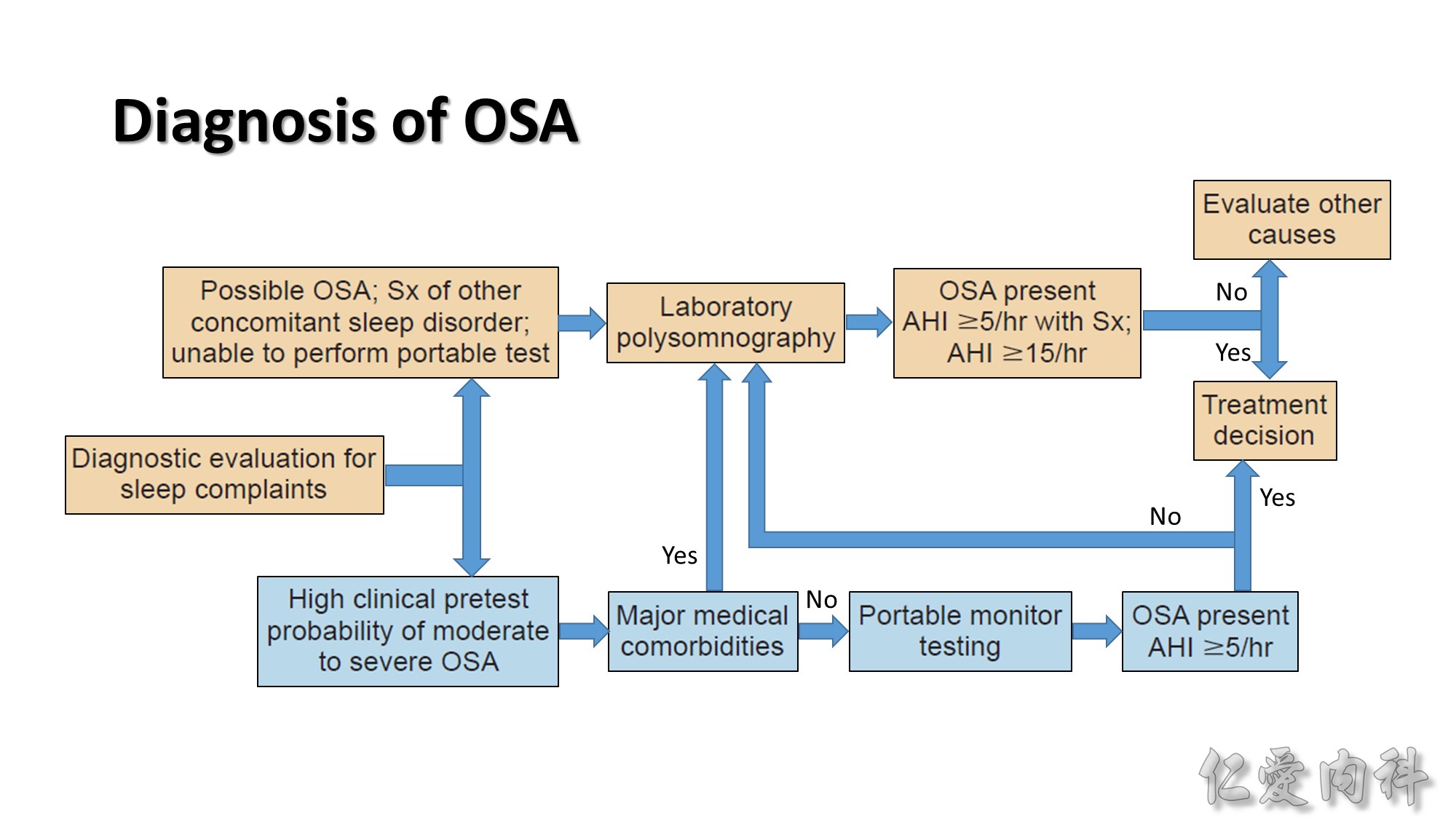
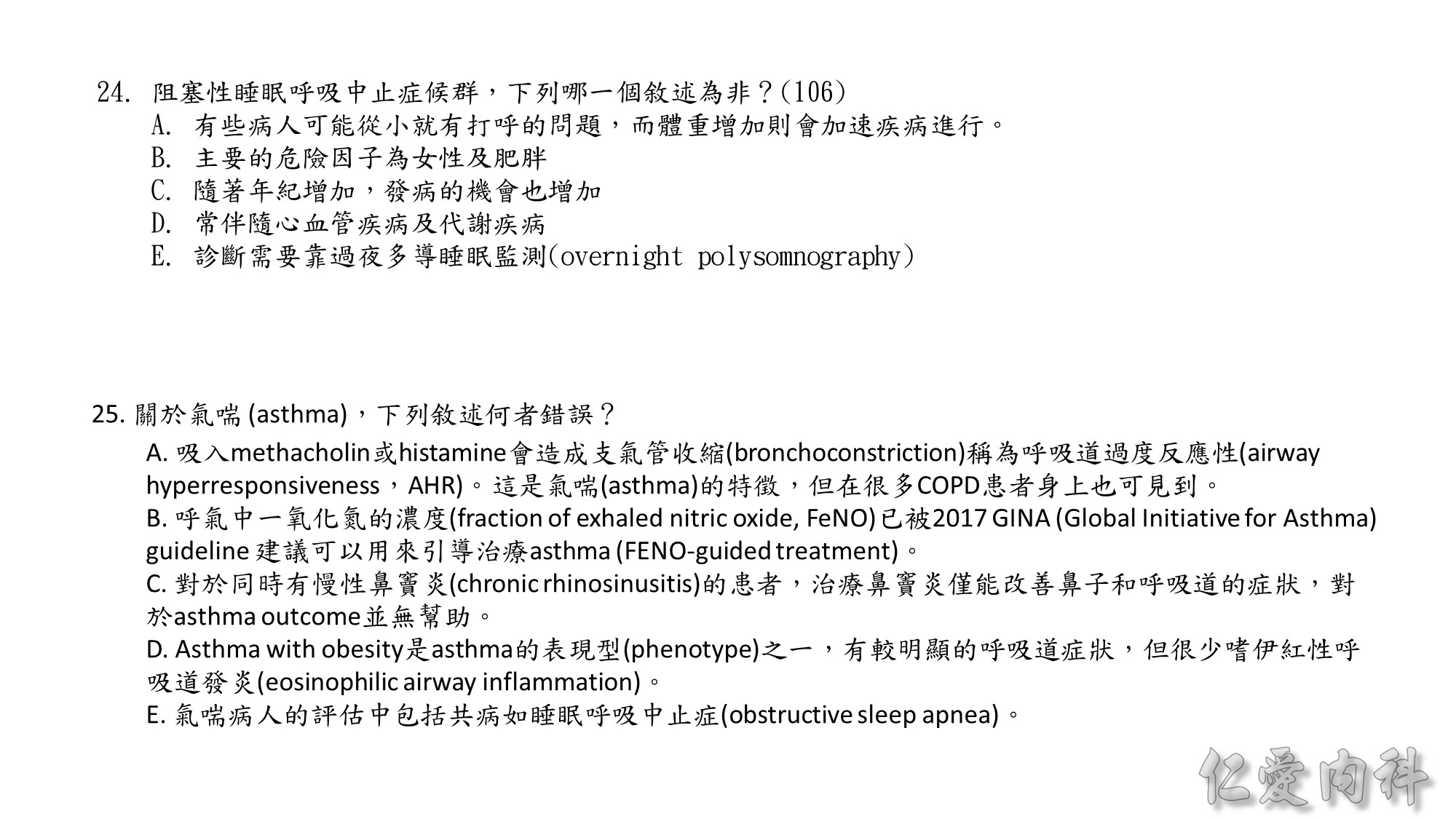
Several questionnaires such as the Berlin and Stop-BANG questionnaires have been developed to grade OSA risk. But objective sleep recording is required to establish a diagnosis of OSA.
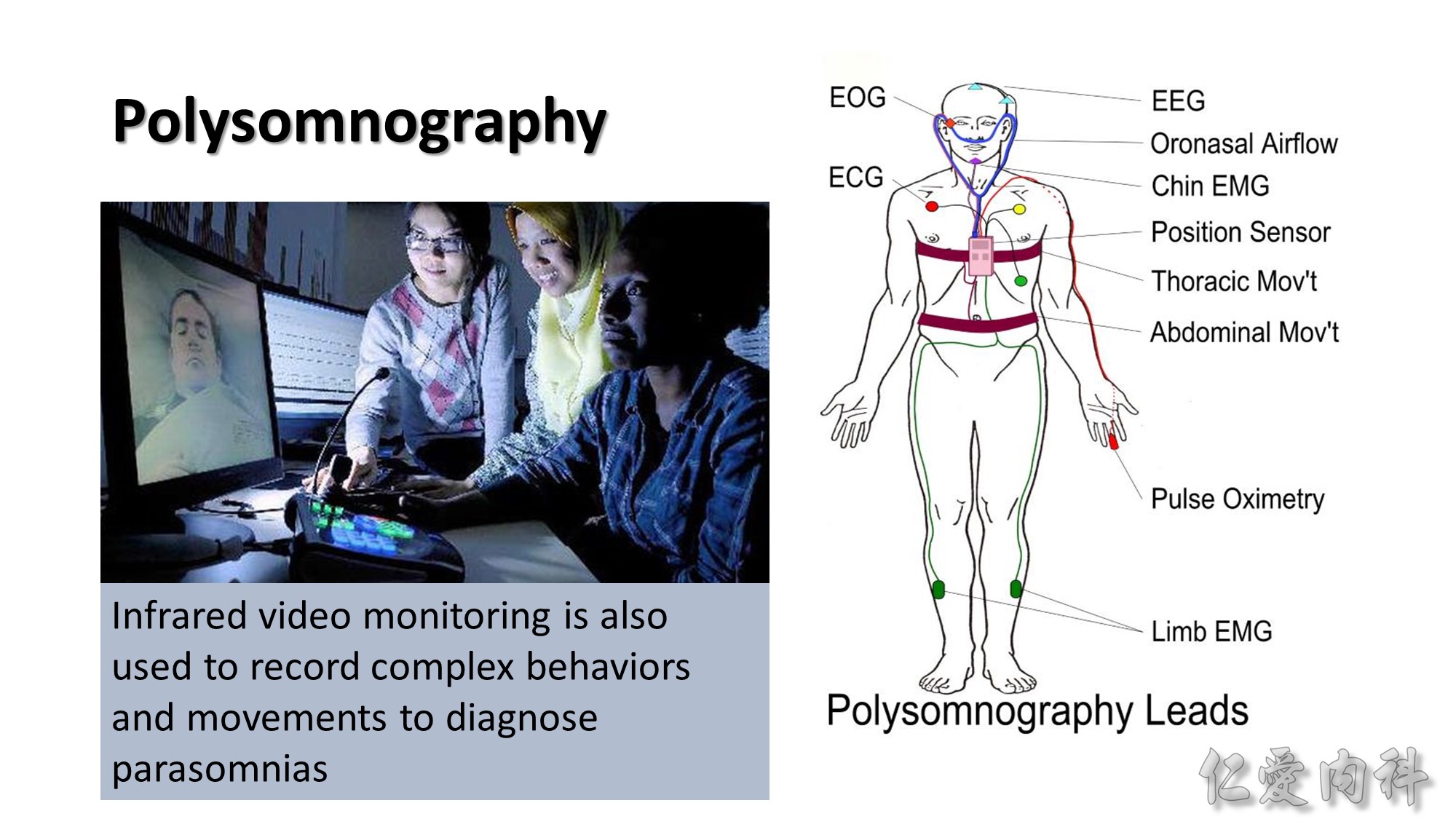
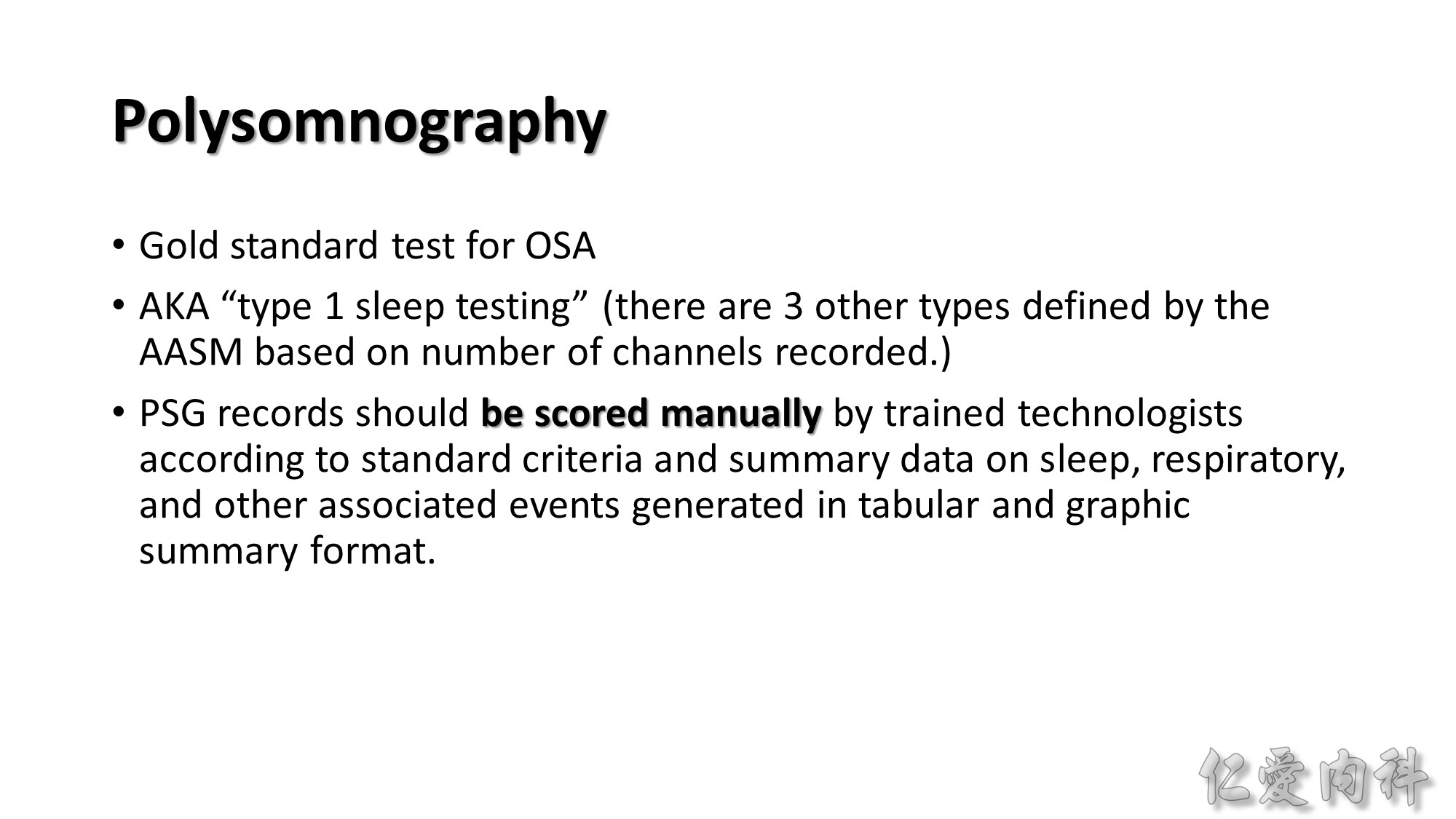
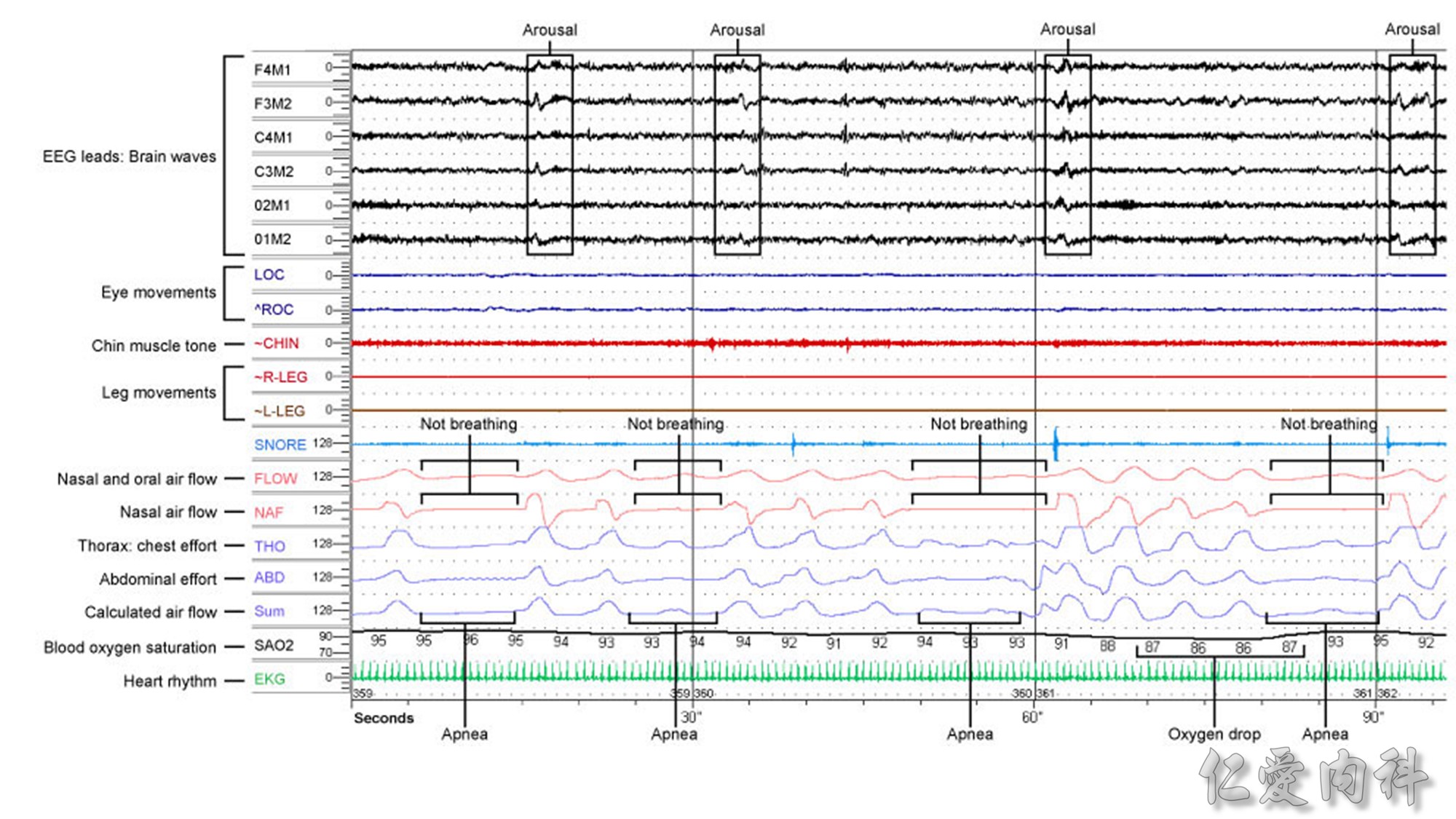
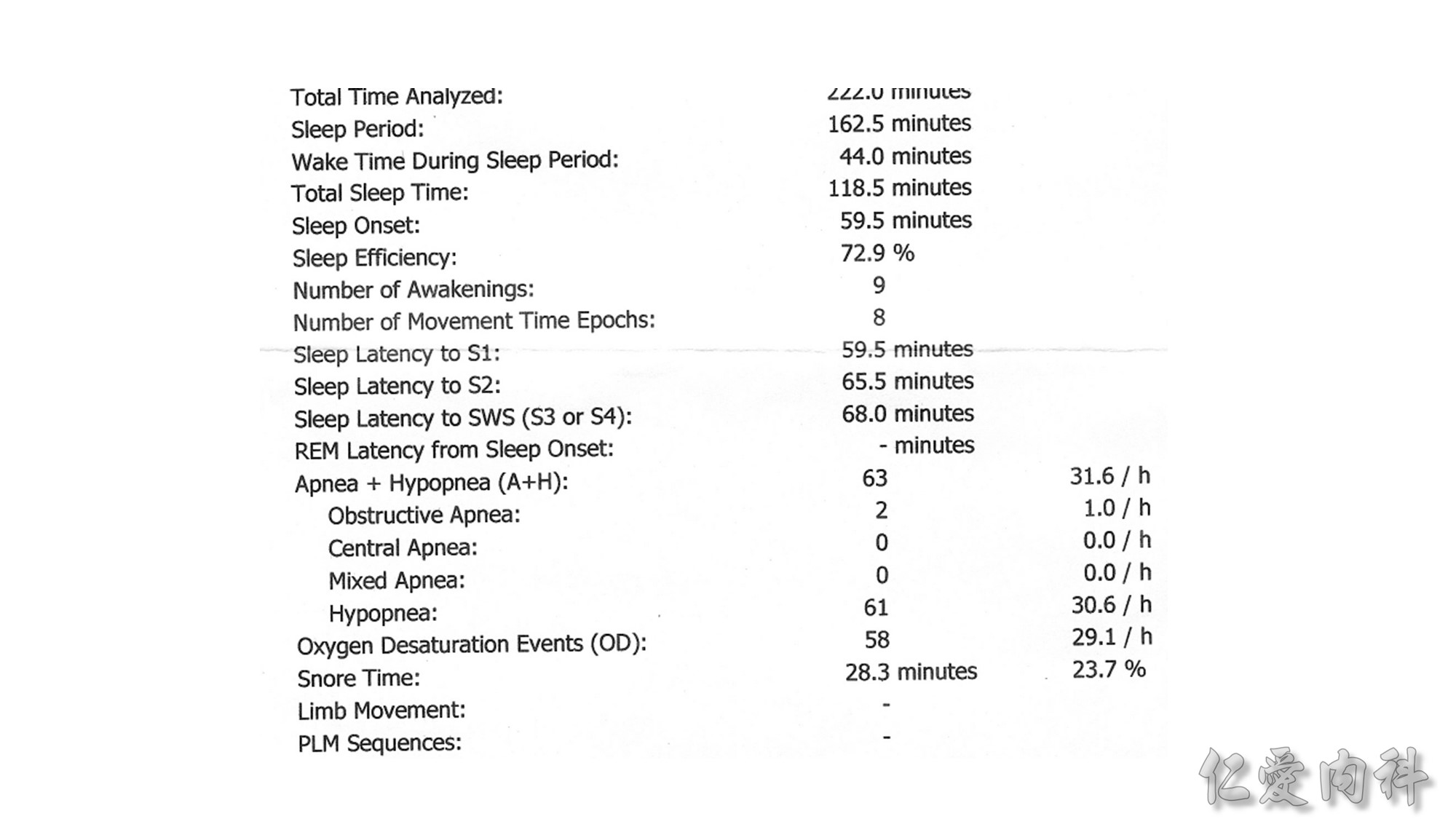
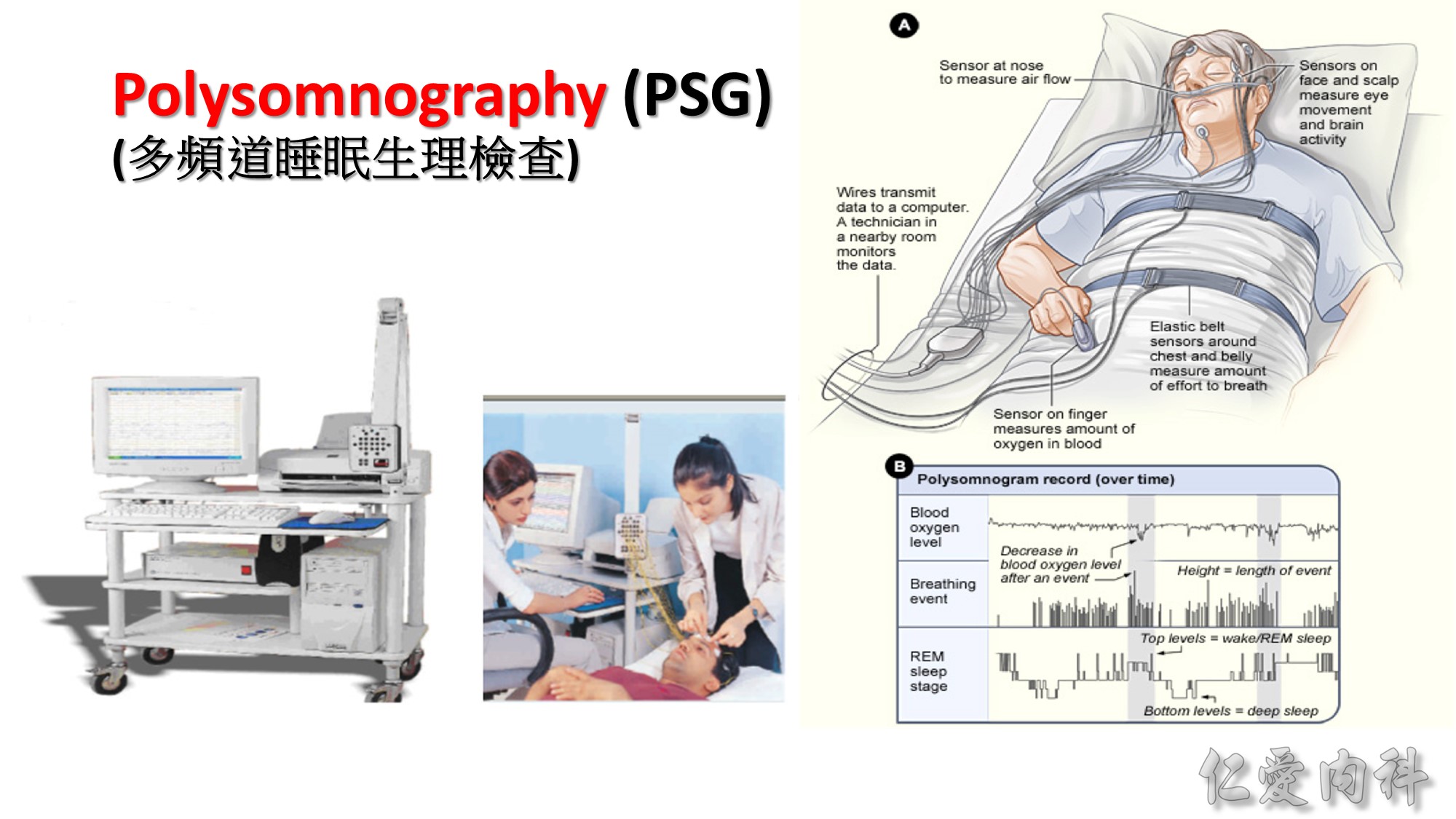
PSG應有的正式報告
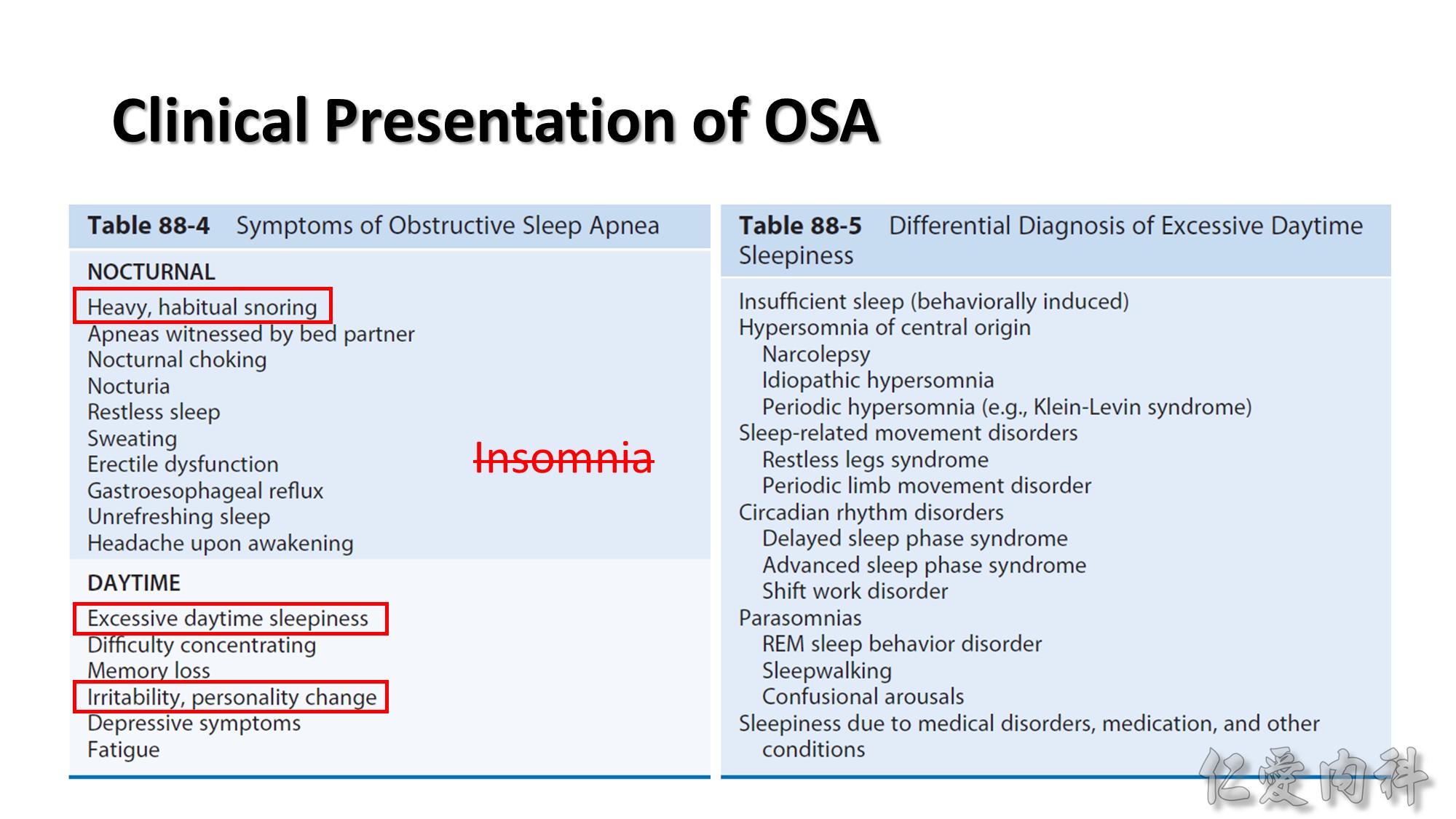
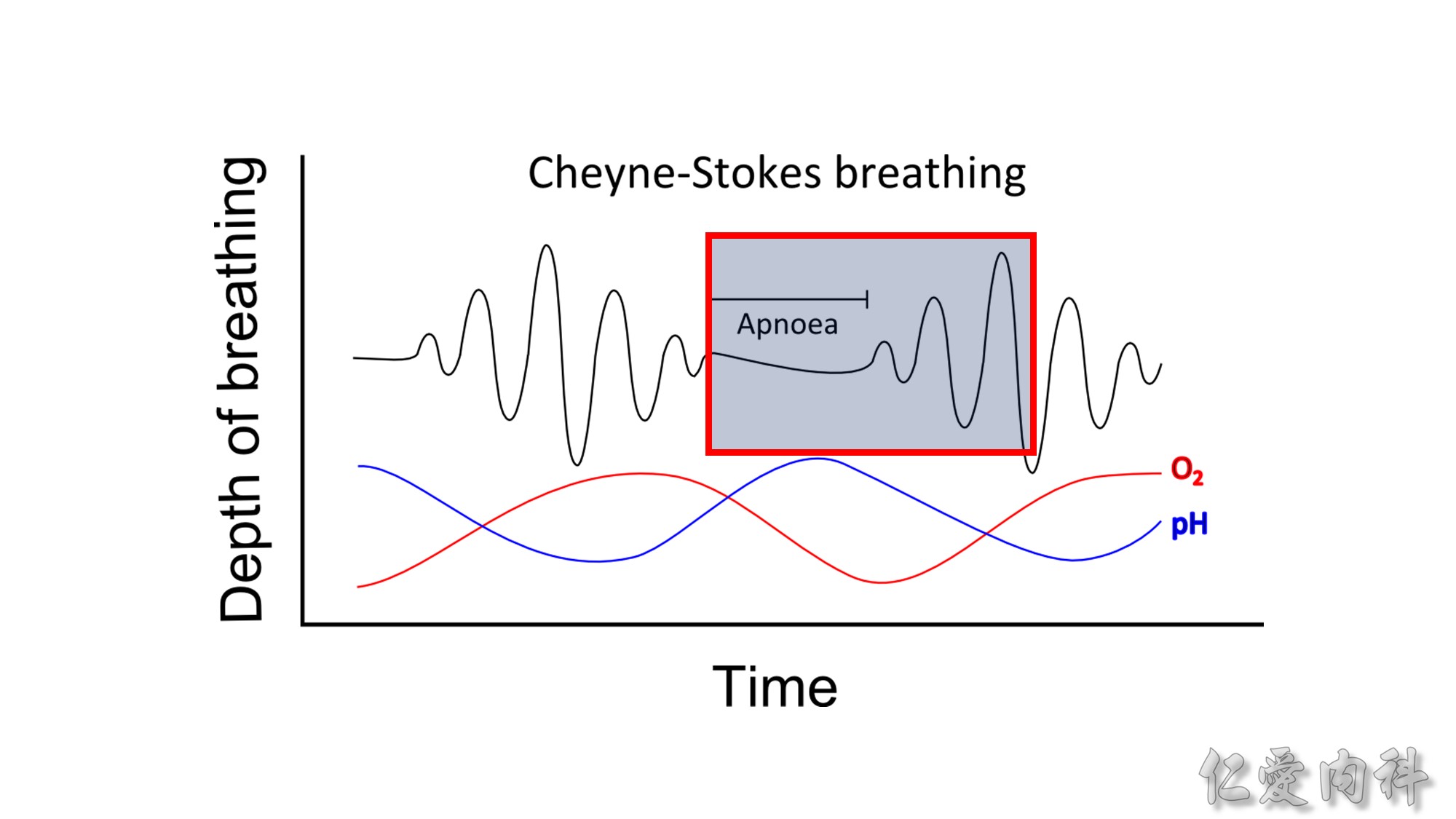
The differential diagnosis for nocturnal choking includes paroxysmal nocturnal dyspnea related to heart failure and Cheyne-Stokes respiration, nocturnal asthma, laryngospasm (idiopathic or due to acid pepsin reflux), orthopnea due to diaphragm dysfuncion, or insular cortical seizures.
Morning headache may be present, which may be associated with nocturnal hypercapnia due to concomitant obesity hypoventilation.
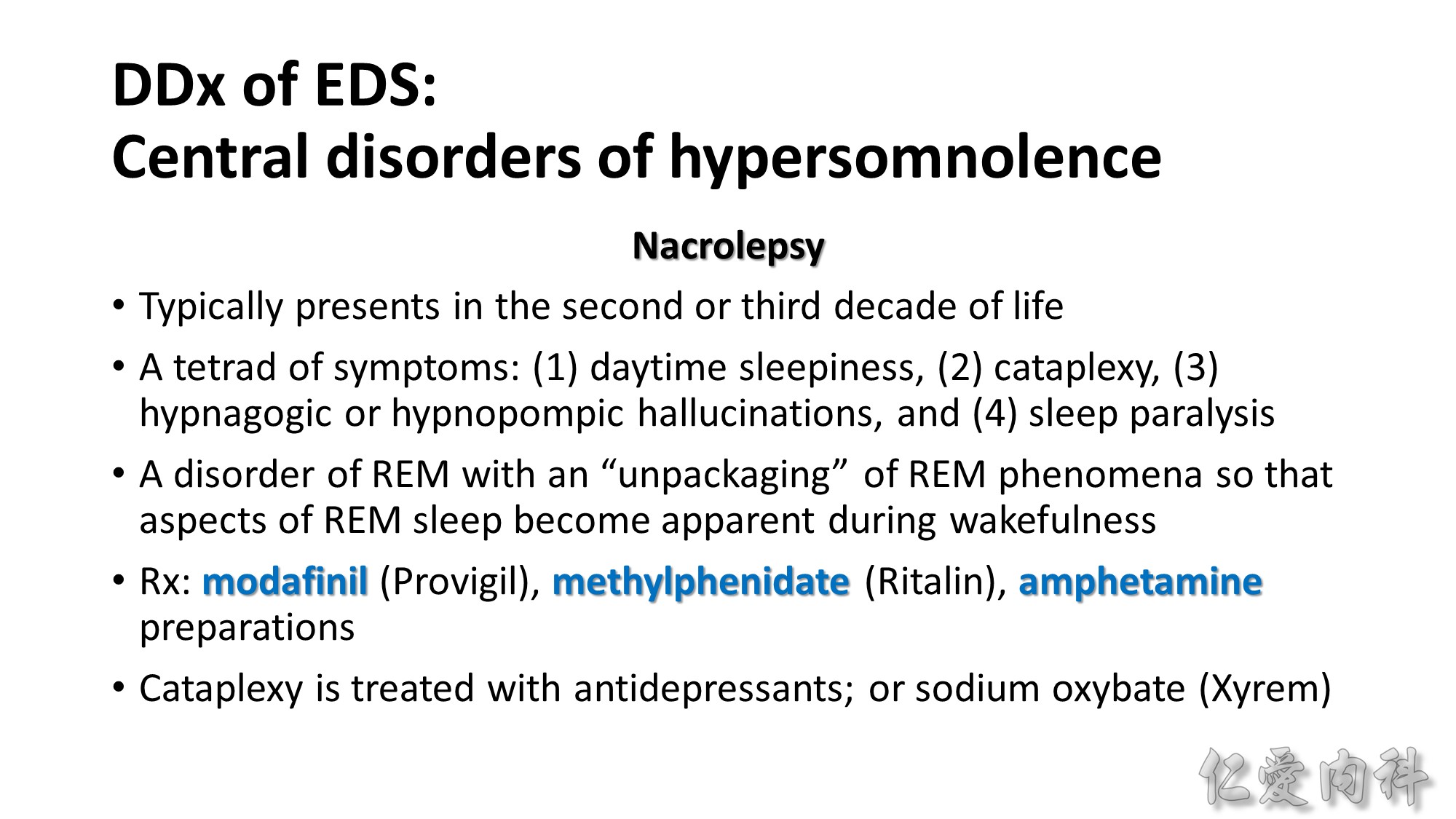
Cataplexy: a sudden loss of muscle tone, as takes place in REM sleep, which is precipitated by emotion (laughter, anger, surprise) during wakefulness. It is a virtually pathognomonic symptom, although narcolepsy can be seen without cataplexy. It is associated with objective transient areflexia and can mimic syncope.
Hypnagogic and hypnopompic hallucinations are vivid dreams typically with a strong visual component that are experienced either at sleep onset or when awakening from sleep.
Interventions to shift the biologic clock, such as administration of melatonin in the evening and exposure to bright light in the morning
- Application of nasal CPAP to treat OSA restores sleep continuity and may be associated acutely with a rebound increase in N3 (slow-wave) and stage R (REM) sleep, which patients perceive as improved sleep quality.
- Individuals with EDS should be warned of the dangers of driving before treatment, undergo diagnostic sleep testing within 1 months, and start CPAP treatment following a positive diagnostic test. (several studies have shown a high prevalence of OSA among commercial drivers.) Screening for OSA is recommended as part of the general medical evaluation for commercial drivers.
- Depression may worsen symptoms of sleepiness and fatigue in OSA. Some studies report improvement in depression scores with OSA treatment.
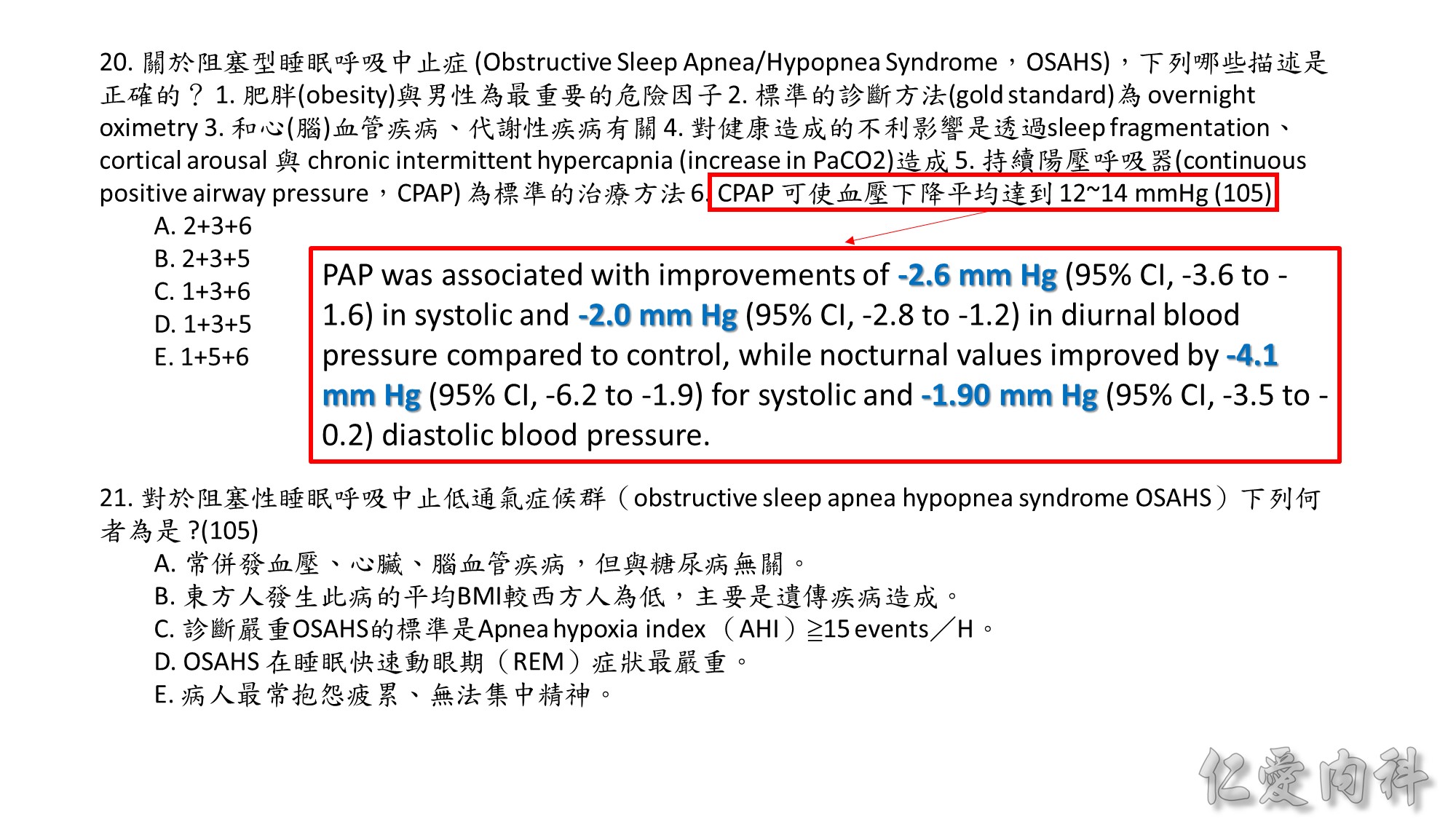
- PAP treatment improves hypertension. PAP was associated with improvements of -2.6 mm Hg (95% CI, -3.6 to -1.6) in systolic and -2.0 mm Hg (95% CI, -2.8 to -1.2) in diurnal blood pressure compared to control, while nocturnal values improved by -4.1 mm Hg (95% CI, -6.2 to -1.9) for systolic and -1.90 mm Hg (95% CI, -3.5 to -0.2).
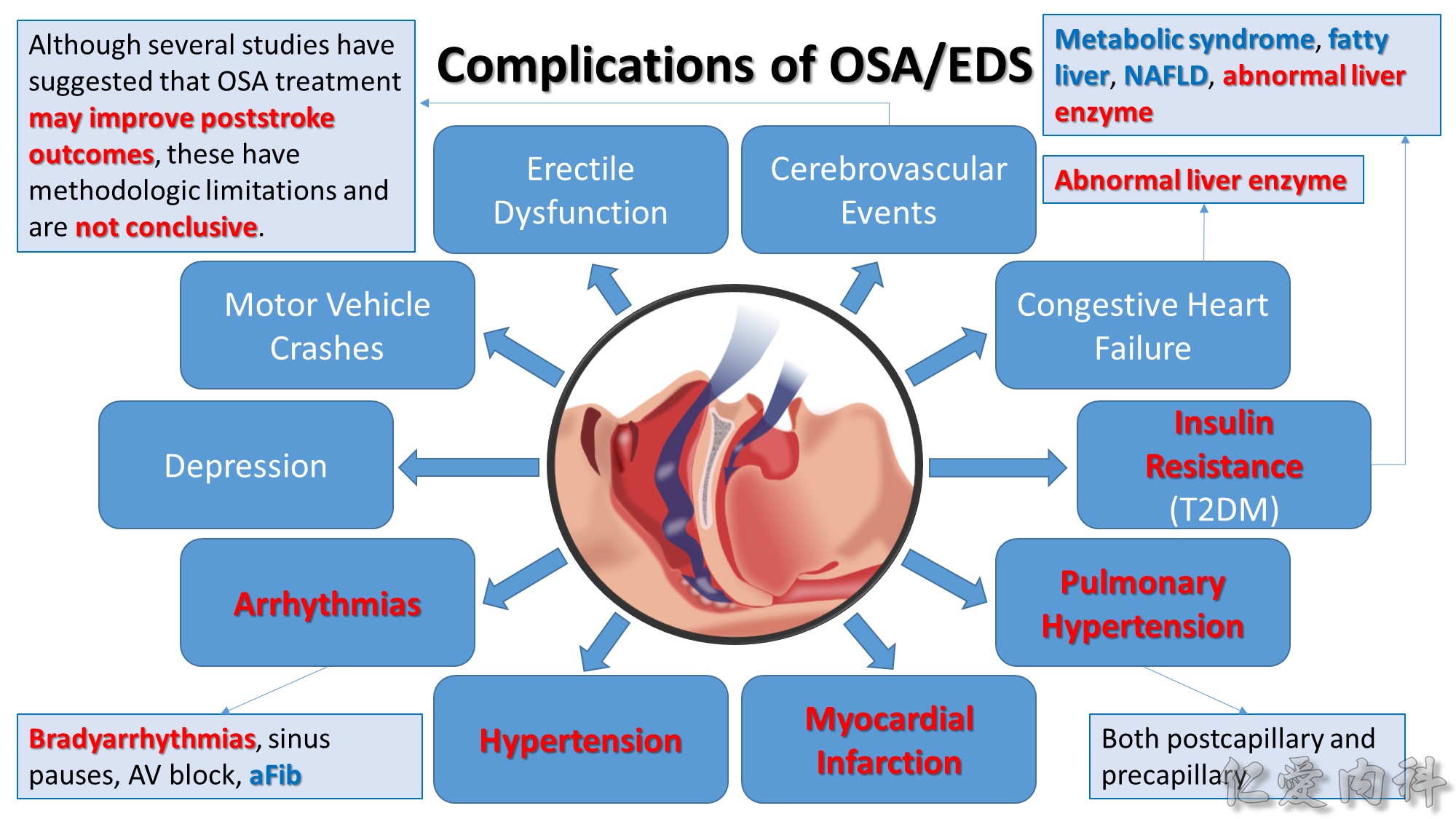
- Arrhythmias: bradyarrhythmias, including sinus pauses and atrioventricular block; atrial fibrillation; evaluation for OSA and, if present, institution of treatment should be considered in patients with atrial fibrillation.
- In observational studies, coronary patients who accepted OSA treatment suffered fewer subsequent cardiovascular events than those who declined. (However, refusal of CPAP may be a marker of poor health behavior that could also adversely affect outcomes.)
- OSA is reported to be prevalent among patients who have suffered acute myocardial infarction and, if present, OSA is associated with worse cardiovascular outcomes.
- The recently published Multicentre Obstructive Sleep Apnoea Interventional Cardiovascular (MOSAIC) trial evaluated the effects of CPAP compared to control on reduction of a surrogate cardiovascular risk score and found that calculated risk was not significantly reduced. However, CPAP was associated with a significant improvement in endothelial function in a subgroup of MOSAIC subjects. Follow-up of MOSAIC subjects for long-term “hard” cardiovascular outcomes may yield additional findings.
- A recent randomized trial by the Spanish collaborative group showed no significant difference over 7 years in the incidence of cardiovascular events and hypertension in CPAP-treated compared to control groups. However, there was a significant reduction in events for patients compliant with CPAP for 4 or more hours per night (incidence density ratio, 0.7 [95% CI, 0.5 to 0.9]compared with control group).
- Although stroke may also in turn produce or worsen sleep-disordered breathing, studies suggest that in many cases OSA preceded the stroke.
- Although several studies have suggested that OSA treatment may improve poststroke outcomes, these have methodologic limitations and are not conclusive.
- A recent meta-analysis of six studies evaluating the effects of OSA treatment on left ventricular function showed a significant mean improvement in left ventricular ejection fraction of 5.2% (95% CI, 3.3% to 7.1%).
- Early studies in severe OSA patients showed that pulmonary artery pressure can improve substantially following tracheostomy but may not normalize.
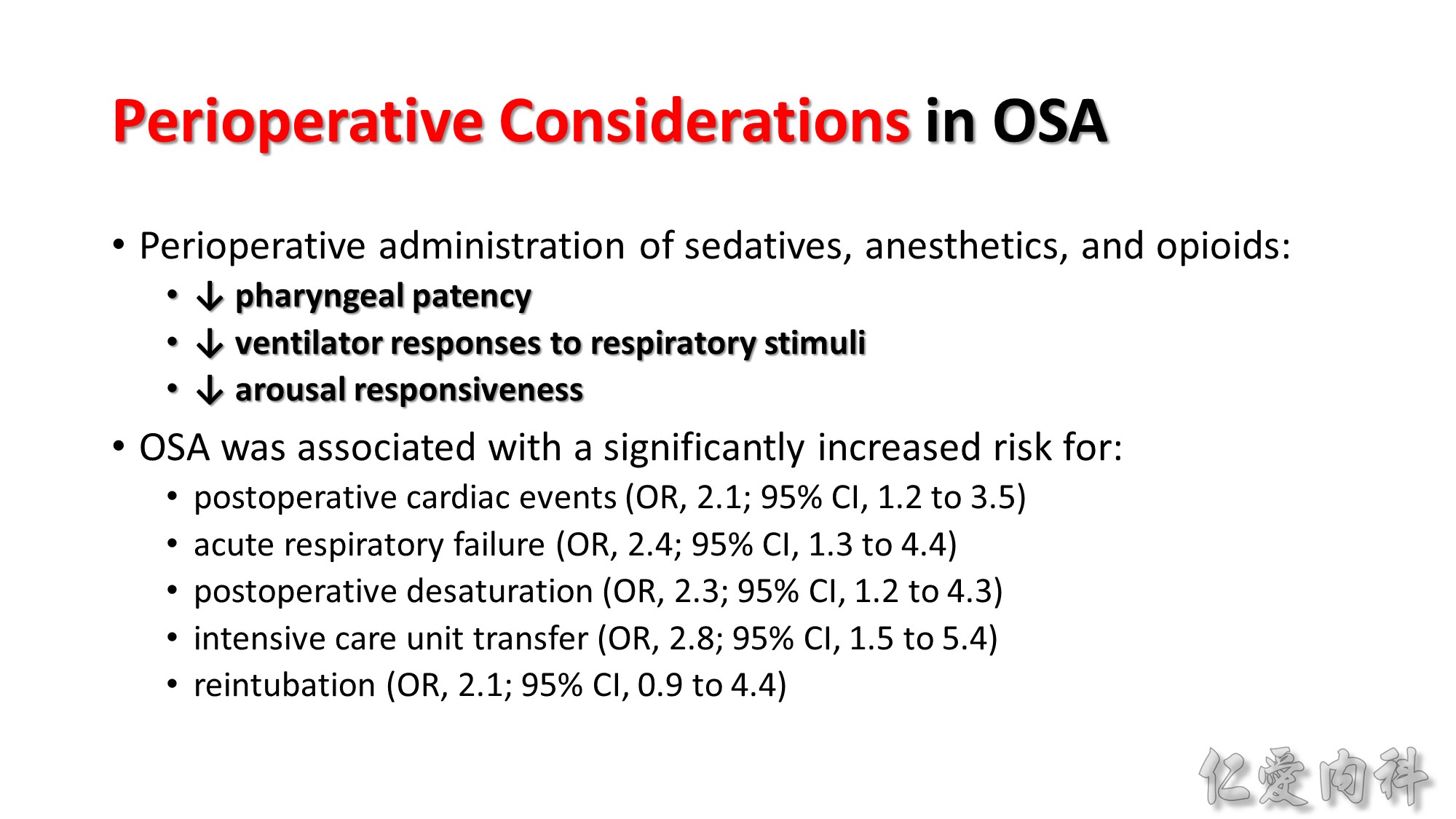
OSA is associated with an increased risk for perioperative complications. OSA treatment should be started before elective surgery when possible; patietns with known or suspected untreated OSA undergoing emergency surgery should be monitored closely in the post operative period.
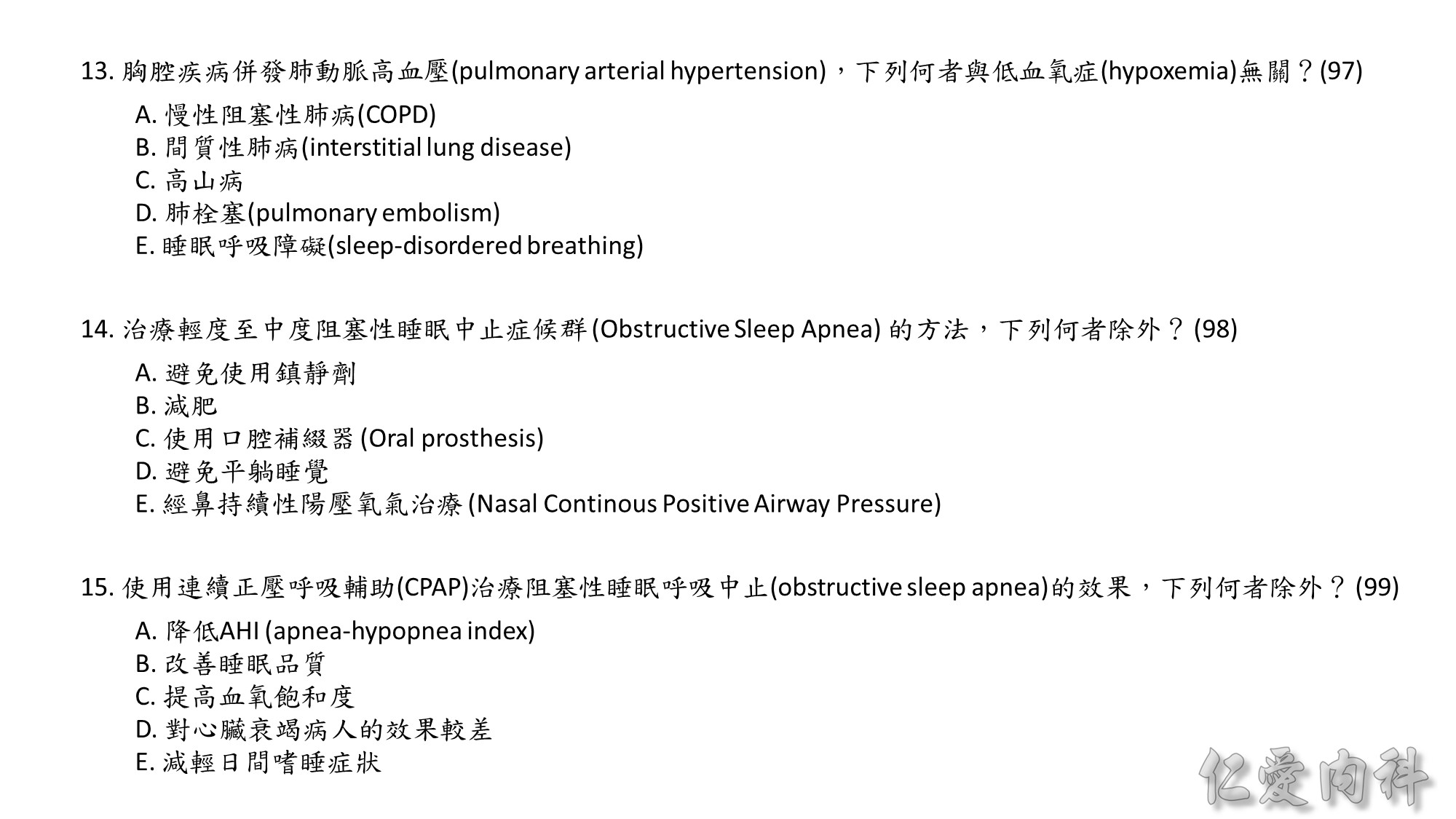
98 (E)